During the last 20 years, there has been an ever-increasing development of acute treatment, rehabilitation and secondary stroke prophylaxis. Diagnosis of the condition has improved with routine use of CT caput and establishment of separate stroke units in many places (1, 2). New medicines have been documented to efficiently prevent recurrence of stroke, and new treatment principles are being tested (3 - 9).However, new knowledge is not always applied in clinical practice. In Sweden, a national voluntary stroke register has been established to help improve knowledge on treatment and prognosis for stroke (10), and in Norway one is working to establish such a register. Asker and Bærum hospital has an internal stroke register and this article presents clinical findings (data on admission, status upon discharge and 7-years of follow-up) on patients admitted to that hospital with stroke during the two years 1994 and 95.
Material and method
All patients from Asker and Bærum who were hospitalised with acute stroke in 1994 or 1995 were included in the register. Bærum hospital had two separate stroke units; one ward for patients with recent strokes and one for training and rehabilitation of stroke patients. In 1995, the two municipalities (Asker and Bærum) had a population of 158 131. The stroke unit was part of the medical department and was under professional leadership by specialists in internal medicine and geriatrics. Organisation of the unit was based on cross-disciplinary cooperation with groups of physicians, nurses, assistant nurses, physiotherapists, occupational therapists, speech therapists and social workers worked working closely together on acute treatment and rehabilitation. If cerebral infarction occurred, a neurosurgeon was routinely contacted and consulted. Most patients in the register were treated in the stroke unit. When there were too many patients in the unit; some were occasionally placed in a ward for internal medicine.
Information was recorded for all patients who were hospitalised with stroke (ICD-9-code 431 - 436) as a main diagnosis or a subdiagnosis. 9ICD-9-codes comprise cerebral infarction, cerebral embolism, cerebral haemorrhage, subarachnoidal bleeding and subdural bleeding, but not epidural haematoma. 457 patients were identified, and of these the 421 who were living in Asker or Bærum were included in the register.
We recorded information on previous strokes and transitory ischemic attacks and risk factors for cerebral disease such as hypertension, symptom-giving arteriosclerosis (claudicatio intermittens, coronary disease and carotis stenosis), daily smoking, diabetes and atrial fibrillation. Clinical symptoms and neurological events were recorded according to a classification used by Oxfordshire Community Stroke Project (OCSP), where stroke is divided into four different syndromes based on localisation and extent (11 - 13).
The four stroke syndromes are:
POCS (posterior circulation syndrome) - posterior circulatory syndrome
LACS (lacunar circulation syndrome)
TACS (total anterior circulation syndrome
PACS (partial anterior circulation syndrome)
As a diagnostic tool, we used an algorithm requiring the examining physician to record whether the neurological event was one-sided, if applicable which side it was on and whether the localisation was related to face, arm/hand, nystagmus or dizziness. These results were treated and classified according to the OCSP-classification.
Blood pressure was recorded upon arrival and the first blood pressure was measured the day after arrival and at discharge. Values were recorded for Hb, leucocytes, trombocytes, glucose, sodium, potassium and CRP taken within two hours after hospitalisation. Medicines and the patients’ level of consciousness were recorded at arrival. Patients with a level of consciousness below 11 (according to the Glasgow coma scale [GSC]) were classified as somnolent and patients with a score lower than seven were classified as comatous. Previously diagnosed dementia was recorded. The results of previously taken, more recent or repeated CT caput examinations were also recorded. Depending on the outcome the following was recorded; the duration of the stay, hospital morbidity and medication upon arrival and discharge. Level of functioning at discharge was related to everyday activities and assessed through a cross-disciplinary integrated approach by a physician, a nurse, a physiotherapist and an occupational therapist. In addition to tests such as Scandinavian Stroke Score, Barthel Index and Minimal Mental Status (MMS), the assessment especially emphasised the patient’s ability to master daily activities at home.
