Allergic contact eczema is a T cell-mediated immune response, often referred to as a type IV allergy. Haptens in the skin are transported by Langerhans cells and presented to CD4 and CD8 positive T cells in the lymph nodes, thereby activating and regulating these T cells. The patch test is an important diagnostic tool for confirming and uncovering the cause of suspected contact allergic eczema. At Stavanger University Hospital, two nickel substances (nickel sulfate and nickel chloride) are included in the standard patch test.
Several studies show great variation in the prevalence of contact eczema: 1 to 26 % of those tested are positive (1,2). The incidence of contact allergy to many allergens is increasing in industrialized countries – as we become exposed to more allergens (1). Documentation of the increasing incidence of contact allergy will provide guidance for implementation of preventive measures for those groups of the population most at risk.
Nickel allergy has been the most prevalent type of contact allergy in Western populations for many years. Nickel is used in processes such as gold and nickel plating and in many types of alloys; e.g. white gold, stainless steel and silver-like copper alloys. Direct contact with the skin occurs most often through the use of jewellery (including piercing), belts, glasses, watches and trouser buttons. Items containing nickel are known to cause chronic eczema, especially hand eczema, and nickel allergy has indirect socio-economic consequences in the form of sick leave, disability pension and having to change jobs (3).
The European Surveillance System on Contact Allergies (ESSCA) has collected patch test results from 17 centres in nine European countries since 2001 (4). The Norwegian Dermatological Society set up a register, NOLAR, in 2005 to track the incidence of contact allergic reactions in Norway (5). We wanted to document the most common contact allergens for the population in the southern part of Rogaland and compare them with the results from ESSCA and NOLAR, especially the incidence of nickel allergy.
Material and methods
857 people were tested for contact allergy at the Department of Dermatology in Stavanger University Hospital during 2001 and 2002. The hospital offers health services to about 300 000 people. The patients were referred by doctors in the primary health service for examination and treatment of eczema and, in the cases of suspected contact allergy, for patch testing (fig 1). The test and reading followed standard procedures – the patches were taken off after 48 hours and the reactions read after another 24 hours by one (or two) of only three specialists in Dermatology (5). Reactions + to +++ are considered positive (fig 2) (5). Certain patients known to previously have had a violent reaction were not tested again. The standard serie, consisting of 26 – 29 substances, is regularly evaluated and changed. The most common allergens are described in box 1.
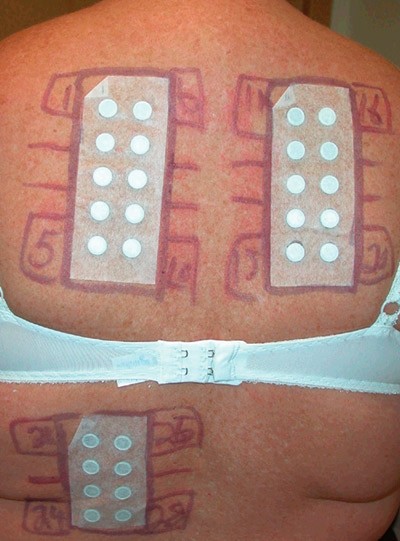
Figure 1 Patch test
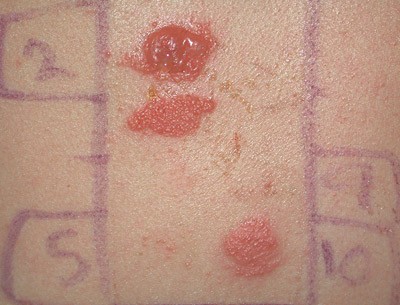
Figure 2 Positive patch test with erythema, vesicles and bullae
Box 1
The most common allergens found in patients tested for contact allergy at Stavanger University Hospital and their areas of use
Nickel: Metal element. Used in buttons, zippers, magnets, handles, kitchen tools, scissors, watches, coins and keys etc.
Cobalt: Metal element. Used in nickel alloys, wet cement, hard metal objects, fresh blue and green pigments for paintings, basic decoration for china
Fragrance mix: Consists of eight perfume chemicals. Used in cosmetics, skin care, make-up, perfume, sun lotion
Balsam of Peru: Brown liquid from a tree in Central America. Contains some of the same perfume chemicals as fragrance mix. Used in skin treatment and as additives in food, toothpaste and cough syrup
Colophonium: Resin from conifers. Used in glue, paste, plasters, printing inks, linoleum, soap, grout (wet cement), cosmetics, chewing gum
Compositae: Daisy, dandelion, found in nature,i.e. salad. Used in cosmetics, herbal medicines and herbal additives in food
Formaldehyde: Chemical compound with bactericide properties. Used in skin care, shampoo, skin cleansers, toilet paper, treatment for non-iron textiles, leather dyeing
Thiuram mix: Rubber additive. Used in all rubber products such as gloves, support stockings, elastic in sock cuffs, shoes, condoms, balloons, car and bicycle tyres
4-phenylenediamine: Chemical colour. Used in hair dyes, heavily dyed fabrics, printing inks
Data were collected by retrospective analysis of medical records for tested patients. General data were recorded; such as age, sex, duration of symptoms, rash site, final diagnosis, other skin disease, possible atopic background and job (6). The project was reported to and approved by the data protection official for research at the Norwegian Social Science Data Services.
