It has been documented for 70 years that electroconvulsive therapy (ECT) is effective in the acute treatment of major depression (1). The treatment is based on experience, and the mechanism of action has been uncertain, but recent research shows an increase in the nerve cell growth factor and in the volume of the hippocampus (2). The therapy is continuously being modified to reduce acute side-effects, while long-term side-effects have not been documented until recently (3, 4). After 1958, many thought that use of this type of treatment would cease because psychotherapy and new drugs would take over as the main methods of treatment together with milieu therapy and sociopsychiatric measures. Studies have shown that ECT has regained popularity in severe diseases where other methods fail (5). During the last 20 years ECT has been considerably improved as regards safety and technique, including routine use of ECG and EEG monitoring. It has been maintained that this method should be used early in depression that is life-threatening and graded as psychotic (6, 7). Delusions and psychomotor retardation in the severely depressed are strong clinical predictors of response (8). In Norway, ECT is used relatively seldom, but has been used increasingly in recent years. For example, at the turn of the century, Oslo University Hospital used this treatment in about 20 patients per 100 000 inhabitants compared with only three in 1988 (9).
Several studies have shown that electroconvulsive therapy in major depression gives a better and quicker response than antidepressant drug therapy (10). A rapid response is important if there is a great danger of suicide. Most treatment algorithms for depressive mood disorders recommend starting with at least two trial courses of treatment with drugs, each lasting 6 to 8 weeks, with a possible exception when treating life-threatening depression. However, the question is whether months of suffering can be shortened by starting ECT earlier (11). On the other hand, there is still uncertainty about possible permanent side-effects. Although the study design cannot document permanent damage to memory, we decided to investigate indications, registered efficacy, and possible side-effects of ECT given over 36 years at Dikemark Hospital.
Material and method
Dikemark was Norway’s largest psychiatric hospital until Oslo psychiatry was reorganised in 1996. The hospital admitted adult patients from Oslo. Some patients were referred directly, while in the case of others who showed insufficient improvement, an application for transfer for further treatment was sent by psychiatric clinics. At three departments, one general psychiatric and two gerontopsychiatric units, separate protocols were kept, and all the ECT treatments in these departments between 1960 and 1995 inclusive were included in the material. In the hospital’s other four departments this form of therapy was only given very rarely here, and no protocol was available.
We also present data for the inpatients who received ECT during the period 1955 – 59. Protocols were not kept before 1960, so the figures for the years 1955 to 1959 have been taken from the hospital’s annual reports. The number of patients admitted to the hospital during various years was taken from the annual reports. The study is naturalistic and retrospective, and it has been possible to assess the benefit gained by the patients during the first four weeks after the ECT on the basis of information in the case records. The investigation is part of quality assurance.
A Siemens Convulsator with sine wave stimulation was used in 80 % of the courses. After 1992, the new Thymatron apparatus with brief pulse stimulation was used. The treatment was given three times a week. The ECT procedure has been described previously (9).
Assessment of the diagnosis, effect of treatment, and side-effects were based on the first author’s systematic scrutiny of the whole hospital medical record, including the application for admission, the doctors’ notes, discharge reports, and the daily reports by the milieu personnel that were written at least three times a day. Different systems of diagnosis were used during these 36 years. The first author has re-diagnosed all the patients using ICD-10. Standardised tests for improvement based on the Montgomery-Aasberg Depression Rating Scale (MADRS) were only used unsystematically, starting in about 1992, while symptoms, functional improvement and clinical assessments were described in the continuous case record or discharge summary. The clinical efficacy of the first course was assessed and documented in all the medical records. In only one record was it not possible to assess the efficacy of a later course.
Improvement was classified as follows:
Much improved: regaining the premorbid functional level with full remission of symptoms, leading to discharge from hospital within four weeks.
Improved: improvement of symptoms and functional level, but with residual symptoms making it impossible to discharge the patient from hospital in the course of the first four weeks.