Information on survival and mortality was retrieved from national population statistics (Statistics Norway) in January 2003. The prevalence of recurrent stroke after the primary stroke that led to inclusion in the register was followed up through January 2003 by review of diagnosis lists (from 1.1.1994 up to 1.1.1995) in the hospital’s database.
Survival is presented by a Kaplan/Meier plot. The difference between groups was analysed with a Cox Proportional Hazard model. A two-sided p-value < 0.05 was considered significant. Fischer’s exact test was used to compare outcomes for the two subgroups stroke and myocardial infarction.
Results
Risk factors
Table 1 gives an overview of the material by age group. Of 421 patients, 203 were women and 218 were men. 95 (23 %) patients had previously had stroke. The mean age for admission to hospital was 75 years. Upon admission, 140 (33 %)had felt hypertonia and 96 (23 %) smoked daily. 135 (32 %) had symptoms of general arteriosclerosis in the form of coronary disease, claudicatio or carotis stenosis, 52 (12 %) had diabetes mellitus (type I or II) and 84 (20 %) had atrial fibrillation. 103 (24 %) patients had none of these risk factors, 168 (40 %) had one and 150 (36 %) had two or more risk factors. It seemed as if most known risk factors for arteriosclerotic disease occurred more frequently among the younger, with an exception of atrial fibrillation that was more frequent among the oldest patients.
|
Table 1 Observed findings related to age groups
|
|
a) Age group (years)
|
20 - 65
|
|
65 - 75
|
|
75 - 85
|
|
> 85
|
|
Total
|
|
Number and percentage of patients
|
71 (17)
|
|
127 (30)
|
|
159 (38)
|
|
64 (15)
|
|
421 (100)
|
|
Mean age (years)
|
57
|
|
71
|
|
80
|
|
89
|
|
75
|
|
Men; Number (%)
|
47 (66)
|
|
74 (58)
|
|
84 (53)
|
|
13 (20)
|
|
218 (52)
|
|
Women; Number (%)
|
24 (34)
|
|
53 (42)
|
|
75 (47)
|
|
53 (80)
|
|
203 (48)
|
|
b)
|
No.
|
(%)
|
|
No.
|
(%)
|
|
No.
|
(%)
|
|
No.
|
(%)
|
|
No.
|
(%)
|
|
Previous TIA
|
6
|
(9)
|
|
13
|
(10)
|
|
20
|
(13)
|
|
3
|
(5)
|
|
42
|
(10)
|
|
Previous stroke
|
13
|
(18)
|
|
38
|
(30)
|
|
32
|
(20)
|
|
14
|
(22)
|
|
95
|
(23)
|
|
Hypertension
|
30
|
(42)
|
|
52
|
(4)
|
|
42
|
(26)
|
|
16
|
(25)
|
|
140
|
(33)
|
|
Arteriosclerotic disease
|
13
|
(18)
|
|
46
|
(36)
|
|
54
|
(34)
|
|
22
|
(34)
|
|
135
|
(32)
|
|
Daily smokers
|
30
|
(42)
|
|
29
|
(23)
|
|
30
|
(19)
|
|
7
|
(11)
|
|
96
|
(23)
|
|
Diabetes mellitus
|
10
|
(14)
|
|
20
|
(16)
|
|
15
|
(9)
|
|
7
|
(11)
|
|
52
|
(12)
|
|
History of atrial fibrillation
|
6
|
(9)
|
|
14
|
(11)
|
|
40
|
(25)
|
|
24
|
(38)
|
|
84
|
(20)
|
|
Comatous upon admission
|
12
|
(17)
|
|
13
|
(10)
|
|
31
|
(20)
|
|
