Patients on drug-assisted rehabilitation have the same right to pain relief as others. Techniques that reduce the need for opioids should be used when possible in opioiddependent individuals who need treatment of acute and post-operative pain. Substitution treatment should always be continued. In some situations a switch to a different opioid or route of administration is required. Higher doses of opioids than those needed in other patients may be required for analgesia. Well-designed clinical studies are lacking in this field.
Treatment of acute pain in patients on opioid maintenance therapy (OMT) represents challenges for both doctor and patient. The patient may fear acute pain as well as abstinence symptoms. There are many misconceptions among doctors about the treatment of pain in this patient group (Table 1) (1).
|
Table 1 Common perceptions among healthcare staff about pain treatment for patients in medication-assisted rehabilitation (OMT) (1)
|
|
Perception
|
Comment
|
|
OMT patients who are receiving opioids get pain relief from these opioids.
|
Opioids that are correctly dosed for OMT patients do not alleviate pain. The dose is titrated to provide sufficient receptor stimulation to avoid abstinence. There are no opioids «left over» that can relieve pain.
|
|
The combination of OMT opioids and opioids for pain relief results in a high dose, which poses a considerable risk of respiratory depression.
|
These patients have developed a tolerance for opioids that includes a tolerance for respiratory depression. If opioids that are used for pain are titrated in an appropriate manner, the risk of respiratory depression is no greater than it is for other patients with acute pain, even though the total dose is higher.
|
|
The use of short-acting or intravenous opioids in pain treatment can intensify the craving for intoxicants and can trigger abuse.
|
Partly correct. However, there is more reason to believe that the under-treatment of acute pain will lead to patients trying to get hold of opioids themselves to alleviate the pain. Such self-medication will probably entail a greater risk of triggering new abuse.
|
|
Patients manipulate the situation in order to experience the intoxicant effect of opioids.
|
For patients with post-operative pain or obvious injury, staff should rely on the reports of pain being genuine. The patient must be examined, and there must be concurrence in the clinical picture. Acute pain is always accompanied by stress symptoms.
|
The main prerequisites for the successful treatment of acute pain among OMT patients are a good relationship between the patient and the treating staff and realistic expectations on the part of the patient. He/she must be informed that no patient can expect a total absence of pain after surgery or injury. At the same time it must be made clear that the planned treatment is intended to minimise pain and to prevent both abstinence symptoms and a reduction in the ability to cope with intoxicants. Postoperative pain is normally asessed using a numeric or visual rating scale for pain intensity. Such asessment will also be important for OMT patients, but pain scores can be affected by anxiety, agitation and abstinence.
Material and method
The article is based on other relevant articles, identified by a non-systematic search in PubMed and selected on the basis of personal judgement and the authors’ clinical experience.
General considerations
Unless they are contraindicated, non-opioid analgesics should always be used in the same way as for other patients when treating acute and postoperative pain, i.e. paracetamol and non-steroidal antiinflammatory drugs (NSAIDs). These medicines alone will most often provide adequate relief for moderate pain. Paracetamol is contraindicated in patients with acute hepatitis, while patients with moderate chronic liver affection can take paracetamol in normal therapeutic doses. A single dose of steroids can also provide better postoperative pain relief.
When treating moderate to severe pain, the choice is usually between treatment with opioids and regional anaesthesia/infiltration anaesthesia. Treatment with ketamine in sub-anaesthetic doses – for example 1 mg/kg/24 hours subcutaneously – may also be a possibility in special cases. In other patient populations, low-dosage ketamine has been found to have an opioid-saving effect with little risk of psychomimetic side effects (2). When using a catheter for epidural analgesia or for peripheral blockades, a continuous infusion or repeated doses of local anaesthetic can be given. Figure 1 shows an algorithm for the choice of postoperative pain treatment for OMT patients. If a regimen without opioids is chosen, it must be borne in mind that the patient still needs his/her usual substitution dose of opioid to avoid abstinence symptoms. If the route of administration for the substitution dose has to be changed, in most cases it will also be necessary to change the dose or the opioid.
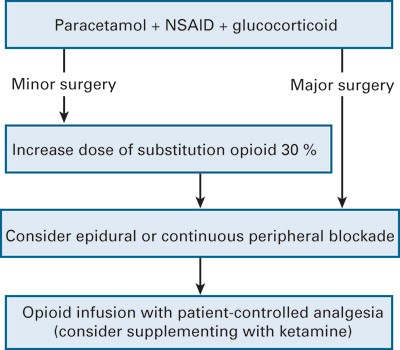
Figure 1 Postoperative pain treatment for patients in medication-assisted rehabilitation
When treating pain with opioids, using a pump with a combination of continuous infusion and bolus doses may be preferable to giving bolus doses alone. Medication from a pain pump can be given intravenously or as a subcutaneous infusion. Intravenous administration is easier to titrate, whereas subcutaneous infusion causes slower changes in the serum concentration and therefore presumably less sense of intoxication from the bolus doses.