Statistics
SPSS 14.0 was used for frequency analyses and chi square tests. Positive reactions to allergens were further analysed using logistic regression to calculate the odds ratio and 95 % confidence interval (CI) with the cut-off point for significance at p < 0.05.
Results
857 patients (mean age 38.3 years, 64 % women) were tested for at least one of the substances in the standard series (e-tab 1). Psoriasis was recorded in 93 cases (11 %), atopic eczema in 356 (42 %) and occupational dermatitis in 184 cases (21 %). Eczema affected mainly the hands (56 %) and/or face (43 %).
|
Table 1 Incidence of positive standard patch test results at the Department of Dermatology, Stavanger University Hospital 2001 – 02; p-values refer to differences between men and women (chi square analysis)
|
|
|
|
|
|
Sex differences
|
|
|
Total
|
|
Men
|
|
Women
|
|
|
Allergen
|
n
|
Pos (n)
|
(%)
|
|
n
|
Pos (n)
|
(%)
|
|
n
|
Pos (n)
|
(%)
|
p-value
|
|
Nickel chloride 2.5%
|
834
|
330
|
(39.6)
|
|
296
|
69
|
(23.3)
|
|
538
|
261
|
(48.5)
|
< 0.001
|
|
Nickel sulfate 5.0%
|
833
|
192
|
(23.0)
|
|
296
|
28
|
(9.5)
|
|
537
|
164
|
(30.5)
|
< 0.001
|
|
Cobalt chloride 1.0%
|
833
|
93
|
(11.2)
|
|
295
|
23
|
(7.8)
|
|
538
|
70
|
(13.0)
|
0.022
|
|
Fragrance mix 8.0%
|
831
|
85
|
(10.2)
|
|
294
|
16
|
(5.4)
|
|
537
|
69
|
(12.8)
|
0.001
|
|
Balsam of Peru 25.0%
|
834
|
78
|
(9.4)
|
|
295
|
23
|
(7.8)
|
|
539
|
55
|
(10.2)
|
n. s.
|
|
Potassium dichromate 0.5 %
|
834
|
54
|
(6.5)
|
|
296
|
22
|
(7.4)
|
|
538
|
32
|
(5.9)
|
n. s.
|
|
Compositae mix 6.0 %
|
830
|
51
|
(6.1)
|
|
293
|
13
|
(4.4)
|
|
537
|
38
|
(7.1)
|
n. s.
|
|
Colophonium 20.0%
|
832
|
44
|
(5.3)
|
|
295
|
16
|
(5.4)
|
|
537
|
28
|
(5.2)
|
n. s.
|
|
Formalaldehyde 1.0%
|
833
|
43
|
(5.2)
|
|
295
|
15
|
(5.1)
|
|
538
|
28
|
(5.2)
|
n. s.
|
|
Thiuram mix 1.0%
|
833
|
27
|
(3.2)
|
|
295
|
5
|
(1.7)
|
|
538
|
22
|
(4.1)
|
0.062
|
|
4-phenylenediamine base 1.0%
|
833
|
22
|
(2.6)
|
|
295
|
6
|
(2.0)
|
|
538
|
16
|
(3.0)
|
n. s.
|
|
Quaternium 1.0%
|
833
|
17
|
(2.0)
|
|
295
|
4
|
(1.4)
|
|
538
|
13
|
(2.4)
|
n. s.
|
|
Lichen acid mix 0.3%
|
698
|
14
|
(2.0)
|
|
236
|
3
|
(1.3)
|
|
462
|
11
|
(2.4)
|
n. s.
|
|
Cl+Me-isothiazolinone 0.01 %
|
829
|
15
|
(1.8)
|
|
295
|
3
|
(1.0)
|
|
534
|
12
|
(2.2)
|
n. s.
|
|
1.2-dibromo-2.4-dicyanobutane 0.3%
|
123
|
2
|
(1.6)
|
|
52
|
2
|
(3.8)
|
|
71
|
0
|
(0.0)
|
0.096 (n. s.)
