Hypospadias means «crack/opening beneath». The name refers to a malformation where the urinary tract opening, the meatus, is located on the ventral side of the penis in boys or on the anterior wall of the vagina in girls. Hypospadias in girls will not be further discussed, as it is a rare condition of minor medical importance.
The incidence of hypospadias in Europe is 1 – 3 cases per 1 000 live-born boys (1). This corresponds to about 90 cases in Norway annually. Some countries report an increased occurrence from 1960 to 1980 (2 – 4). This may be a real increase, but other explanations can be improved diagnosis and increased reporting of less severe cases.
For most malformations it is known when the abnormality occurs in the embryo, but for hypospadias the cause is unknown, unclear or multifactorial. During embryogenesis, normal development of the penis and male urethra depend on androgen stimulation. Animal tests have shown that if testicles in the male embryo are removed early, a female appearance of the external genitalia will develop (5). The same occurs with insufficient androgen receptor in tissue and with 5-alpha reductase deficiency, which is necessary for the transformation of testosterone into the more biologically active dihydrotestosterone. Other endocrine effects, for example caused by gestagens, have also been mentioned as possible causes of hypospadias (6). In female embryos, excessive androgen exposure will lead to virilisation of external genitalia, e.g. in the adrenogenital syndrome. Possible associations between hypospadias and a number of external factors, such as pesticides used in agriculture, have been also been considered (7). So far it is not clear whether such associations exist, but if so, they are unlikely to be frequent causes of the condition. Data from the Norwegian Medical Birth Registry indicate that a prematurely detached placenta can be a contributing factor in the development of hypospadias (8). Genetic factors are also relevant. If a close relative (father, brother) has hypospadias, the next male infant has an increased risk of being affected (9, 10). Future genetic research is likely to contribute to the elucidation of etiology and pathogenesis of hypospadias (11). Proximal types of hypospadias and ambiguous sex may have a chromosomal and/or hormonal cause.
Material and methods
Incidence, etiology and diagnosis of the hypospadias condition are discussed on the basis of clinical experience and thorough, but non-systematic literature searches (PubMed). The discussion of possible treatment, including some relevant surgical approaches, is based on experience from recent years in the pediatric surgery division at Ullevaal University Hospital, Oslo.
Diagnostics
Hypospadias is usually diagnosed during the routine examination after birth (fig 1). While diagnosis is easily established in the presence of an external and visible malformation, less severe disease is sometimes not identified. Depending on the position of the meatus, the condition is classified as glanular/subglanular, penile, penoscrotal or perineal. Most hypospadias are of the distal type; e.g. 69 % of the cases were distal in a Norwegian follow-up study (12) (fig 2). The ventral part of the penis is more or less developed. In addition to a misplaced urethral opening, most affected infants will have a dorsally placed, hood-formed foreskin that does not cover the ventral portion of the glans. In addition, there may be varying degrees of ventral curvature of the penile shaft, and a variably developed corpus spongiosum (fig 3). Some patients have a narrow meatus which requires a meatotomy before final surgical correction. In rare cases, there is also pathological torsion of the penis; there is also an increased occurrence of micro penis. If one or more of these conditions exist despite a normal position of the meatus, the abnormality is usually referred to as «hypospadias». In some cases, parents’ reports of a backward urine flow and/or an increasing downward curvature of the penis when erected can lead to the diagnosis hypospadias. In most cases, careful clinical examination will be sufficient. With proximal types, radiological examination of the urinary tract and hormonal and chromosomal analyses are appropriate. Other urogenital abnormalities may be associated with more pronounced hypospadias with kryptorchism (abdominal retention of the testicles) as one of the most frequent abnormalities.
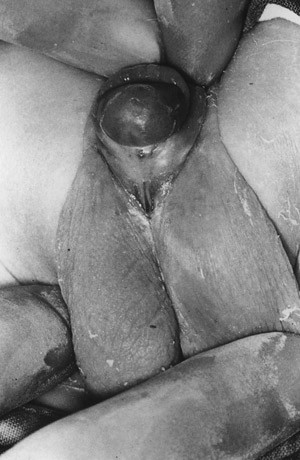
Figure 1 Hypospadias- proximal type (12). Reproduced with permission
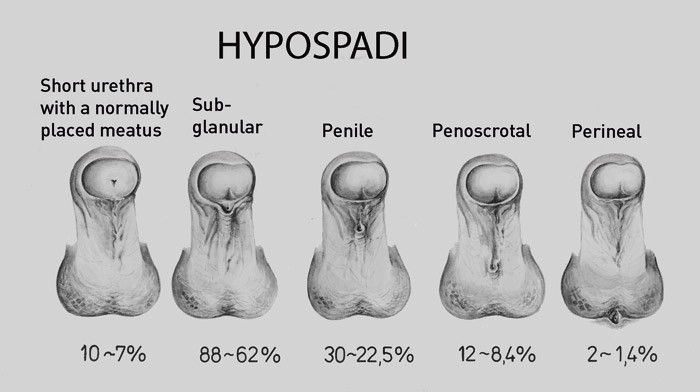
Figure 2 Hypospadias types – percentual distribution (12). Reproduced with permission

Figure 3 Ventral curvature of penis (chorda) (12). Reproduced with permission
Treatment
If there is no meatus stenosis requiring urgent treatment, most centres will treat hypospadias after the infant has turned one year. In the 1970s, treatment was usually started when the child was 4 – 5 years old, so that therapy could be completed before entering grade school. A psychological point of view gives many reasons for performing surgery between the age of six and 18 months (13), but the small size of the penis at this age poses more of a technical challenge. Therefore, pre-surgical treatment with testosterone is sometimes advised. In many countries correction of hypospadias has been taken over by pediatric surgeons, but plastic surgeons and urologists still perform such procedures.
