In 2002, the ownership and responsibility for running 250 Norwegian health institutions was transferred from the county level to the state level through five regional, and 34 local, health trusts. The reform also involved new principles of organisation and management. Before the reform, the operation of hospitals was often criticised for being ineffective for various reasons including as a result of strong local political interests and county officials with little competence on health administration and health in general. After the reform, the hospitals are organised as independent legal entities with their own management boards, following the model used in business and industry. These health trusts have stated objectives for clearer division of responsibility, improved access for all, and, not least, more effective use of the available resources (1).
Under this new regime, the responsible medical professionals must, to a greater extent than previously, be answerable to professional superiors who lack medical competence. These people are often blamed for prioritising balancing the budget before ethics and professional medical opinion. Clinicians may occasionally feel squeezed between the patients” (and the authorities”) requirements for optimal professional treatment, and the leaders” and politicians” demands for control of expenses.
When the economic framework is too narrow, or the organisation of the health service is sub-optimal, professional quality and patient safety is threatened. Should such conditions arise, health personnel have a legal duty, embodied in the health personnel law § 17, to speak out. However, as the distance between clinical employees and the leadership increases, this is not always so easy. Additionally it has been pointed out that the new reform places higher demands on the employees” loyalty towards the leadership.
There are various anecdotal accounts of medical leaders who have notified their superiors about scarcity of resources and increased risk of inexcusable treatment errors, and who have had to leave their jobs at the next round, or who have had difficulties getting a new job - because an error has occurred. Unfortunately it is very difficult to document such occurrences.
This background was the basis for the present investigation on whether doctors believe that being critical may have negative consequences for them, and whether this situation has changed after the hospital reform.
Material and methods
The Research Institute of the Norwegian Medical Association has established a reference panel of about 1 600 doctors who are sent a questionnaire every other year with questions about health, work conditions, and relevant health political approaches to problems. This article is based on data from two of these questionnaires, one which was sent in 2000 to 1 616 doctors, and one which was sent to 1 497 of these same doctors in 2004. The reason for the lower number in 2004 was that 119 doctors were no longer members of the panel, mostly because they had retired. Other reasons included death or that they no longer wished to participate.
We were interested in finding out whether the hospital reform in 2002 could have affected the physicians” opinion on how easy it was to speak out about professionally unsatisfactory conditions in the workplace, a concept that we have called «professional right of voice». In order to investigate this, we used the following four expressions, which were presented both in 2000 and in 2004.
To what extent do the following expressions correspond with your work environment? (as based on your main employment position)
Those that criticise risk sanctions from the departmental superiors.
Those that criticise the hospital risk sanctions from the administrative leadership.
Those that criticise expose themselves to heavy personal strains.
Those that criticise risk needing to find another job.
The options for answering were: «corresponds well», «corresponds moderately», «corresponds slightly», «does not correspond» and «not relevant». If each answer is given a numerical value from 1 (corresponds well) to 4 (does not correspond), then a high value would represent a work environment in which it is easy to be critical. If the mean value for each statement is lower in 2004 than in 2000, this indicates that there is a negative tendency regarding openness and also that the doctors feel that their professional right of voice has been impaired. Changes from 2000 to 2004 were explored using a paired t-test.
Logistic regression was used to analyse those factors which could be associated with doctors whose opinion on each of the four statements was more negative in 2004 than in 2000. Sex, age (as a continuous variable) and professional field were the independent variables tested.
We also included two statements which were only presented in 2004:
The distance from the professional environment to the leadership and management is greater now than it was before the hospital reform.
The loyalty demand in the health trust/local authority is a threat to professional right of voice.
The answer alternatives were «yes», «no», and «don”t know».
We grouped the medical specialties into the following six subject areas: general medicine, laboratory medicine (including radiology and pathology), internal medicine fields (all specialist branches together, including paediatrics, neurology, and oncology), surgical fields (including also anaesthesia and gynaecology), psychiatry, and social medicine. Doctors who were in the process of specialising were categorised with respect to their future specialisation.
Results
In 2000, responses were received from 1 318 doctors, thus an 82 % response rate (1 318/1 616). In 2004, responses were received from 1 005 doctors, thus a 67 % response rate (1 005/1 497). A total of 897 doctors answered in both 2000 and 2004. In table 1, the characteristics of those who responded are compared with all doctors in active employment in Norway during 2004.
