Over the last 30 years there has been an increasing interest in how doctors and patients communicate, and a number of studies have given us considerable knowledge on the key elements of good communication (1). Systematic videotaping of consultations for use in counselling groups for the specialization in family medicine has been in use since the late 1980s, and this topic is also described in the basic courses in family medicine. In the specialized somatic health services, on the other hand, only the oncologists have included communication as a mandatory element in their programmes for continuing and further education.
Over a period of approximately 15 years, the American health maintenance organization Kaiser Permanente has developed a systematic training programme in clinical communication intended for specialists (2). The programme is called «The four habits approach to effective clinical communication», and focuses on training groups of skills until they turn into habits (Habit I – Invest in the beginning, Habit II – Elicit the patient’s perspective, Habit III – Demonstrate empathy, Habit IV – Invest in the end). A comprehensive course (over five days) intended for doctors with particularly poor communication skills has been shown to increase patient satisfaction (2). Even more important, however, is the observation that these doctors, who at the outset took a sceptical view of the training course, were also very satisfied and felt that they had been provided with an important tool for their work.
In August 2006 we implemented a three-day pilot course that conformed to Kaiser Permanente’s approach with 16 Norwegian participants and three American and three Norwegian instructors. The course showed that this training programme, which in Norwegian has been given the title «Fire gode vaner» («Four good habits»), with some adjustments also could benefit Norwegian hospital doctors (3). Kaiser Permanente’s basic programme for new doctors provides 12 hours of training. We chose to implement a 20-hour course over two days, as we felt that this would be acceptable for the hospital management as well as the participants.
The course model was tested in a randomized, controlled study undertaken at Akershus University Hospital in April 2007 – June 2008. The main objective of the study was to find out whether a course of this type would be sufficient to induce behavioural change, and this was studied with the aid of video analyses of consultation behaviour. These results will be published at a later time.
In the context of the implementation of the course, we surveyed the doctors’ own experiences and views with regard to the confidence they had in their own clinical communication skills both prior to and after the course. The purpose of this sub-study is to investigate the extent to which the doctors’ confidence in their own skills changed during the course.
Material and methods
Among the 249 doctors aged 60 or younger who were employed at Akershus University Hospital as of 15 February 2007, a statisticianrandomly selected 80 for inclusion in the study, stratified by 16 departments (anaesthetics/emergency, paediatrics, endocrinology, gastro-surgical, gastro-medical, gynaecology/obstetrics, haematology/oncology, coronary, infectious medicine, vascular/thoracic, pulmonary, neurology, nephrology, orthopaedics, urology, otorhinolaryngology) and by positions (chief consultant, doctor in internship). In addition, another 51 doctors were selected as replacements if someone were incapable or unwilling to participate. The doctors were randomly assigned to courses held during the summer of 2007 and the winter of 2008, and received training in groups of 4 – 7 participants, as well as in plenary sessions of up to 16 participants.
Three of the course instructors had varying previous experience from communication training and had served as assistant teachers during the pilot course, the three assistant instructors were familiar with the training programme after having participated in it previously. The six instructors spent one full day jointly preparing for the role of course teachers.
A total of 20 hours of training was provided over two days. Approximately half of the training consisted of plenary sessions, the other half took place in groups. Table 1 provides an overview of the topics. Upon arrival, the participants completed a questionnaire (4). This questionnaire contained the question: «Do you believe that one can improve one’s communication skills by participating in a training course?» Response alternatives were «to a great extent», «to some extent», «to a little extent», «not at all» and «don’t know». The doctors’ confidence in their own ability to master specific communication skills (self-efficacy) was measured by the question: «How certain are you that you can successfully perform the following tasks?» in which responses should be given on scale from 1 (very uncertain) to 10 (very certain) with regard to the issues in Table 2. A corresponding questionnaire was completed immediately after the course. The questionnaires were collected by a secretary, but it is unlikely that the participants considered their responses as anonymous, since there were a limited number of participants in each course. In the final session of the course, the participants were requested to describe and identify which habit(s) among the four they would emphasize in the period following the course.
|
Table 1 Overview of topics in the course programme «Four good habits» in clinical communication
|
|
Mutual presentation and review of the participants’ expectations and scepticism to the course(1 hour)
|
|
Discussion of a video scene from a feature film (1/2 hour)
|
|
History, overview of the four good habits, documentation of effects of good communication.(1 hour)
|
|
The first habit – Invest in the beginning! (2 hours, whereof 1 hour role-play in small groups)
– Main elements: How to establish good contact, how to elicit all the patient’s concerns, planning the rest of the consultation
|
|
The second good habit – Elicit the patient’s perspective! (2 hours, whereof 1 hour role-play in small groups)
– Main elements: What are the patient’s conceptions of his/her condition/symptoms, how do they affect daily life, what are the patient’s expectations of what the doctor can do
|
|
– Main element: The doctors address their own emotions in a personal narrative
|
|
The third good habit – Demonstrate empathy! (21/2 hours, whereof 1 hour role-play in small groups)
– Main elements: How to become aware of and respond to the patient’s emotions, how to prepare the ground for turning them into a topic when required, awareness of one’s own reactions and behaviour patterns
|
|
The fourth good habit – Invest in the end! (2 hours, whereof 1 hour role-play in small groups)
– Main elements: How to provide information and link it to the patient’s perspective, how to make sure that the information has been understood, how to make sure that the patient follows up the treatment, how to end the consultation
|
|
Training according to the participants’ wishes (11/4 hour of role-play in small groups)
|
|
Motivation for further training, summing up, review of what has been learned, follow-up (1 hour)
|
|
Table 2 The participants’ responses to the question : «How certain are you that you can successfully perform the following tasks?», ranked on a scale from 1 (very uncertain) to 10 (very certain). Averages (standard deviations). N = The number of participants who responded to the question before and after the course.