19
|
(30)
|
|
75
|
(18)
|
|
History of dementia
|
0
|
(0)
|
|
2
|
(2)
|
|
15
|
(9)
|
|
5
|
(8)
|
|
22
|
(5)
|
|
Signs of ischemia on CT
|
33
|
(47)
|
|
89
|
(70)
|
|
108
|
(70)
|
|
37
|
(58)
|
|
267
|
(63)
|
|
Cerebral bleeding documented on CT
|
16
|
(23)
|
|
15
|
(12)
|
|
15
|
(9)
|
|
7
|
(11)
|
|
53
|
(13)
|
|
Dead in hospital during the acute phase
|
7
|
(10)
|
|
21
|
(17)
|
|
25
|
(16)
|
|
18
|
(28)
|
|
71
|
(17)
|
|
Discharged to home
|
50
|
(70)
|
|
69
|
(54)
|
|
71
|
(45)
|
|
15
|
(23)
|
|
205
|
(49)
|
|
Transferred for further rehabilitation
|
12
|
(17)
|
|
21
|
(17)
|
|
25
|
(16)
|
|
6
|
(9)
|
|
64
|
(15)
|
|
Transferred to permanent nursing home
|
2
|
(3)
|
|
15
|
(12)
|
|
37
|
(23)
|
|
25
|
(39)
|
|
79
|
(19)
|
|
Dependent at discharge
|
12
|
(17)
|
|
40
|
(31)
|
|
69
|
(43)
|
|
31
|
(48)
|
|
152
|
(36)
|
|
Independent at discharge
|
52
|
(73)
|
|
66
|
(52)
|
|
65
|
(41)
|
|
15
|
(23)
|
|
198
|
(47)
|
|
Recurrence in the observation period
|
9
|
(14)
|
|
28
|
(26)
|
|
27
|
(20)
|
|
7
|
(15)
|
|
71
|
(20)
|
|
Dead after discharge
|
11
|
(15)
|
|
52
|
(41)
|
|
98
|
(62)
|
|
44
|
(69)
|
|
205
|
(49)
|
Clinical findings and laboratory test results
At the first examination in the hospital, 75 (18 %) of the patients were comatous or deeply somnolent (GCS < 11), a condition that rendered a detailed neurological examination more difficult. 22 patients had previously been diagnosed with dementia. Right-sided neurological symptoms were observed in 157 (37 %) and left-sided symptoms in 166 (39 %) patients. In 95 (23 %) patients no lateralisation of the symptoms could be determined. 280 (67 %) had pareses in the upper extremity and 242 (57 %) in the lower extremities. 210 (50 %) had aphasia, dysarthria or swallowing difficulties. 17 (4 %) patients were hospitalised for other causes than stroke and experienced a stroke during the stay.
Mean values for clinical chemical variables were: haemoglobin 13.6, leucocytes 9.3, thrombocytes 245, CRP 25.9, glucose 6.9, total cholesterol 5.9, sodium 40 and potassium 4.0. Elevated CRP upon hospitalisation was found in 123 patients. The mean value for CRP was 61 in those who had CRP above the normal value.
Diagnostic imaging
CT caput was performed once or more in 411 (98 %) of the 421 patients. CT caput showed stroke or signs of cerebral ischemia in 267 (63 %) patients, and primary cerebral haemorrhage in 53 (13 %) patients; two patients had bleeding in the infarct area. Table 1 shows age distribution in the register for patients with cerebral haemorrhage and stroke. Table 2 presents hospital mortality, function and long-term survival separately for cerebral haemorrhage and cerebral infarction.