Unchanged: no improvement in clinical condition or functional level.
Worse: exacerbation of symptoms or functional level within four weeks after treatment.
Much worse: considerable exacerbation of symptoms or functional level within four weeks after the treatment.
The time when the first signs of improvement after ECT were noted in the patient’s record was registered. The same applied to all forms of discomfort, side-effects, or complications of the treatment, registered during the first four weeks after the therapy.
The reliability of the diagnoses, scoring of effect and side-effects was tested by selecting at random 22 case records which were reviewed independently by the second author. Kappa statistics were used. The kappa value for diagnosis was 0.84 (95 % KI 0.55 – 1.00). The weighted kappa value for effect was 0.64 (95 % KI 0.33 – 0.95). The kappa value for side-effects was 0.83 (95 % KI 0.55 – 1.00).
Statistically significant differences were calculated using a two-tailed Fisher test. The statistically significant difference was defined as p < 0.05.
Ethics
The study was approved by the Privacy Protection Representative at Oslo University Hospital.
Results
Between 1960 and 1995, 241 courses of therapy were given to 141 individuals, an average of 1.7 courses to each patient. In total, 1960 treatments were given, an average of 8.1 treatments per course. From 1955 to 1995, 7.7 % of the patients admitted to hospital received this treatment. From 1960 to 1979, the treatment was little used, and only given to 0.3 % of those admitted. From 1980 to 1989 the use was increasing, and 1 % were given this treatment, increasing to 1.7 % in 1990 to 1995 (Fig. 1). 74 % were women, 53 % of all the patients were married, 19 % unmarried, 17 % widows/widowers, and 9 % were separated or divorced. The majority were in the age group 60 to 79 at their first treatment with ECT. The age range was from 29 to 87 years, with an average of 64 years (SD = 10.9). The average age at the first depressive episode was 52 years (4 – 85 years). Of 124 patients with major depression as their main diagnosis, 93 (75 %) had the psychotic type of depression. In 136 patients (96 %), at least one comorbid somatic condition was registered. These patients had an average of 4.8 comorbid somatic conditions in addition to depression. Cardiovascular, urogenital and musculoskeletal disorders were most common (Table 1).
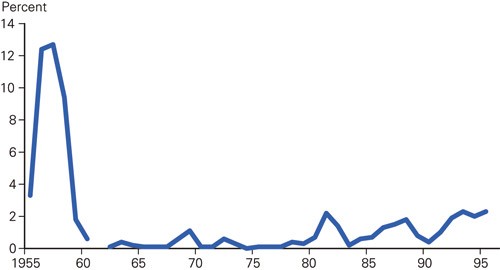
Figure 1 Percentage of inpatients in Dikemark Hospital who received electroconvulsive therapy in the period 1955 – 1995 (the percentage for 1961 is not available)
|
Table 1 Number of patients with somatic comorbid diseases (%) (n = 141)
|
|
No.
|
(%)
|
|
Cardiovascular
|
77
|
(54.6)
|
|
Musculoskeletal
|
74
|
(52.5)
|
|
Urogenital
|
71
|
(50.4)
|
|
Gastrointestinal
|
46
|
(32.6)
|
|
Respiratory
|
44
|
(31.2)
|
|
Connected with nervous system
|
42
|
(29.8)
|
|
Endocrine
|
32
|
(22.7)
|
|
Connected with sensory organs
|
31
|
(22.0)
|
|
Related to skin
|
31
|
(22.0)
|
|
Haematological
|
16
|
(11.3)
|
|
Allergic
|
7
|
(5.0)
|
|
Others
|
3
|
(2.1)
|
|
Liver
|
2
|
(1.4)
|
Only 12 patients (9 %) were admitted for the first time. A third of the patients had more than five previous admissions to a psychiatric department. 129 (91 %) of all the patients had tried antidepressant drugs for a long period. 107 (76 %) had used at least two different antidepressants, 67 (48 %) had tried at least two different classes of drug, and 31 (22 %) had tried lithium alone or in combination. A total of 52 (37 %) had received ECT previously.