|
|
N
|
Before the course
|
After the course
|
Change
|
P-value
|
|
Initiate a conversation with a patient regarding his/her concerns
|
60
|
7,50 (1,37)
|
8,03 (1,18)
|
0,53
|
< 0,001
|
|
Conclude a consultation with a summary of the problems and a treatment plan
|
61
|
7,52 (1,41)
|
7,98 (1,23)
|
0,46
|
0,003
|
|
Assess symptoms of anxiety and depression
|
60
|
5,82 (1,74)
|
6,07 (1,58)
|
0,25
|
0,149
|
|
Communicate bad news to a patient
|
60
|
6,47 (1,81)
|
6,98 (1,69)
|
0,52
|
0,001
|
|
Confront in an appropriate manner a patient who denies his/her illness
|
61
|
5,61 (1,68)
|
6,15 (1,58)
|
0,54
|
0,015
|
|
Cope with a situation in which a patient or a relative expresses disagreement with you as a doctor
|
60
|
6,25 (1,71)
|
6,53 (1,68)
|
0,28
|
0,166
|
|
Encourage a patient to describe his/her feelings
|
59
|
6,51 (1,44)
|
7,17 (1,51)
|
0,66
|
0,003
|
|
Explore intense emotions, such as anger, in a patient
|
61
|
5,03 (1,86)
|
6,28 (1,57)
|
1,25
|
< 0,001
|
|
Help a patient cope with an uncertain situation
|
61
|
6,48 (1,63)
|
7,15 (1,35)
|
0,67
|
0,004
|
A frequency analysis of the responses was made. Statistical comparisons of the averages were done using t-tests for paired observations.
Results
Of the 80 doctors selected, 21 of 26 (14 who declined to participate, 12 who were unable) were replaced (five doctors could not be replaced because of the stratification). Of the 21 substitutes, another two declined and three were unable to participate. Two of these could be replaced so that a total of 72 doctors were included in the study, whereof 56 formed part of the original sample. Later it turned out that ten of these could not receive the intervention (four because of their workloads, two because of sickness of their children, one because of illness, one because of paternity leave, one because of appointment to a new position and one because of other mandatory training that could not be rescheduled), so that 62 doctors underwent the training programme. Table 3 shows the characteristics of the participants. The distribution according to gender, type of position, age and specialization in the sample that underwent the intervention is not significantly different from the total population from which the sample was drawn.
|
Table 3 Distribution by age, gender, group of specialization, type of position and previous experience from communication training among the participants and the population from which they were sampled
|
|
Hospital doctors in total (N = 249)
|
Participants (N = 62)
|
|
Number (%)
|
Number (%)
|
|
Age
|
|
40 years or younger
|
138 (55)
|
35 (56)
|
|
Older than 40 years
|
111 (45)
|
27 (44)
|
|
Gender
|
|
Women
|
98 (39)
|
28 (45)
|
|
Group of specialization (incl. internships)
|
|
Internal medicine
|
81 (33)
|
23 (37)
|
|
Surgery (incl. anaesthetics/emergency, orthopaedic, otorhinolaryngological
|
95 (38)
|
17 (28)
|
|
Neurology
|
26 (10)
|
8 (13)
|
|
Paediatric
|
27 (11)
|
7 (11)
|
|
Gynaecology/obstetrics
|
20 (8)
|
7 (11)
|
|
Type of position
|
|
Chief Consultant
|
130 (52)
|
32 (52)
|
|
Internship
|
119 (48)
|
30 (48)
|
|
Previous communication training
|
|
Number having taken such courses
|
–
|
17 (27)
|
|
– Whereof after medical school
|
–
|
2 (3)
|
The training course changed the participants’ views on whether it is possible to learn to communicate with the aid of this type of training in a positive direction and to a statistically significant extent (fig. 1). The proportion who believed that these skills could be improved to a high extent increased from 19 % prior to the course to 36 % after the course, while the proportion who had little faith in such training courses (the sum of «to a little extent», «not at all» and «don’t know») declined from 16 % to 3 %. Two doctors had taken a much more positive and 16 doctors had taken a somewhat more positive view, while 40 doctors had not changed their minds. We have no data for four doctors.
