Complex chronic diseases require an increasing proportion of society’s resources and represent a growing challenge. Valid biomedical models of aetiology, pathogenesis, treatment and prognosis are inadequate for understanding these diseases. The article discusses current knowledge about the impact of stress on the immune, hormonal and central nervous systems, and integrates this knowledge with a phenomenological understanding of the body in an attempt to explain the complex chronic fatigue syndrome. The medical significance of the individual’s biography is highlighted, and the inadequacy of statistics-based biomedical research when aiming to understand complex disease is presented. By regarding human beings as persons whose experience affects them physically and who both create and convey meaning, we claim to have transgressed the mind-body-dichotomy in complex disease development. The dichotomy converges in the lived body.
«The disparity between physical and psychological stressors is an illusion. Host defence mechanisms respond in adaptive and meaningful ways to both» (1).
The development of physiology in the 1800s provided modern medicine with a theoretical foundation that was useful for diagnosis and treatment of organ-specific disease. In the same period, the growing understanding of infectious disease and immunological defence mechanisms proved valuable in treating and classifying many previously unexplained diseases. Explanations of these diseases (easy to understand in the sense that clear links are given between malfunction and change in structure) are compatible with and provide part of the basis for the modern understanding of biomedicine.
Another group of diseases, which are complicated in the sense that we know little or nothing about their biological basis, do not accord with the biomedical paradigm for understanding disease. Aetiologies of diseases such as chronic fatigue syndrome, rheumatic diseases and chronic pain syndromes are still not adequately understood (2, 3). Classic biomedical approaches have not explained them so far, and it is often pointed out that «more research is needed to improve our understanding».
In this article, we aim to provide a broader understanding by arguing that in order to categorize complex, unexplained diseases, they must first be considered in an integrated perspective where evolution, ontogeny and societal relationships are taken into account. Our contention is that many complex diseases are ontogenetically conditioned, i.e. conditioned by the individual’s complete development from fertilized egg to the onset of illness. If this is correct, not only biological but also historical, biographical, sociocultural and relational aspects are relevant. Likewise, methodology based on statistical comparisons between groups will not suffice. Experts currently consider chronic fatigue syndrome (CFS/ME) as a condition that fails to concord with the traditional division of disease into «somatic» or «mental» (3, p. 12). Consequently, our understanding should not only be anchored in a broader perspective and other methods, but also transcend classic, dualistic thinking. This can be achieved by regarding the biological, psychological and sociocultural aspects as parts of a whole; and by seeing the individual in a context of meaningful relationships to other people.
By reacting to situations, individuals express their experience, which is species-specific and ontogenetically determined. Whereas evolutionary experience, that forms the historical context, converges towards a stereotypic response, experience linked to culture, gender and language also forms a relevant context and contributes to diverging responses. The human organism’s «interpretation» of the situation and its context is decisive for whether the reaction becomes health-preserving or health-threatening. The response will in turn affect the way the original situation is understood. An infection will for example activate the innate and adaptive immune system, which will lead to restored health (with immunological memory) or to chronic inflammation in the form of allergy or autoimmunity. The result depends on the organism’s genetic outfit, previous experience with the infectious world and the relevant context (fig 1).
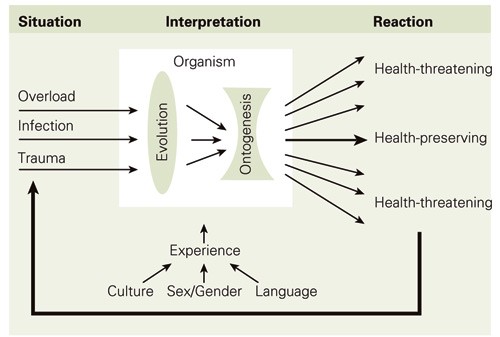
Figure 1 The human organism’s «interpretation» of the situation and its context is decisive for whether the reaction becomes health-preserving or health-threatening
We base our view on studies of associations between immune, nervous and endocrine functions; more specifically, the way in which immunological phenomena are integrated into the other functions and how strain in general and chronic overload in particular can affect them all.