Result of the first ECT course (n = 141)
Table 2 shows that in 14 % the condition of the patients was unchanged, while 85 % improved in the course of the first four weeks after the first ECT course.
|
Table 2 Effect of electroconvulsive therapy registered during the first four weeks after the first and later courses of treatment at Dikemark Hospital 1960 – 95 (n = 241)
|
|
First course
|
|
Later courses
|
|
No.
|
(%)
|
|
No.
|
(%)
|
|
Much improved
|
61
|
(43.3)
|
|
39
|
(39)
|
|
Improved
|
59
|
(41.8)
|
|
48
|
(48)
|
|
Unchanged
|
20
|
(14.2)
|
|
9
|
(9)
|
|
Worse
|
1
|
(0.7)
|
|
3
|
(3)
|
|
Much worse
|
0
|
–
|
|
0
|
–
|
|
Unknown
|
0
|
–
|
|
1
|
(1)
|
|
Total
|
141
|
(100)
|
|
100
|
(100)
|
Table 3 shows the registered effect in patients with different diagnoses. Most had recurrent major depression with delusions and risk of suicide. A total of 64 (45 %) had made at least one attempt at suicide. Nine had an organic brain disorder as their main diagnosis, while five had schizophrenia and three had schizoaffective disorder. Major depression was the indication for ECT in these 17 patients. 30 (21 %) had bipolar depression. Of the 124 with a primary diagnosis of an affective disorder, 93 (75 %) had psychosis, classified as F31.50, F32.30 and F33.30 in ICD 10. In this group, the condition was registered as improved in 84 (90 %). All eight patients with depression in schizophrenia or schizoaffective disorder (F20 – 25.2) improved, and three of these were registered as much improved.
|
Table 3 Effect of electroconvulsive therapy with different diagnoses registered in the course of the first four weeks after treatment at Dikemark Hospital 1960 – 95 (n = 141)
|
|
Major depresssion with psychosis
|
|
Major depresssion without psychosis
|
|
Organic brain disorder
|
|
Schizophrenia/schizoaffective
|
|
Total
|
|
No.
|
(%)
|
|
No.
|
(%)
|
|
No.
|
(%)
|
|
No.
|
(%)
|
|
No.
|
(%)
|
|
Improved/much improved
|
84
|
(90)
|
|
23
|
(74)
|
|
5
|
(56)
|
|
8
|
(100)
|
|
120
|
(85)
|
|
Unchanged
|
8
|
–
|
|
8
|
–
|
|
4
|
–
|
|
0
|
–
|
|
20
|
(14)
|
|
Worse/much worse
|
1
|
–
|
|
0
|
–
|
|
0
|
–
|
|
0
|
–
|
|
1
|
(1)
|
|
Total
|
93
|
–
|
|
31
|
–
|
|
9
|
–
|
|
8
|
–
|
|
141
|
(100)
|
Figure 2 shows the registered effect during the first four weeks after treatment in different age groups, with a tendency to best effect in the oldest patients.
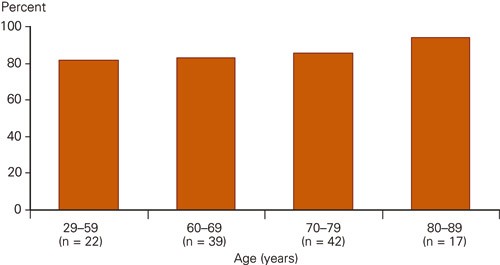
Figure 2 Proportion of patients who were assessed as improved in different age groups four weeks after the first ECT course at Dikemark Hospital 1960 – 95 (n = 120)
How quickly did the improvement occur after the first ECT course?