|
Table 2 Hospital mortality at the index stroke, total mortality at the end of the observation period (January 2003), outcome and recurrent stroke related to cerebral haemorrhage or cerebral infarction in the register. Fischer’s exact test was used to test whether there were significant differences between the groups
|
|
Stroke
|
Cerebral haemorrhage
|
Total number
|
P-value
|
|
No. of hospitalised
|
368
|
53
|
421
|
|
|
Dead in hospital in the acute stage
|
65 (17.7 %)
|
6 (11.3 %)
|
71 (16.9 %)
|
Not significant
|
|
Dependent on others upon discharge
|
123 (33.4 %)
|
29 (54.7 %)
|
152 (36.1 %)
|
< 0.05
|
|
Recurrence during the observation period
|
68 (22.4 %)
|
3 (6.3 %)
|
71 (20.3 %)
|
< 0.05
|
|
Dead in January 2003
|
241 (65.5 %)
|
35 (66.0 %)
|
276 (65.6 %)
|
Not significant
|
|
Not registered recurrent stroke
|
101 (27.5 %)
|
15 (28.3 %)
|
116 (27.5 %)
|
Not significant
|
Medicines at hospital admission
101 (24 %) patients used blood platelet inhibitors, and acetylsalicylic acid (mean dose 149 mg) was the only treatment used. 34 (8 %) patients used orally administered anticoagulation with warfarin. 170 (40 %) patients used antihypertensives at admission.
Clinical course
71 (17 %) patients with an average age of 77 years died during hospitalisation. The mean stay was 18.4 days. Of the 350 patients discharged alive, 205 (59 %) were discharged directly to their home, and 198 of these were assessed as independent. 64 (18 %) were discharged to an institution for further rehabilitation, while 79 (23 %) were assessed as needing chronic care (dependent) and were transferred to a nursing home. Figure 1 presents functional status by age groups at discharge. Table 3 and Figure 2 present functional status at discharge by OCSP classification. 171 of 350 (49 %) patients that were discharged alive still had reduced function in the upper extremities and 150 (43 %) had reduced function in the lower extremities. Aphasia, dysarthria or swallowing difficulties were still present upon discharge for 102 (29 %) patients.
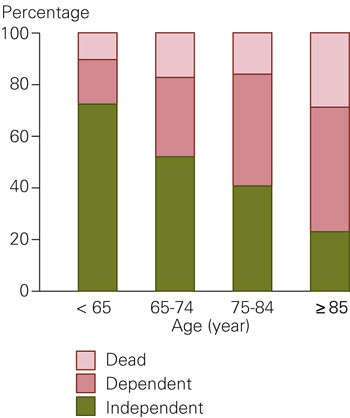
Figure 1 Hospital mortality and functional status upon discharge related to age groups
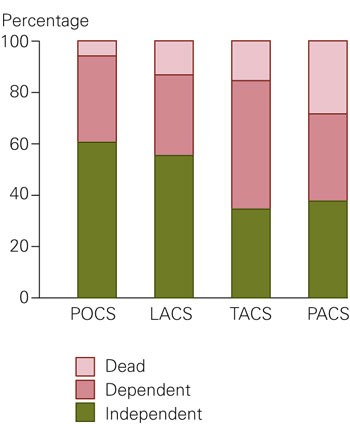
Figure 2 Hospital mortality and functional status upon discharge related to OCSP-classification as follows: POCS (posterior circulation syndrome), LACS (lacunar circulation syndrome), TACS (total anterior circulation syndrome), PACS (partial anterior circulation syndrome)
|
Table 3 Mortality and functional status upon discharge by the OCSP classification: POCS (posterior circulation syndrome), LACS (lacunar circulation syndrome), TACS (total anterior circulation syndrome), PACS (partial anterior circulation syndrome)
|
|
Number (%)
|
|
POCS
|
TACS
|
PACS
|
LACS
|
Not classifiable
|
Total
|
|
No. in the group
|
88 (21)
|
85 (20)
|
176 (42)
|
48 (11)
|
24 (6)
|
421 (100)
|
|
No. of haemmorhages
|
15 (17)
|
6 (7)
|
29 (16)
|
1 (2)
|
2 (8)
|
53 (13)
|
|
Dead in hospital
|
4 (5)
|
13 (15)
|
48 (27)
|
6 (12)
|
0 (0)
|
71 (17)
|
|
Dependent
|
30 (34)
|
42 (50)
|
61 (34)
|
15 (31)
|
2 (8)
|
150 (35)
|
|
Indpendent
|
54 (61)
|
30 (3)
|
67 (38)
|
27 (56)
|
20 (83)
|
198 (47)
|
Antithrombotic medication upon discharge
303 of 350 patients that had been discharged had experienced a myocardial infarction and had an indication for antithrombotic treatment. Of these 199 used acetylsalicylic acid (mean dose 165 mg) and 74 patients with atrial fibrillation used anticoagulation in the form of warfarin. So, 273 of 303 patients (90 %) received antithrombotic therapy according to guidelines. Oral coagulation was not started in 28 patients with atrial fibrillation treatment, 16 of these patients were more than 80 years old.