|
|
Lanolin derivative 30.0%
|
834
|
11
|
(1.3)
|
|
296
|
6
|
(2.0)
|
|
539
|
5
|
(0.9)
|
n. s.
|
|
Neomycin 20.0%
|
826
|
10
|
(1.2)
|
|
293
|
1
|
(0.3)
|
|
533
|
9
|
(1.7)
|
0.090 (n. s.)
|
|
Epoxy resin 1.0%
|
833
|
10
|
(1.2)
|
|
295
|
5
|
(1.7)
|
|
538
|
5
|
(0.9)
|
n. s.
|
|
Sesquiterpene lactone mix 0.1%
|
830
|
9
|
(1.1)
|
|
294
|
2
|
(0.7)
|
|
536
|
7
|
(1.3)
|
n. s.
|
|
Tixocortol-21-pivalate 0.1 %
|
832
|
9
|
(1.1)
|
|
294
|
4
|
(1.4)
|
|
538
|
5
|
(0.9)
|
n. s.
|
|
Quinolone mix 5.0%
|
831
|
7
|
(0.8)
|
|
295
|
2
|
(0.7)
|
|
536
|
5
|
(0.9)
|
n. s.
|
|
4-tert-butylphenol formaldehyde resin 1.0%
|
832
|
7
|
(0.8)
|
|
294
|
1
|
(0.3)
|
|
538
|
6
|
(1.1)
|
n. s.
|
|
Parabens 3.0%
|
834
|
7
|
(0,8)
|
|
295
|
5
|
(1.7)
|
|
539
|
2
|
(0,4)
|
0.045
|
|
N-Isopropyl-N-Phenyl-PPD 0.1%
|
834
|
6
|
(0.7)
|
|
295
|
3
|
(1.0)
|
|
539
|
3
|
(0.6)
|
n. s.
|
|
Budesonide 0.01%
|
818
|
4
|
(0.5)
|
|
289
|
2
|
(0.7)
|
|
529
|
2
|
(0.4)
|
n. s.
|
|
Benzocaine 5.0%
|
833
|
3
|
(0.4)
|
|
295
|
1
|
(0.3)
|
|
538
|
2
|
(0.4)
|
n. s.
|
|
Mercapto mix 2.0%
|
833
|
1
|
(0.1)
|
|
295
|
0
|
(0.0)
|
|
538
|
1
|
(0.2)
|
n. s.
|
|
Mercaptobenzothiazole 2.0%
|
834
|
1
|
(0.1)
|
|
295
|
0
|
(0.0)
|
|
539
|
1
|
(0.2)
|
n. s.
|
|
Primin 0.01%
|
833
|
1
|
(0.1)
|
|
295
|
0
|
(0.0)
|
|
538
|
1
|
(0.2)
|
n. s.
|
123/192 (64 %) patients testing positive for nickel sulfate had hand eczema and so did 192/330 of patients (58 %) testing positive for nickel chloride. But if patients with contact allergies in addition to nickel are excluded, there is no significant association between reaction to nickel sulfate or nickel chloride and hand eczema. Hand eczema is particularly common in jobs involving exposure to toxic agents: medical staff (54 of 71), farm workers (11 of 29), cleaners (22 of 27), cooks and canteen workers (19 of 25).
509/857 (59 %) of the patients tested were positive for at least one of the allergens in the standard series (e-tab 1). 425 (50 %) had contact allergy to substances other than nickel. More women than men reacted to at least one allergen (67 % versus 45 %; odds ratio (OR) 2.5; 95 % CI 1.83 – 3.23).
The most common contact allergens were metals such as nickel (in the form of nickel chloride and nickel sulfate), cobalt and chromate, perfume and perfume chemicals, balsam of Peru, Compositae (daisy, dandelion) and colophonium (e-tab 1). Allergy to several allergens affected significantly more women than men e.g. nickel chloride, nickel sulfate, cobalt chloride and fragrance mix.
Significantly fewer atopic patients had positive reactions to nickel sulfate (18 %) and nickel chloride (35 %) than did nonatopic patients (27 % and 43 %) (p = 0.002 and p = 0.015). No difference in the incidence of nickel allergy was found between patients with or without psoriasis.
341/834 (41 %) patients tested had positive reactions to nickel sulfate or nickel chloride or both. Twice as many women as men tested positive for at least one of the nickel substances (50 % versus 25 %). 181 (53 %) of the nickel sensitive patients had positive reactions to both nickel chloride and nickel sulfate; 149 (44 %) to nickel chloride alone and 11 (3.2 %) to nickel sulfate alone. The number reacting to both nickel substances was higher among women (OR 4.7; 95 % CI 2.96 – 7.38), but the number reacting to nickel chloride alone was higher among men (OR 1.9; 95 % CI 1.29 – 2.84).