In 92 of the 120 patients (77 %) with improvement after the first ECT course, the time when the first signs of improvement occurred was noted in the case record. The first signs of improvement were noted on the same day as the first treatment was given (day 0) in 24 %, within six days in 77 % and within 15 days in 97 % (Fig. 3).
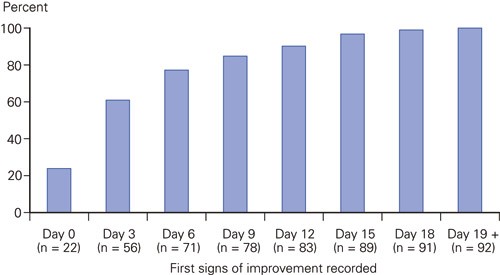
Figure 3 Positive effect noted according to number of days after first ECT given at Dikemark Hospital 1960 – 95, cumulated. The time when the first signs of improvement were noted in the medical records in 92 of the 120 patients with improvement after the first treatment (n = 92)
Signs of improvement were registered in the majority of patients as early as after three treatments, regardless of diagnosis. No statistically significant connection was found between the type of stimulus (sine wave treatment or brief pulse stimulation) or electrode placement and how rapidly the effect appeared (data not shown).
Results of all the ECT courses (n = 241)
It was possible to assess the degree of improvement in 240 of 241 ECT courses. The findings in later courses were about the same as in the first course (Table 2).
Side-effects were observed in connection with the treatment in about half the courses (Table 4). Most of these were very transitory and only present during the waking up phase after general anaesthesia. Forgetfulness was noted in 49 (20 %), confusion in 34 (14 %), dizziness/unsteadiness in 14 (6 %), and headache in 8 (3 %).
|
Table 4 Side-effects described during the first four weeks after electroconvulsive therapy given at Dikemark Hospital 1960 – 95 (n = 241)
|
|
No. courses
|
(%)
|
|
Nothing noted
|
118
|
(49.0)
|
|
Forgetfulness
|
42
|
(17.4)
|
|
Considerable forgetfulness
|
7
|
(2.9)
|
|
Confusion
|
34
|
(14.1)
|
|
Dizziness/unsteadiness
|
14
|
(5.8)
|
|
Headache
|
8
|
(3.3)
|
|
Cardiovascular¹
|
5
|
(2.1)
|
|
Neurological²
|
3
|
(1.2)
|
|
Other³
|
10
|
(4.1)
|
|
Total
|
241
|
(100)
|
|
[i]
|
Discussion
The indication for electroconvulsive therapy at Dikemark Hospital after 1960 reflects the present recommendations, with relatively limited indications. As many as 88 % had an affective main disorder, and there was a high degree of severe psychotic depression, pronounced somatic morbidity, many attempts at suicide, and admissions before their first course of treatment.
About 85 % were reported as being improved during the four weeks after starting treatment, and the majority of these showed signs of improvement as early as during the first week of the treatment. This applied to both the first and later courses. A total of 43 % were described as being much improved after the first ECT course and could be discharged within four weeks. This is a high response rate in patients who are very often regarded as resistant to treatment.
In a prospective study in the USA, 75 % of 253 patients with severe unipolar depression, and who completed the study, had remission after the treatment. Of those with psychotic symptoms, as many as 95 % achieved remission with bitemporal placement of the electrodes (8). Psychosis in patients with major depression seems to predict beneficial results of bitemporal ECT, while antidepressants are probably less effective (10, 12). Psychotic depressed patients should therefore not be regarded as resistant to treatment before they have received a full ECT course. According to a leading article by Beale & Kellner, the treatment can reduce and prevent suffering when given earlier in the course of psychotic depression (13). A longer index episode reduces the possibility of achieving remission (7). Kellner et al. found that electroconvulsive therapy reduced the danger of suicide by 81 % in the course of 10 treatments (14). Early use of this treatment is connected with less time spent in hospital and lower costs (15).
The result of treatment is surprisingly good as most patients had tried two antidepressants for a long period. In the STAR*D study in the USA, only 14 % of those who had not achieved remission after use of two different antidepressants, achieved remission on the third attempt at treatment with medication (11).