Antihypertensive medication upon discharge
Of 350 discharged patients, 146 (41.7 %) used one or more types of antihypertensive treatment: 55 used betablockers, 56 calcium antagonists, 61 ACE inhibitors and 66 used diuretics. Antihypertensive treatment was started in five patients who had not received such medication previously. 206 (59 %) were discharged with elevated blood pressure (> 140/90 mm Hg), and of these, 106 (51.5 %) were discharged without any type of antihypertensive treatment.
Recurrence of stroke and survival
The 350 patients who were discharged alive were followed until 31 January 2003. In this period 77 new admissions were registered because of stroke recurrence in 71 patients. Mean time to the first recurrent stroke was 2.8 years and the recurrence rate over a 5-year period was 22 %. 205 deaths were recorded for the group.
Figure 3 presents the Kaplan-Meier curve for survival without recurring stroke by age groups for the 421 patients. Figure 4 presents Kaplan-Meier curves of survival without recurring stroke for the 397 patients who could be categorised according to OCSP. We did not find a significant difference in survival after correcting for age differences in the patient group with or without hypertonia (140/90 mmHg).
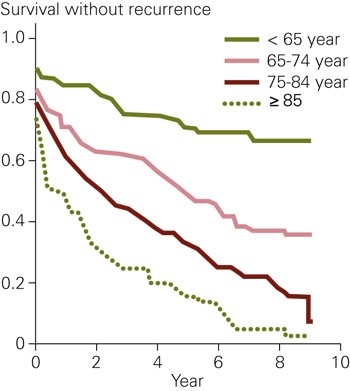
Figure 3 The Kaplan-Meier curve describes survival without recurrence in 421 patients related to age groups at the time of the stroke
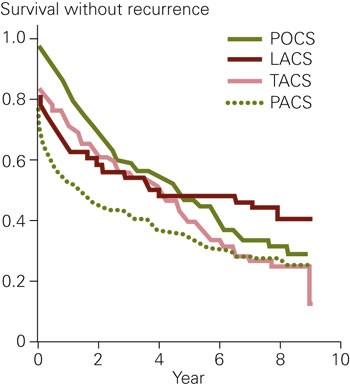
Figure 4 Kaplan-Meyer plot of survival without new recurrence for 397 patients who could be classified according to the OCSP-classification: POCS (posterior circulation syndrome), LACS (lacunar circulation syndrome), TACS (total anterior circulation syndrome), PACS (partial anterior circulation syndrome)
Discussion
Our register comprises all patients in Asker and Bærum who had been hospitalised with stroke; it therefore also includes the sickest stroke patients who are often not treated in stroke units. The national population statistics data (Statistics Norway) provide valid data for the living and dead. We therefore believe we have identified all deaths that have occurred in the register population. However, a study population of 421 still limits our possibilities of drawing conclusions. Our register contained several categories of stroke with different pathology and prognoses. Although the pathological processes behind cerebral haemorrhage and cerebral infarction are different, we did not find significant differences in hospital mortality and long-term survival between these conditions (tab 2). Neither did we find differences between patients with first time stroke and those who had previously had stroke. We therefore chose to use the entire stroke population as a basis for further analyses.