|
Table 1 Comparison between respondents to the questionnaire and all physicians in active employment in Norway during 2004. Physicians in the second and third columns are largely the same, with a four-year gap between data collection
|
|
Respondents in 2000(N = 1 318) with 95 % CI
|
Respondents in 2004(N = 986)1 with 95 % CI
|
Norwegian physicians in active employment in 2004 (N = 17 572)
|
|
|
Women (%)
|
32 (30 - 35)
|
33 (30 - 36)
|
35
|
|
Age (years) (mean)
|
46 (45 - 47)
|
49 (48 - 50)
|
48
|
|
Women
|
42 (41 - 43)
|
45 (44 - 46)
|
42
|
|
Men
|
48 (47 - 49)
|
51 (50 - 52)
|
51
|
|
Hospital physicians
|
|
|
|
|
Chief physicians (%)
|
21 (19 - 23)
|
32 (29 - 35)
|
30
|
|
Specialist physicians (consultants) (%)
|
24 (22 - 26)
|
5 (13 - 17)
|
20
|
|
General practitioners (%)
|
21 (19 - 23)
|
29 (26 - 32)
|
24
|
|
Others (%)
|
34 (32 - 37)
|
24 (22 - 27)
|
26
|
|
[i]
|
For all the questions there was an increase in the proportion of doctors that believed that it was difficult to speak out, and a corresponding decrease in the proportion that did not consider it to be difficult (tabs 2). For all the statements there was a statistically significant difference in the direction of less openness, particularly with respect to the statement «Those that criticise the hospital, risk sanctions from the administrative leadership» (fig 1).
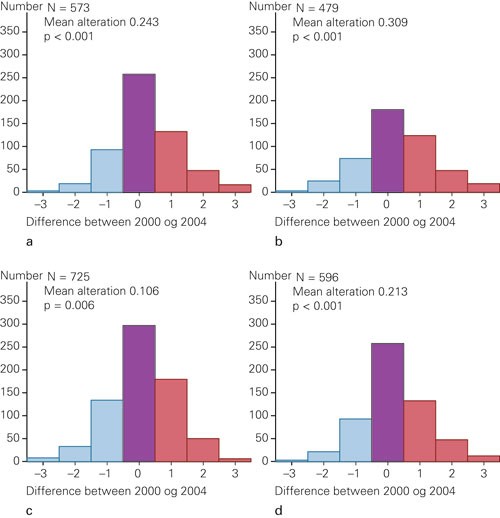
Figure 1 Distribution of the difference in values between 2000 and 2004 among respondents who answered on both occasions. A zero value (0) indicates no change, a positive value indicates that that the statement was considered to be more appropriate in 2004 than 2000, and negative values indicate that the statement was more appropriate in 2000 than 2004. The data were analysed by paired t-test, which demonstrated that the mean difference was significantly different from 0. The different numbers for those that responded to each statement meant those that responded with «not appropriate for me» are omitted. The statements were: a) Those that criticise risk sanctions from the departmental superiors. b) Those that criticise the hospital risk sanctions from the administrative leadership. c) Those that criticise expose themselves to heavy personal strains. d) Those that criticise risk needing to find another job. The alternative answers for each of the statements were: 1 - corresponds well, 2 - corresponds moderately, 3 - corresponds slightly, 4 - does not correspond, 0 - not appropriate for me (not included in the figure)
|
Table 2 The percentage (with 95 % CI) in 2000 and 2004 for the answer categories for the four statements on professional right of voice. The number of respondents is given in parentheses. The number varies because those respondents who chose the answer «not appropriate for me», are not included in the table. This table includes all the respondents, not only those who answered in both 2000 and 2004. The proportions for which there were significant changes (the confidence intervals did not overlap), are italicised
|
|
|
Corresponds well
|
Corresponds moderately
|
Corresponds slightly
|
Does not correspond
|
|
Those that criticise risk sanctions from the departmental superiors
|
2000 (951)
|
3.7 (2.6 - 5.1)
|
10.9 (9.1 - 13.1)
|
33.6 (30.7 - 36.8)
|
51.7 (48.5 - 55.0)
|
|
2004 (725)
|
10.9 (8.8 - 13.4)
|
12.7 (10.4 - 15.4)
|
32.8 (29.4 - 36.4)
|
43.6 (40.0 - 47.3)
|
|
Those that criticise the hospital risk sanctions from the administrative leadership
|
2000 (798)
|
12.7 (10.5 - 15.2)
|
23.8 (20.9 - 27.0)
|
31.7 (28.5 - 35.1)
|
31.8 (28.6 - 35.2)
|
|
2004 (621)
|
21.7 (18.6 - 25.2)
|
27.7 (24.2 - 31.4)
|
29.1 (25.6 - 32.9)
|
21.4 (18.3 - 24.9)
|
|
Those that criticise expose themselves to heavy personal strains
|
2000 (1 124)
|
23.4 (21.0 - 26.0)
|
37.9 (35.1 - 40.8)
|
23.5 (21.1 - 26.1)
|
15.2 (13.2 - 17.5)
|
|
2004 (854)
|
30.2 (27.1 - 33.4)
|
37.9 (34.7 - 41.3)
|
20.0 (17.4 - 22.9)
|
11.8 (9.8 - 14.2)
|
|
Those that criticise risk needing to find another job
|
2000 (997)
|
6.4 (5.0 - 8.2)
|
12.8 (10.9 - 15.1)
|
33.5 (30.6 - 36.5)
|
47.2 (44.1 - 50.4)
|
|
2004 (739)
|
11.8 (9.6 - 14.4)
|
17.1 (14.4 - 20.0)
|
32.9 (29.5 - 36.4)
|
38.3 (34.8 - 41.9)
|
The alteration in a negative direction was independent of the respondents” sex and there was an insignificant association with professional field (data not shown). Younger doctors had changed their opinion in a negative direction from 2000 to 2004 to a greater extent than older doctors, and this was particularly with respect to the statement that those who criticised risked sanctions from the administrative leadership.