Few surgical conditions have been the basis for development of such a variety of procedures; 200 – 300 different methods have been described. This reflects the great variation of hypospadias and the frequent complications related to its surgical correction. In the 1960s and 70s, it was quite common that individual surgeons and departments used different standardized methods. In the pediatric surgery division at Rikshospitalet in Oslo, a two-step procedure was most commonly used (12). Another two-step method was later implemented in the department of plastic surgery at the same hospital (14).
Surgical treatment aims at a result that is functionally and cosmetically as close to normal as possible, while minimizing the risk of complications. The principle of treatment is to straighten the penis and to construct a distal urethral opening with a normal position of the meatus, all well covered by tissue. The newly formed urethral opening can generally be modeled from adjacent penile skin, including foreskin. In rare cases, free skin or mucosa transplants are necessary.
During the last 10 – 15 years, many centres have adopted a one-step method. In general, the choice of surgical method depends on the type of hypospadias and additional factors such as curvature, skin/scrotum abnormalities, affected person’s or caretaker’s request for or against circumcision etc. The most common procedure with the distal form at the pediatric department at Ullevaal University Hospital is MAGPI (meatal advancement glanular plasty included) (15). The so-called TIP-procedure (tubular incised plate), most commonly used with penile types, usually results in a satisfactory degree of straightness and cosmetic appearance, with near normal appearance of the meatus on the penis head (16). In case of proximal forms with pronounced curvature of the penis and in cases of secondary surgery after previously unsuccessful procedures, the foreskin is often used to extend the urinary tract – «onlay flap» or «island flap» (17). At the pediatric surgery department at Ullevaal University Hospital, there has so far been no need for mucosa transplants for urethra reconstruction, but this is an alternative method. If possible and requested, a foreskin remodeling procedure may be performed, by which the foreskin is sutured together underneath the penis head. Circumcision of the foreskin is not advised (neither on a ritual nor traditional basis) before completion of hypospadias surgery. Sufficient foreskin should be available in case there is a need for additional tissue for repairing complications.
After distal hypospadias surgery, the patient is usually released on the same or the following day. Correction of the proximal types require a catheter to be placed in the reconstructed urinary tract (fig 4). In this case the patient usually remains in the hospital for 3 – 5 days, and returns for removal of the catheter 7 – 10 days after surgery. Antibacterial prophylaxis is administered during surgery and as long as the catheter remains in place.

Figure 4 Completed operation of hypospadis with newly constructed distal urethra, inserted catheter to the urinary bladder and bandaging with transparent plastic foil (Tegaderm)
157 hypospadias-related surgeries were performed at Ullevaal University Hospital between January 2002 and September 2005; 102 of these were genuine hypospadias operations (83 new cases and 19 secondary surgeries or step two surgeries) (unpublished data).
Results
The cosmetic result of hypospadias surgery is significantly better today than in previous decades, with improved placement and more normal appearance of the meatus on the penis head. Urethral fistulas, constrictions and persisting curvature remain the most frequent complications after surgery (unpublished data, Ullevaal University Hospital). Fistula problems can be reduced by sufficient tissue coverage over the constructed urinary tract. A spacious urinary tract is essential in order to avoid damage related to high pressure. Stitches that remain for a long time in the tissue also constitute a risk for fistulas. We therefore recommend that suture materials are thin, single filaments that are easily absorbable. Complications due to constrictions can be largely avoided by ensuring that the original meatus and the new meatus have the right dimension, and by ensuring that the urinary tract is sutured over a sufficiently sized catheter. After surgery, the patient is monitored by means of anamnesis and clinical examination, and by urinary stream measurements provided the patient is old enough. Reduced urinary stream speed is usually a temporary problem, but may sometimes require resolution by unblocking or meatotomy. A persisting curvature is a common complication after proximal hypospadias surgery. A straightening procedure may then be necessary. This can be done by pulling tissue together on the dorsal side of the penis. Occasionally a short urethra needs to be extended or requires complete reconstruction. There is some advantage in postponing straightening surgery until after puberty (18).
The desired post-surgical functional results is:
An urinary stream which exits at the top of glans, and which can be controlled
Unrestricted and painless urination
A penis which is straight during erection and exhibits normal sensibility
Studies of adult patients are required in order to determine sequelae/late complications. Such studies obviously do not exist for the more recent methods of surgery. According to published follow-up examinations, most problems occur with a small penis (micro penis) and/or circumcised appearance of the penis (situations that cannot be corrected) in countries where this is not common (19). Because of this, circumcision in patients with hypospadias should be avoided or postponed. Fertility and sexual performance appear to be within normal variation, except for patients with entirely proximal hypospadias (20). Comparative and long-term studies have shown that men who have undergone hypospadias surgery are more self-conscious, timid, and less stress tolerant (21). Nevertheless, psychological abnormalities are rarely pronounced, and most patients can live a normal life (20).
Conclusion
Surgical correction of hypospadias is challenging. The surgeons must possess sufficient knowledge of current treatment techniques, and they must be able to adapt the method of choice to a given type of hypospadias. Conditions that can reduce the risk of complications, particularly fistulas and/or constrictions, should be emphasized. The first operation may be decisive for a lasting and positive result. For further reading, we recommend a recently published monograph written by internationally known experts. This book provides a comprehensive analysis of «hypospadiology», including detailed illustrations that provide a useful and practical guide for surgical procedures (22).