In 1994 - 95, the majority of hospitalised stroke patients had substantial neurological outcomes and nursing needs. As a consequence of changes in the health services, an increasing number of patients with mild and transient strokes are now admitted to hospital. Our results reflect a population that was hospitalised for stroke in 1994 - 95 and are therefore most relevant for assessment of prognoses and results in treatment of stroke patients with serious cerebrovascular disease.
Results of stroke treatment in hospital
We found that hospital mortality was 16.7 %. This is a relatively high mortality when compared to more recent data (2000) from the stroke register in Sweden (Riks-Stroke), which reports a 28-day mortality of 9.5 % in stroke wards and 13.7 % in general wards (10). Our register population was affected by relatively large and serious strokes, and the mortality data are likely to reflect that.
Secondary prophylaxis and existing guidelines
An important function for clinical registers is to relate patient treatment to existing guidelines for clinical treatment and prophylaxis. Antithrombotic treatment was well established in 1994 - 95, and in our study we found that 273 of 303 (90 %) patients that were discharged after stroke received treatment with acetylsalicylic acid or warfarin according to guidelines. Of 206 who were discharged with hypertension, 106 (51.5 %) did not receive any antihypertensive treatment. Secondary prophylaxis in the form of blood pressure control has a documented effect on recurrent stroke, but not on survival (5). The usefulness of such prophylaxis was questioned during the inclusion period, and one explanation for the low number of patients that received antihypertensive treatment can be that one was afraid to reduce the cerebral perfusion pressure in these patients. In our limited register we see a possible effect after three years on relapse-free survival. However, the numbers are not significant when corrected for age difference between the groups. The number of recurrent strokes is relatively small in comparison with the total mortality in the observation period; our observations therefore seem to fit with findings in larger meta-analyses (5).
Prognostic factors for recurrent stroke and survival
Several studies have assessed data on long-term follow-up of stroke patients (4 - 17). However, comparison between studies may be difficult as recording of recurrent strokes, other methodology and study populations differ. One study relates long-term prognoses to various types of stroke such as cerebral haemorrhages, lacunary infarctions and thromboembolic infarctions. In our study, patients with atrial fibrillation and thromboembolic strokes were six years older than other patients when the stroke occurred. Age-related skewing of data will in general affect a number of analyses related to pathological processes. To reduce this problem we have chosen to present data related to the OCSP- classification that connect the stroke to extent and localisation ; this substantially reduces the age effect between groups. As other authors, we find that lacunary strokes and strokes in the posterior circulation (LACS and POCS) have the best prognosis, while stroke in the anterior circulation (PACS and TACS) have a more serious prognosis. This is important information for adjusting and interpreting short and long-term results from different populations. The prognostic importance of age on survival curves and function results upon discharge has previously been described in several register studies of quite different designs (11, 14, 16 and 17). In our register, age is the factor that most influences outcome.
We found a five-year recurrence rate of 22 %; in other studies it varies from 15 % to more than 30 % (5, 16, 18). For studies performed before acetylsalicylic acid became commonly used for prophylaxis, this may explain part of the variation. Post mortem findings when death has occurred outside of hospital are reported to a varying degree; this will naturally contribute to improved information on recurrent stroke and cause of death. However, it is interesting that the OCSP group did not find statistical differences in recurrence rate related to neither age nor type of stroke. From other studies it may seem that cerebral haemorrhages tend to be associated with worse outcomes in the acute stage, but to fewer recurrences in the follow-up period (15, 16). We see similar trends in our register, but the statistical material for cerebral haemorrhages is quite small in all the registers.
Conclusion
Patient age at the time of stroke and the anatomical extent of the stroke are important prognostic factors for survival and function after stroke. This study shows that half of the stroke patients were not followed up according to existing guidelines for blood pressure treatment. Nine of 10 patients with stroke received secondary prophylaxis in the form of antithrombotic treatment with acetylsalicylic acid or warfarin. This study provides information that can be used for quality assurance of clinical work with stroke patients. A national stroke register can provide valuable information about clinical practice and form a basis for improved treatment of this patient group.