75 % (95 %, CI 68 - 80 %) of surgeons, 69 % (95 %, CI 60 - 76 %) of psychiatrists, and 44 % (95 % CI 38 - 59 %) of general physicians were of the opinion that the distance between themselves and those in positions of leadership and management had increased since the hospital reform. Considered together, 62 % of the doctors felt that the demands for loyalty from the health enterprise/local authorities were a threat to their professional right of voice. A clear difference between professional specialties was also found here; the result for public health physicians was 49 % (95 %, CI 33 - 65 %) and that for surgeons was 70 % (95 % CI, 63 - 76 %).
Discussion
The strength of this study is its prospective design; we have been able to obtain data from the same doctors at two different time points. We do not have data to control whether any of the doctors changed their employment situation, either by altering their job within the same health trust or by moving to another. It is therefore not certain that the work environment evaluated in 2000 is the same as that evaluated in 2004. Nevertheless, should a change in employment situation have been motivated by a lack of professional right of voice, this should have resulted in an increased feeling of freedom and have the opposite effect of that found in this study.
The central theme of this research is the doctors” opinion on how easy or difficult it is to express critical points of view on «the system». We used the relatively imprecise term «criticise». This can obviously mean anything from bringing up a case in the work environment which one feels should be handled, or should have been handled in a better way, up to criticising the health service via the mass media. A previous study has shown that 50 % of Norwegian doctors believe it is difficult to complain about unethical and professionally reprehensible practice in the work environment (2). It also appears that doctors are not only apprehensive about their superiors, but also, to a large extent, find the criticism of their colleagues difficult. In our opinion it is important to differentiate between «whistle blowing» and «criticism»; whistle blowing arises first when criticism is interpreted or suppressed or when those who are criticising are opposed. Definitions of whistle blowing have included «an attempt, in good faith and in the public interest, to disclose and resolve in a reasonable and non-vexatious manner, but in the face of significant institutional or professional opposition, a significant deficiency in the quality or safety of health care» (3). A work environment in which there is little acceptance of criticism will suppress those signals which are necessary to enable improvements, and thus be a threat both to patient safety and to ethical reflection. A work environment in which there is hostility towards necessary criticism will also, according to this definition, result in a greater degree of whistle blowing, which otherwise should have been perceived as constructive criticism. Such a culture can easily cause good colleagues, who are concerned about quality and ethics, to become involuntary whistle blowers.
The fact that older doctors fear sanctions to a lesser extent than younger doctors if they speak out about unsatisfactory conditions, cannot only be because older doctors are more thick-skinned. Perhaps it is because they have more extensive experience with the health bureaucracy and endless new directors? We found that psychiatrists and doctors working in the surgical field in particular considered demands for loyalty towards the leadership to be a threat to their professional right of voice. For many years, psychiatrists have contended with increased demands and lack of resources. Many psychiatrists have a daily struggle with sub-optimal conditions; a struggle which occasionally comes up in the mass-media (4, 5).
Obviously we cannot establish that the hospital reform alone has been the reason for a deteriorating relationship of trust between doctors and administrators - this is an international trend (6). The transformation of hospitals from monolithic, doctor-managed organisations to modern, commercial enterprises began long before 2000 (7). The success criteria for such reorganisations are improved budget management, shorter waiting lists, and fewer corridor patients, that is, efficiency targets. Maintenance of, and possibly improvements in, professional and ethical standards appears to be a secondary consideration (8). This alone is an important explanation of why the experts can assert that the distance between clinical personal and the leadership has increased.
This assessment provides no information on whether the degree to which doctors” experience the risk associated with their professional right of voice reflects reality. Doctors frequently oppose changes, even changes which later have been shown to be expedient. When important decisions are taken by the administrators without medical competence, this can obviously cause frustration, although there are good grounds to assert that doctors must also respect administrative or political decisions that are not always popular, e.g. in prioritising work. In this it is important to differentiate between essential political management and loyalty requirements that that can threaten patient safety, as well as professional and ethical standards (3, 9). But the administrative leadership is dependent on good communication with the clinical leadership. The fact that many more clinicians now believe critical comments can result in sanctions, is worrying, both with respect to patients and the profession as such. Although our findings can be rebutted on the basis that they do not demonstrate genuine problems - only the doctors” interpretation of the situation - nevertheless, leaders within health services should take these signals seriously and encourage an open and continuous dialogue around difficult ethical and medical questions - a dialogue in which there is also room for criticism. And the doctors themselves should work actively to break down the concept that a culture open to criticism is not collegial (10).