Premedication with benzodiazepine or opioids should not routinely be given to OMT patients. Indications for premedication with benzodiazepine are intense anxiety and agitation. Several of the authors have experienced that the sedative effect of opioids can also be used to reduce anxiety and agitation before surgery. It is not clear how high the threshold should be for administering such premedication, but the majority of the authors support a restrictive policy.
Methadone
Methadone is a synthetic opioid which is mainly used in OMT for opioid abusers, but it is also utilised in the treatment of pain in the event of poor response to the usual first-line opioids. Methadone mixture is most used in substitution treatment, while tablets are most used for pain treatment. Methadone injection fluid for intravenous use can normally be procured via the pharmacy in two days or so. The half-life of methadone varies from 7 to 65 hours, while bioavailability on oral administration is usually 70 – 80 %.
The long and variable half-life makes it particularly difficult to dose methadone. Overdosing is a hazard because acumulation may cause rising serum concentration even several days after an increase in dose. The inter-individual variations in bioavailability also contribute to making it difficult to estimate the equivalent dose when switching from enteral to parenteral administration. Methadone mixture usually produces maximum concentration in the blood within two hours. The typical substitution dosage of methadone is 70 – 150 mg daily as a single dose. When treating pain, methadone must be given three times a day (2 – 4 times). A case has been reported where methadone had to be administered every second or third hour for postoperative pain (9).
In the event of acute pain, if a decision is taken to increase the patient’s dose of methadone substantially, an ECG should be considered to assess the increase in QTc time. The threshold for taking an ECG should be low but dependent on the patients’ other risk factors for arrhythmia, such as electrolyte imbalances, cardiac disease and drug interactions.
Carbamazepine and a number of antibiotics and psychopharmaceuticals may lead to an increase or a reduction in the methadone concentration through induction or inhibition by CYP enzymes (4). In spite of reports of the successful use of methadone for breakthrough pain, a short-acting opioid will be preferable to methadone in a phase of relatively fast titration of the opioid to effectiveness in the immediate postoperative phase.
Buprenorphine
Buprenorphine is used in two forms for OMT patients: either alone (Subutex) or in combination with naloxone (Suboxone). Buprenorphine is a partial opioid agonist/antagonist. Due to the absence of a full agonist effect, there is a ceiling effect when high doses are given. This ceiling effect has been well documented for subjective opioid effects such as euphoria and respiratory depression. A similar definite ceiling effect has not been demonstrated for pain alleviation (5, 10).
Strong receptor binding means that buprenorphine in high doses can also block the effect of other opioids.The normal dosage of buprenorphine for OMT patients is 8 – 24 mg a day. Since buprenorphine is a partial antagonist, morphine and other opioid agonists may have a poor analgesic effect when these patients suffer from acute pain. Due to the uncertainty related to the ceiling effect, patients who are being treated with buprenorphine are usually «rotated» to the pure opioid agonist methadone prior to major surgery. However, this creates uncertainty, and is particularly difficult to carry out before emergency operations. In some hospitals it has been decided to use morphine as both substitution and pain treatment.
An alternative is to use buprenorphine for postoperative pain treatment. One study has reported the effect of buprenorphine/naloxone tablets dissolved on the tongue as needed for postoperative pain for patients who were initially being treated with 24 mg buprenorphine/6 mg naloxone daily (3). Morphine has also been reported to be effective for postoperative pain after emergency surgery on patients who were being treated with 16 mg/day of buprenorphine (6). Since changing between different opioids always entails a risk of under-treatment or overdosing, it will often be simplest and best to avoid changing opioids in patients who are being treated with buprenorphine. Several of the article authors have had positive experience of treating acute pain in this patient group with supplementary doses of buprenorphine. Moreover, in the event of acute injury and emergency surgery it will not be possible to carry out a planned conversion to other opioids. Routines must therefore be in place for the treatment of acute pain in patients who cannot be changed from buprenorphine to another opioid.
Outpatient surgery
After outpatient surgery, mild or moderate pain can most frequently be treated with non-opioid analgesics alone. However, long-term use or abuse of opioids may lead to increased pain sensitivity. These patients may therefore need opioids after surgery for which such medication is usually not required.