Most patients showed signs of improvement already during the first week. A rapid response by patients suffering deep depression has also been found by others (16). ECT should be the first choice when rapid remission is important. This applies to patients who are severely affected, those with serious danger of suicide, depressive psychosis, melancholia, life-threatening depression with insomnia, anorexia and significant loss of weight (11). This also applies to some patients with severe pre- and post-natal depression during pregnancy and after delivery (5, 17).
Electroconvulsive therapy was well tolerated. In almost half the case records, neither doctors nor nurses had noted any form of side-effect or complications. In those with forgetfulness, the memory impairment was described as considerable after seven courses (3 %). We do not know how long the memory impairment lasted. We know from other studies that these side-effects disappear after a few weeks in most cases, in others after some months. It cannot be stated categorically that memory impairment is only temporary in all cases (4). The impairment may also be due to the depression itself. Lerer et al. concluded that two treatments a week is effective with fewer cognitive side-effects than with three treatments a week, while three treatments a week is indicated when a rapid onset of improvement is important (18). We know that side-effects are reduced with brief pulse stimulation and unilateral electrode placement, which is standard now (19). Elderly patients with cognitive impairment often develop transitory episodes of confusion immediately after treatment, which is often dependent on the number of treatments, strength of the pulse and which type of stimulation is given (20). In our experience, headache often lessens after the first meal or can be treated with a mild analgesic.
In most cases the side-effects were temporary. Five patients developed serious and more permanent complications in connection with the treatment (possible compression fracture, fracture of neck of femur, pareses and myocardial infarction/death). The doctors concluded that several of these events were not directly related to ECT treatment.
Having major depression for a long time is a health risk in itself, with increased risk of morbidity and mortality. The risk of developing side-effects from the treatment should be weighed against the risk of suffering from this condition. In a large register-based study, lower mortality from natural causes and a slightly higher suicide rate were found in hospitalised patients who had received ECT compared with those who had not. The patients who had received this therapy were mentally and somatically seriously ill, and lower mortality from natural causes was regarded as evidence that the treatment was not dangerous, but the authors assume that the effect on the mental health reduced the mortality due to somatic causes. A slightly higher risk of suicide in this group was assumed to be due to this being a special sample with a high degree of morbidity, but also shows that those who treat these patients should be particularly careful when considering maintenance therapy, for example with antidepressants (21).
Strengths and weaknesses
The patient population consisted of patients admitted from one area and poorly functioning patients transferred from other departments. The sample may thus represent rather more poorly functioning patients than in the general population.
Primarily, the important limitations of the present study are the retrospective design and the dependence on the quality of the information in the case records. The study cannot answer the question of whether any patients had a long-term effect on their memory. The assessment of the clinical effect was carried out by the same person, the first author, after reading through the case records. The first author has worked in all three departments, and has taken part in administering some of the ECT treatments. This may weaken the validity of the assessments. The reliability of the diagnoses, the effect, and side-effects were checked by independent scrutiny of randomly selected case records by the second author, and indicates that the assessments are objective. The results were not compared with a control group that received another type of treatment in the hospital during the same period. However, the strength of the study is its naturalistic design in a psychiatric hospital that used ECT to a limited degree, which probably reflects typical clinical practice in Norway during this period. All the patients who received this type of treatment throughout 36 years in three departments at Dikemark Hospital were included. The case records were lengthy, and the reports by the nurses and auxiliary nurses, which were written continuously several times a day, were detailed. A future study should explore the differences in response between different methods of treatment by using recommended assessment scales and independent individuals for assessing effect and side-effects.
Conclusion
The results indicate that ECT is a method that gives a rapid response in the treatment of major depression. The treatment was relatively well tolerated, even by the physically feeble elderly. The rapid onset of effect is very important when the patients are severely affected or when the danger of suicide is great.