61/93 (66 %) of those who tested positive for cobalt were also sensitive to nickel sulfate and 77 (82 %) of them to nickel chloride. Patients were nine times more likely to react to cobalt if they were positive for nickel sulfate (OR 8.9; 95 % CI 5.54 – 14.12) or nickel chloride (OR 9.3; 95 % CI 5.29 – 16.21). More women than men tested positive for both nickel sulfate and cobalt chloride (OR 2.7; 95 % CI 1.36 – 5.18; p = 0.004) and for both nickel chloride and cobalt chloride (OR 1.9; 95 % CI 1.10 – 3.29).
Discussion
The ten most common contact allergens for our patient group were metals such as nickel, cobalt and chromate; perfume and cosmetic chemicals such as perfume, balsam of Peru, Compositae (daisy, dandelion), colophonium and formaldehyde; and rubber and colour substances such as thiuram mix/4-phenylenediamine base. The results are commensurate with the average for the Norwegian departments of dermatology in 2005 and 2006 (5), but higher than the averages in a European study with comparable sex, age and job (4). The patch test was read only at 72 hours and not at four and seven days as is often recommended. So the number of positive reactions must be seen as minimum values. Even though the study is based on a retrospective analysis of a selected patient population, it gives information on the incidence of contact allergy in the southern part of Rogaland, where most of the patch testing is done. The strength of the reaction to an allergen and the patient’s clinical symptoms are decisive for whether a patient is allergic to a substance. The relevance of a reaction to a test substance can be difficult to determine and we have chosen our starting point to be positive reactions alone, as in other studies.
A higher proportion of our patients were positive for at least one of the allergens in the standard series than in the European study (4). The difference may be due to stricter test indications. Using the same supplier should result in a high degree of reproducibility (4, 5). Reading the test reactions is to some extent observer-dependent and some erythematous reactions are difficult to distinguish from unspecified irritant reactions. How to interpret weak reactions may vary from centre to centre, which makes any comparison difficult. The variation may also be due to the inclusion of highly specialized centres in the ESSCA report where occupational medicine and pediatric departments were also included (5).
Women were nearly 2.5 times as likely as men to react to at least one of the test substances, in particular nickel. This may be due to women being more easily sensitized to various allergens and having a stronger immune response than men (7).
Nickel is the most common cause of contact allergy in the western world (1, 4). In Norway, the number of people testing positive for nickel is higher than the average in European countries, including Denmark (1, 4). The reason may be a generally higher exposure to nickel and sensitization frequency in the population, as shown, for example, by Smith-Sivertsen et al in a population-based study in South Varanger and Tromsø (2, 7). The higher number of women testing positive for nickel, as e.g. in our study, may be because ear-piercing is more common in the female population (8). After implementation of the EU nickel directive (94/27/EEC) in 1994, several EU countries have recorded a decrease in the prevalence of nickel allergy among younger test subjects, which may explain why these countries have had a stable incidence of nickel allergy (9). The EU directive was not implemented in Norway until 1.9.2005 (10), which explains the high prevalence of nickel allergy in our patient population. We cannot draw conclusions from this study about the frequency of occupational nickel allergy because of the small number of people involved in the various jobs.
Nickel chloride is not contained in the standard series used by other Norwegian departments of dermatology or in the European centres reported in the ESSCA study. Many patients testing positive for nickel chloride did not react to nickel sulfate, but about two thirds of the nickel chloride reactions were weak (+). According to Rasanen et al, the concentrations of nickel chloride (2.5 %) and nickel sulfate (5 %) produce irritant reactions in 2.5 % (nickel chloride) and 0.9 % of the patients (11). These irritant reactions to nickel chloride may, in some cases, have been misinterpreted as weak positive reactions. Even so, a third of patients with isolated nickel chloride reactions were strongly positive (++). So, supplementary testing with nickel chloride is useful in cases of suspected nickel allergy when the test reaction to nickel sulfate is negative.
The number of patients reacting to nickel chloride alone was higher among men than women, but women reacted more often to both nickel substances. This may be due to women having a lower threshold for nickel sensitization. Men are more prone to irritant reactions, as perhaps shown in the higher incidence of reaction to nickel chloride alone (12).
The incidence of cobalt allergy at Stavanger University Hospital was higher than in the European study (4), but lower than at Rikshospitalet and Ullevaal University Hospital (5). Many alloys contain both nickel and cobalt. The high incidence of cobalt allergy among patients allergic to nickel may be due to ear-piercing, but also to cross-reactions or the contamination of test material for cobalt (13, 14).