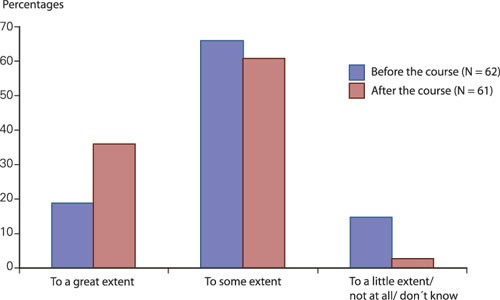
Figure 1 The participants’ responses to the question «Do you believe that one can improve one’s skills in communicating with patients by participating in a training course?» Percentages.
The course also changed the participants’ perception of how well they could cope with seven of the nine tasks they were asked to describe, to a statistically significant extent (tab. 2). This applied irrespective of how the doctors assessed their skills prior to the course. This improvement also did not correlate with whether the doctors initially had considerable, medium or little confidence in the effectiveness of the training course. Neither could we detect any differences associated with the training groups in which the doctors had participated.
We estimated the total change in self-efficacy for each doctor by adding the values for the nine skills prior to and after the course. A total of 41 doctors had improved, and ten had reduced their self-efficacy. We found no differences associated with gender or age group, nor could we detect any significant differences associated with specialization, but these groups are very small. Four of the five who reported the greatest reduction of their self-efficacy were surgeons. The doctors whose self-efficacy was reduced reported the same positive change in their views on the possibility of learning to communicate with the aid of a course of this type as the doctors whose self-efficacy was enhanced. Of the 62 doctors, a total of four did not wish to practise any of the four habits in particular after the course. Of the other a total of 37, 33, 20 and 27 doctors wished to practise Habit I, Habit II, Habit III and Habit IV respectively.
Discussion
This is the first study which has attempted to include a representative sample of hospital doctors from all somatic disciplines, trained specialists as well as doctors in internships, in a general training programme in clinical communication. The rate of attrition was limited (well under 20 per cent), and did not affect the distribution by gender, age, type of position and specialization to any significant extent. With regard to representativeness we regarded it as positive that nine of the participants (15 per cent) had weak, negative or indifferent expectations to the benefit to be gained from the course, since it is unusual for less motivated doctors to participate in this type of studies at all.
The questionnaire on self-efficacy has been used in the context of communication training for oncologists and is not especially intended for «Four good habits». We chose to use this questionnaire since the skills examined are relevant in many different situations, because the characteristics of the questionnaire have been tested, and because the training programme teaches general communication skills. Of the skills that were surveyed, only how to initiate and end the conversation and how to encourage discussion and exploration of emotions (such as anger) were practised in all the groups. Many groups also practised how to report bad news. On the other hand, no groups specifically practised how to detect serious anxiety or depression. The differences in the changes among the indicators are a sign that the group training may have had an effect, and that the doctors have made assessments of the substance of each item in the questionnaire separately. In terms of the study’s validity, it can be argued that the doctors have been prone to provide positive feedback out of regard for the instructors, or because they could not rely on remaining anonymous.
Most doctors reported an improved self-efficacy after the completion of the training course. However, the average change constituted less than half of the 1.3 points that were observed in a Danish study of doctors and nurses in a paediatric department, in an intervention that lasted for five days (5). Even though the change detected by us is statistically significant, the implications of this change remain uncertain. A sense of self-efficacy increases well-being on the job, and it has been shown that patients’ compliance with the treatment is positively correlated with the doctors’ well-being in their job (6). Ten of our doctors reported feeling less self-efficacious after the completion of the training course. This notwithstanding, they came out of the course with a more positive attitude to its learning effect than they had at the outset. In the oral evaluation session, three of the five doctors who reported the largest negative change expressed that the course had made them aware of a number of aspects of their own way of communicating, and that they perceived this as highly useful. A negative change in the perception of self-efficacy may be related to the realization of a need for improvement. Such realizations are motivating, and it would be likely to have a beneficial effect if these doctors could be given some follow-up, for example in the form of feedback based on video recordings.
Kaiser Permanente has experienced that weakly motivated doctors have welcomed «Four good habits». We find that doctors with low expectations or low initial self-efficacy perceive an equally positive change in their self-efficacy as doctors who enter the course with high expectations and high self-efficacy. Similarly we find no differences related to age or gender, or to whether the doctors are chief consultants or interns. This indicates that the level and methods applied in the course are generally useful. It would also appear that they function well across specializations, although this result should be given less emphasis, since each group consisted of relatively few doctors. We wish to underscore that an effect on self-efficacy does not necessarily imply a subsequent change in behaviour. Our findings indicate that the doctors perceived that they had benefited from the course irrespective of such factors, but it remains to be seen whether this has entailed any changes in behaviour.
Empathy, Habit III, was the habit that the fewest doctors reported they wanted to practise after returning to clinical work after the training course. We can imagine a number of causes for this observation. Many doctors expressed that they felt confident about their abilities in this respect. Others also noted that they often would refrain from discussing emotional aspects to prevent the consultation from taking too much time. The course, on the other hand, emphasizes that even small demonstrations of empathy may have a positive effect, and only rarely entail a loss of time. However, this habit is less instrumental than the others, and it may well be that we succeeded to a lesser extent in creating convincing role-play situations for this habit than for the other ones.