If pain treatment with opioids is necessary after discharge, the easiest procedure will be to increase the dose of the opioid that is used in the OMT treatment. A suitable dosage increase will usually be 20 – 30 %. To attain a stable serum concentration, the supplementary dosage should be divided into 2 – 3 doses, one being administered together with the substitution dose and the other(s) at intervals of twelve or eight hours. In some places the custom is also to divide the substitution dose when the dosage is increased to relieve pain. The two methods of dividing the total dosage have not been compared in clinical trials. The dosage should be regulated in cooperation with the OMT doctor to ensure that it is both safe and effective. An appointment should be made for a follow-up consultation with the OMT doctor or primary doctor as soon as possible after discharge.
Major surgery
Regardless of the choice of anaesthetic technique, on the day of the operation the patient should usually be given the substitution dose in the morning (8). If possible infiltration anaesthesia, peripheral blocks or epidural anaesthesia should be used to reduce the need for opioids. If satisfactory pain relief cannot be attained with such procedures, the pain should be treated in the usual way with intravenous opioids, preferably in a combination of continuous infusion and bolus doses. These patients may need higher doses than other patients. For example it has been reported that after a caesarean section, female OMT patients need 70 % higher opioid doses than other patients postoperatively (7). The change from intravenous to peroral administration of the opioids should be made as soon as possible. Even though emergency surgery may have allowed less time for planning the postoperative pain treatment, the advice given for elective surgery should be followed as far as possible.
General anaesthesia – special points
Because OMT patients have developed tolerance to opioids they can be expected to require higher opioid doses for induction of anesthesia compared to other patients. Opioids should be titrated to effect. Maintaining anaesthesia with opioids will be more difficult due to tolerance and hence a higher risk of per-operative stress. It can also be assumed that there will be an increased risk of unintended awareness during general anaesthesia for muscle-relaxed patients, particularly if total intravenous anaesthesia (TIVA) has been chosen. Consequently a gas-based anaesthesia will usually be recommended.
Acute pain in patients outside hospital
Acute pain that does not give rise to suspicion of a condition that requires hospitalisation should preferably be treated with non-opioid analgesics. If this does not alleviate the pain adequately, the daily dose of the substitution opioid can be increased by 20 – 30 %, divided into 2 – 3 doses per day. The patient’s primary doctor should regulate this together with the OMT doctor. The patient should agree on when and how the dose is to be reduced to the usual maintenance dose.
In the very few exceptions where a doctor other than the patient’s primary doctor – for example the A&E duty doctor – finds indications for treatment with opioids for acute pain, it will often not be possible to procure extra doses of the opioid that is used in the OMT treatment. The alternative will primarily be other opioid tablets, but an opioid patch can be a supplement if the pain is expected to last for some days or weeks.
In principle, all formulations of all opioids – including opioid patches – can be abused to attain intoxication. Tablets that contain codeine-paracetamol, morphine and oxycodon are in particular used for this purpose. Pethidine suppositories can probably be recommended instead: we are not aware of any reported abuse of this drug. If possible a procedure should be set up that allows the patient’s intake of tablets to be observed, but staff must bear in mind that tablets can be regurgitated or hidden away even when their intake is observed. When patches are used, consideration must be given to the time required for the patch to produce an effect. Treatment with tablets may therefore be necessary while waiting for the serum concentration to provide pain relief.
The patient should not be given «loose» patches to take home. Any change of patch should be carried out by the same person each time, preferably the patient’s primary doctor or OMT service staff. Signing and dating the patch may make it easier to detect abuse. If the pain treatment with opioids is started outside the hospital by a doctor other than the primary doctor or the OMT doctor, only medication for the period up to the next working day should be prescribed or dispensed. It will often be sufficient to give one tablet under supervision and to issue the patient with 1 – 2 tablets to last until the following day. The patient must then contact his/her primary doctor or the OMT doctor to draw up a plan for the duration and reduction of the opioid treatment. In most cases the primary doctor or the OMT doctor should increase the dose of the substitution opioid rather than continuing the treatment with another opioid in addition to the substitution opioid.
Collaboration between the hospital, primary doctor and OMT doctor
Prior to elective surgery with anticipated postoperative pain that will require opioids, the surgeon, anaesthetist and OMT doctor should together plan the postoperative pain treatment. It is important to establish good local procedures. In the event of hospitalisation for emergency surgery or following acute injury, the doctor at the hospital department in question should contact the OMT doctor to plan optimal pain and maintenance treatment during hospitalisation and on discharge. This usually means that on discharge the patient is treated with an increased dose of methadone or buprenorphine, divided into 2 – 3 daily doses. If the patient is treated with opioids on discharge, an appointment should be arranged with his/her OMT doctor or primary doctor 1 – 2 days after discharge for further dose reduction and follow-up.