The immune system’s response characteristics
Our immune system, which recognizes and responds to molecular stimuli from both the world around us and our body, can be divided into the «innate» and the «adaptive». The two systems are linked in that the adaptive response gets its information about the antigenic universe from the innate system; also the adaptive response, once activated, has repercussions on the effector cells in the innate immune response. Thus, our common history (evolution) is connected to our individual learning (ontogenesis) (4).
The innate immune system is almost identical for all of us, but the adaptive immune system is unique to each individual. During an infection, the innate system functions as our non-cognitive sensory apparatus: leucocytes, including natural killer cells (NK cells), macrophages and granulocytes will together with acute phase molecules such as CRP, complement components and interferons recognize the foreign agent as foreign and thereby set up a defence. The adaptive system, consisting of T cells and B cells and their respective receptors, also allows us to respond flexibly to complex surroundings that are ever changing. Flexibility does however include the possibility of responding wrongly to safe stimuli such as allergens and one’s own molecules (4).
Because genes that code for T-cell receptors and immunoglobulins go through an ontogenetic adaptation, identical twins with identical innate immune systems will for example be able to develop quite different adaptive systems during their lives (4). The ontogenetic adaptive mechanisms enable each antigen stimulus to induce a context-dependent adaptive immune response, which in turn shapes later immune responses through a lymphocyte-mediated immunological memory (4). In this way, the immune system becomes individualized and one can say that antigenic experience is written into the body.
Allostasis
Ever since Hans Selye (1907 - 82) (5) used the term «stress» for various external influences and claimed that stress can be both positive (eustress) and negative (distress), others have partly developed and partly rejected his models. The theories do however have a common core: the individual’s responses (considered positive for survival during danger) are adjusted by hormonal interactions between the hypothalamus, the pituitary (gland) and the adrenal gland (HPA axis).
In an attempt to clarify the development from «eustress» to «distress», Bruce McEwen has worked with the concept «allostasis». It means stability through change and is associated with the systems that provide flexible adaptations to different demands (6). Allostatic «load» accumulates in crises and repeated situations of danger. In situations with continual stress; as in war and emergencies, in the loss of a basis for existence in ongoing conflicts and long-term suppression of strong feelings (as when caring for a close family member with Alzheimer’s disease), the individual will suffer from allostatic load. There are strong empirical grounds for believing that such constant emotional overload can wear out the body’s adaptative systems. This may lead to reduced immunity, autonomous dysfunction, cardiovascular disease, osteoporosis, atrophy of the nerve cells and more rapid cell aging in general (6 - 10), and to a complexity of functional disturbances defined as metabolic syndrome in both women and men (11, 12).
Corticosteroids are a causal factor in the development from acute or chronic «stressors» to overload and exhaustion. This is documented in studies, which show high allostatic load in people with the diagnosis chronic fatigue syndrome (13) and also flat cortisol curves (reflecting low production without variation) in adults with the diagnoses fibromyalgia, chronic fatigue syndrome and posttraumatic stress disorder (6).
Psychoneuroimmunology
The immune, hormonal and central nervous systems form a tight network of interactive cells and molecules. They are influenced by each other and by their surroundings, and they are adjusted during ontogenesis so that they harmonize with each other (4, 10). The relationship between stress and immunology is up to now best described by the so-called cytokine shift model, which is based on the fact that two types of helper T cells (Th1 and Th2) produce different types of cytokines (14). While cytokines produced by Th1 cells lead to inflammation with increased protection against intracellular microbes and neoplasia, the Th2 cytokines lead to increased humoral immunity with a disposition towards allergy and autoimmunity. According to this model, a disturbed balance between Th1 and Th2 cytokines could lead to illness.
The model does not, however, embrace all aspects of the immune response to chronic overload. It does not for example include the fact that corticosteroids cooperate with catecholamines to direct the immune response towards a Th2 response (15). Nor does it show that chronically high levels of glucocorticoids in certain organ systems seem to promote rather than inhibit inflammation (16).
The threatened person
To be abused and mishandled is a seriously destructive experience, especially if this happens early in life and even more so if there is no chance of defending oneself. A positive correlation between such humiliation, autoimmune processes and cancer has been demonstrated in an older population: sexual abuse in childhood was, for the men, strongly related to diseases of the thyroid gland and, though weaker, to rheumatoid arthritis. For women, there was a positive correlation to both arthritis and breast cancer; and the risk of breast cancer increased with repeated sexual violation throughout life (17). Another study showed positive correlations between having been abused, ill treated or neglected as a child and manifestations of lung disease, cardiac disease, inflammatory and autoimmune disorders, peptic ulcer and diabetes (18).
