Digital temperature measurement in the rectum is still considered suitable to detect fever in intensive-care patients. Rectal measurement can spread infections (1), may damage the rectal mucous membrane, is contraindicated after rectal surgery, can be perceived as uncomfortable and is resource-intensive, since the procedure requires the patient to be turned over. Infrared temperature measurement in the ear was therefore welcomed in the 1990s, although intensive-care wards had reservations about the method (2). In 1997, the Norwegian Board of Health Supervision stated that «in situations in which an accurate measurement of body temperature is clinically essential, it is recommended to undertake the measurement with the aid of rectal, electronic contact thermometry» (3). Recently, infrared measurement in the temporal artery region has been introduced. The device, which is also referred to as a temporal scanner, selects the highest value from several thousands of measurements per second, which are undertaken when the small, hand-held device (Figure 1) is passed over the temporal region. The probe must have contact with the skin. In adults, a control measurement is also undertaken over the mastoid process. Ideally, the highest value should be reached when the probe passes over the superficial temporal artery, and the device calculates the core temperature from the surrounding temperature and the temperature of the skin over the artery (4). We wished to test the ability of this device to detect a fever.

Figure 1 Use of an infrared device for measuring temporal artery temperature
Material and method
During two periods in 2002, adult (≥ 18 years) patients (n = 164) who were admitted to the intensive-care ward had their temperature measured with both a rectal thermometer (Terumo C402) and an infrared temporal artery thermometer (Exergen Temporal Scanner #TAT-4000). The measurements were undertaken by nurses who had undergone practical training in the use of the device, with the aid of a specially prepared manual with photographs placed with the thermometers, and by following the guidelines in the department’s procedures manual. All the department’s nurses participated. The department has 50 full-time nursing positions divided among approximately 60 persons, including highly skilled specialist nurses and recently graduated, state registered nurses. Values were entered in an Excel spreadsheet for estimates and auto-filter searches. Fisher’s exact test, with estimation of sensitivity and specificity, was made in InStat, and the Bland-Altman plot was prepared in PRISM (both from GraphPad Software, CA, USA). We used a 5 % significance level and two-tailed tests.
Results
On average, the temporal artery measurement was 0.3 °C lower than the temperature measured in the rectum. The difference between the two methods of measurement is shown in a Bland-Altman plot in Figure 2 (5). Cases of fever, defined as a rectal temperature of ≥ 38 °C (n = 70), were detected by the temporal scanner in 37 patients. This gave the scanner a sensitivity to detect fever of 53 % (95 % CI: 41 – 65 %) and a specificity of 96 % (95 % CI: 90 – 99 %). The positive predictive value was 90 % (95 % CI: 77 – 97 %) and the negative predictive value was 73 % (95 % CI: 64 – 81 %). The p-value was < 0.0001.
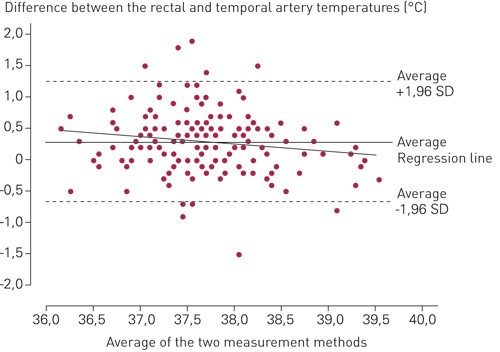
Figure 2 Agreement between the averages of the temperature measurements undertaken temporally and rectally (the x-axis) and the difference between the rectal and temporal artery measurements (the y-axis). The advantages of this presentation form are described in more detail by Bland and Altman (5)
Discussion
Per Valle and collaborators found that infrared temperature measurements in the ear were 0.5 °C lower than when measured in the rectum. Measurements with mercury thermometers and electronic rectal measurement devices yielded nearly identical results. The sensitivity to detect fever with an infrared temperature measurement in the ear was only 30 % (6). Our findings from the use of infrared temporal artery measurements are somewhat better, with a sensitivity of 53 %, and thus approximately equal to the results from the ear-temperature study at Akershus University Hospital (2), but this means that only slightly more than half of all febrile patients are identified by the temporal scanner. A negative predictive value of 73 % means that approximately one in every four adult intensive-care patients indicated as afebrile by the temporal scanner in fact has a fever. On the other hand, the temporal scanner detects few false-positive fever conditions.
In comparison, Banitabeli and Bangstad found a 71 % sensitivity to detection of fever by infrared temperature measurement in the ear in children (7). Greenes and collaborators found that the temporal scanner had a 66 % sensitivity to detection of rectal fever ≥ 38 °C in 308 children aged under one year (8). Suleman and collaborators, however, found a poor correspondence between infrared temporal temperature measurement and measurements undertaken in the bladder and the pulmonary artery in children and adults on a heart-lung machine (9). In this study as well, the best sensitivity (84 %) to detection of a fever (≥ 37.8 °C) was found in children. In adults (n = 30) the temporal measurements were on average 1.3 °C below the temperature of the pulmonalis, and the sensitivity to detection of fever was 0 % (9).
Why does there seem to be a better correspondence between the core temperature and the infrared temporal artery measurement in children? Suleman and collaborators raised the question of whether the relatively thicker skin in adults isolated the pulmonary artery, whether the thicker cranium and muscles better retained the heat from the brain, which in small children probably contributes to the skin temperature in the temporal region, whether atherosclerotic changes in the pulmonary artery in older people reduces the flow of blood, and finally whether larger concentrations of catecholamines in adults result in cutaneous vasoconstriction and hence a lower temperature (9). We could also imagine that variations in the anatomical pathway of the pulmonary artery may play a role (10). This would apply to a larger degree to adults, since hair may come between the probe and the artery if the probe is passed as close to the cranium as recommended by the manufacturer.
Conclusion
The most important function of a temperature measurement is to detect fever. If rectal measurement is to remain the gold standard, infrared measurement over the temporal region has too low sensitivity (53 %) to detect fever in adults admitted to an intensive-care ward.