There is a polarization between «self» and «foreign», «one’s own» and «the other’s»; and a continuum of experience from «safe» to «dangerous», along which choices are made. The individual can choose to accept, open up and adapt to «the other one», or protect and defend themselves. But when something must be tolerated that is really intolerable; when the boundaries of integrity have been violated and protection is impossible; and when the person must do violence to themselves in order to endure the unendurable: then the ability to adapt breaks down and the result is disease. The processes which then dominate cross boundaries. In this way, they reflect their source: damaged integrity (fig 2).
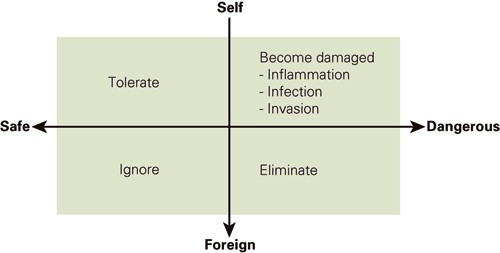
Figure 2 In the polarisation between «self» and «foreign» and the continuum of experience from «safe» to «dangerous» the individual can choose between opening up, adapting, protecting and defending themselves. Individuals under coercion do not have such choices. The processes that then take over cross boundaries. They thereby mirror their own source: damaged integrity
Studies with very different designs have documented that NK cells, macrophages, and T and B cells are affected by the extent to which a person experiences reality as overwhelming and unmanageable (1,6,8). The immune system is thus further individualized and modified. This means that not only protective, but also destructive experiences can be written into our bodies.
The lived body
On the basis of this evidence, we maintain that the traditional scientific assumption of a division between physical and psychological stress is invalid. We take it for granted that experience is perceived, interpreted and integrated bodily because human beings are present in this world as bodies. According to (the) philosopher Maurice Merleau-Ponty (1908 - 62), people cannot perceive, experience, learn or know anything at all without their bodies taking part in the sensing, learning and knowing (19). He sees the body as life embodied. This means that lived time (temporality), places (spatiality) and relations (relationality) are integrated bodily (corporeality). There is therefore no such thing as an unembodied thought or emotion or a purely psychic experience, whatever the distinguishing hallmark.
What is stressful for whom and how depends on the context and can therefore only to a limited degree be based on knowledge generated from methods designed for generalisation. Who reacts to what, why and how cannot be predicted with the aid of a one-dimensional biological or mechanical concept of the body. The human body is, always and without exception, a lived body, in which history and biography are woven together with interpersonal meaning as well as individual purpose (19, 20). Experience is integrated in all bodily processes because:
human beings create and convey meaning in coexistence with other human beings and are therefore situated in a relational and sociocultural context
every person interprets experience within their own horizon or space which only partly coincides with «all the others», even within the same cultural circle or society
human interaction will always and everywhere be informed by systems of values, signs and symbols which form interpersonal reference frames that are essential for any human fellowship
human interaction naturally comprises conflicts, tensions, diversity, contrasts and changes which do not disappear in reality even when an objectifying methodology excludes these elements from the study - and thereby from science
It is not the brain or the central nervous system that interpret events and give them meaning. It is the individual as a whole who does so with the help of the brain, the central nervous system and other integrated structures and elements. The individual interprets happenings, their own experience, even when many others share the same experience. That is why studies of even apparently pure biological processes, such as the immune response, should take into account these prerequisites of human existence.
Chronic fatigue
Solid epidemiological evidence links «chronic stress» to an increased risk of cardiovascular disease, lung and liver disease, obesity, cancer, inflammatory and autoimmune disorders, early menopause, osteoporosis, depression, anxiety, infections, chronic pain and chronic fatigue (1, 6 - 9, 11, 12, 17, 18, 20). Of all these conditions, the last two are the ones least understood from a biomedical point of view. Chronic fatigue, especially, represents a medical enigma (3).
In a recent review article of the condition known as CFS (chronic fatigue syndrome) (in Anglo-American literature, the authors write: «Numerous immunological parameters have been tested and many of them are abnormal but inconsistently so among the various studies.» They continue, «A disruption of the HPA axis has been implicated in the pathogenesis of CFS. Early studies have shown that cortisol levels in patients with CFS are reduced…» (21).
One of the most consistent findings has been that various infections can trigger a state of constant low energy or tiredness as well as other health problems, with chronic pain showing up most frequently, either in general or localized in different parts of the body (3, 21). When infections are a possible common denominator, it is reasonable to ask if there are certain conditions in the individual patient that cause many infections (including ones not normally seen as problematic) to have such devastating consequences. If CFS is a condition that includes a chronic sense of not coping, the implication is that the syndrome is a consequence of changes in several systems. This further signifies that the changes in each system may be too small to appear in biochemical and immunological tests. So, a conflict between systems caused by strain leads to the clinical syndrome, rather than an isolated dysfunction within one system.
Of all possible causes assessed, defined as either somatic or psychiatric, no convincing explanation has come up. Previous infections are a typical symptom of the condition, but even more consistent is the effect of what is persistently defined as emotional stress. In the aforementioned review (21) the authors write, «… emotional stress is known to influence immune responsiveness and virus pathogenesis, and has a profound importance to our understanding of the pathogenesis of infectious diseases and cancer, and may therefore be a key aspect in the pathogenesis of CFS» (our italics).
We wish to emphasize two aspects of this conclusion. Firstly, it has been shown, as we have mentioned, that it is not possible to separate «emotional» stress from other types of stress, both from a biological and an existential perspective. Secondly, the authors contradict their own conclusion in that they categorize «emotional stress» as belonging to the same analytical level as the three other frequent findings in the CFS patient, namely immunological, hormonal and central nervous system deviance. The various immunological and hormonal aspects of the lived body are neither autonomous, nor independent of the body they are a part of. Neither does the central nervous system live independently of its owner’s life, consciousness, perception and situation. These three aspects can neither ontologically nor epistemologically be considered «on the same level» as painful and difficult experiences. Consequently, the conditions categorized as «emotional stress» are a prerequisite for understanding the complex patterns of known dysfunctions and deviations in the cellular, humoral and central nervous system.
Furthermore, defining the category «emotional stress» is problematic. In epidemiological research the term usually comprises supposedly temporary stresses and strains. Frequently studied examples are exams, money problems, job loss, divorce, the death of a near relative or serious illness in the family, or among friends (8). But such problems may last a long time. A person forced into a divorce may continue to suffer long after the event. A child’s death may affect parents decades later. Moreover, there are stresses and strains that are constant and impossible to avoid because they are socioculturally legitimized or covered up and concealed. These concern discriminating social structures related to skin colour, ethnicity, gender, sexual preference etc. and humiliating relationships in the form of destructive enmity within the family. All this signifies that an abstract stress typology is not helpful when exploring dysfunctional relations between the immune, hormonal and nervous systems. An adequate epistemological and methodological starting point is rather the individual’s situation in life.
Interpretation
On the basis of a physiological understanding of organ-specific disease and an immunological understanding of infectious and inflammatory disorders, we have argued that a biomedical understanding is too limited to embrace complex disease and breakdown of functions. Biomedical specialties, oriented towards organs and organ systems or functional entities, converge more and more on findings that challenge the traditional specialty boundaries and the structuring dichotomies grounded in the premise that the human body and mind are separate and different.
«Converging specialties», such as psychoneuroimmunology, mirror the traditional view on what is separate or can be separated and a growing acknowledgement of what acts together or, seen from another epistemological perspective, belongs together. This is shown in studies of complex diseases such as cancer and inflammatory and autoimmune disorders. It becomes especially clear in disorders known as «functional» in somatic medicine and «somatoform» in psychiatric medicine. Such patterns of so-called comorbidity, where disorders that are traditionally regarded as independent of one another seem to overlap, appear to fall outside the biomedical framework. They fully escape the profession’s divided and divisive grip. By their mere existence, they challenge the medical community’s view of the body, their understanding of what it is to be human, and question whether present approaches to obtaining knowledge are adequate for helping people who suffer.
