Local treatment of acne vulgaris is particularly relevant in mild and moderate cases. In cases of comedoacne, local retinoids, for example adapalene, are recommended, because of the keratolytic properties of these drugs. In cases of mild papulopustular acne, local retinoids can be combined with an antibacterial agent, for example benzoyl peroxide.
Acne vulgaris is a very common skin disease particularly in young people. In the age group 12 – 24 years, 25 – 85 per cent are affected , although the condition can occur in all age groups (1). Knowledge of the pathophysiology and clinical characteristics are required in order to select the appropriate treatment. This article presents various forms of local treatment, which will be relevant most often in mild and moderate cases.
Materials and methods
The article is based on a non-systematic literature search in PubMed. A discretionary selection of articles was made on the basis of the authors’ experience from the field.
Pathophysiology
Acne vulgaris is a disease of the sebaceous glands. The condition is associated with sebaceous hypersecretion and is dependent on the sexual hormones testosterone and sex hormone-binding globulin (SHBG) (2). Abnormal cornification of the pilosebaceous canal is caused by increased proliferation or reduced shedding of keratinocytes, which cause the formation of a plug of sebum and keratin. The anaerobic, Gram positive microorganism Propionibacterium acnes proliferates in the anaerobic, lipid-rich environment caused by the increased production of sebum. A high production of sebum results in a higher concentration of P. acnes, although there is no correlation between the number of bacteria on the skin surface and the severity of the acne.
P. acnes produces lipases, which, in combination with other biologically active substances, decompose sebum, thereby releasing fatty acids and hydrolytic enzymes. These affect the sebaceous glands and stimulate an inflammatory response, with a preponderance of the cytokines IL-1-α, IL-β and TNF. Studies indicate that acne is a primary inflammatory disease, since upregulated CD3-positive and CD4-positive T-cells have been found in microcomedones, as well as an increased number of macrophages and upregulated inflammatory vascular markers prior to hyperkeratinization and hyperplasia of the sebaceous glands (3).
The impact of nutrition on the development of acne has been widely debated. Several recent studies indicate that intake of foods rich in quickly degradable carbohydrates causes hyperglycemia, which stimulates the secretion of insulin and the release of an insulin-like growth factor (IGF-1). IGF-1 has a direct effect on the sebaceous glands and stimulates epidermal hyperplasia, which increases the risk of development of acne (4).
Other potentially aggravating factors include sweating, smoking and stress. Some patients experience deterioration in the pre-menstrual period and in times of increased air humidity, while sunlight often improves the condition (5, 6).
Clinical findings in acne
Acne is usually restricted to the face, chest and back. Skin eruptions consisting of comedones, papules and a few pustules are commonly referred to as mild acne. Open comedones are black, punctate lesions in an enlarged follicular canal. Closed comedones are millimetre-sized, non-inflamed white papules. Moderate acne is characterized by a larger number of pustules. The remaining skin tends to be oily, with a shiny surface, particularly in the T-zone of the face, i.e. forehead, nose and chin.
Acne can occur in all age groups, and the youngest patients are treated somewhat differently. Acne neonatorum can be observed in children of both genders aged 0 – 3 months. Causes include hormonal influence, transferred via the placenta, and P. acnes. The condition often manifests itself as comedoacne on the nose, cheeks and forehead. This can be treated with a cream containing ketoconazole 1 – 2 times per day for one month. Infantile acne in the age group 4 – 12 months and pre-adolescent acne in the age group 7 – 12 years are mainly observed in boys. Familial clustering occurs, and could be a warning signal for development of more severe acne in adolescence. Local treatment is usually sufficient. Acne excoriée is most often observed in women who scratch small acne lesions. The patient may suffer from accompanying mental disorders and should be examined for such conditions.
General measures
Thorough information should be provided to young patients to ensure that they follow the treatment regimen . It is important to keep the skin clean in order to restrict the development of skin lesions and oily skin. The face should be cleaned with a cleaning agent with a pH of about 5.5 every morning and evening, and also after physical exertion with pronounced sweating, to remove sebum and impurities (7). This washing has no effect on the production of sebum. The skin should not be scrubbed excessively. Papules and pustules should not be scratched or their content squeezed out, since this could aggravate the inflammation and cause scarring. Cosmetics should be water-based and non-occlusive, this also applies to hair-care products.
Guidelines for choice of treatment
Various medication for local treatment of acne target different points of the pathogenesis (fig. 1). Antibacterial agents such as benzoyl peroxide, azelaic acid and local antibiotics inhibit the growth of P. acnes. The production of sebum can also be reduced by using local retinoids and benzoyl peroxide. These preparations also act comedolytically.
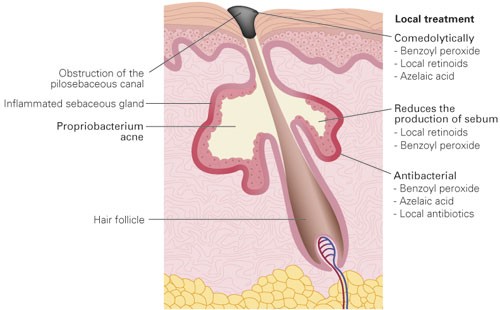
Figure 1 The anatomy of the sebaceous gland and points of attack for various drugs for local treatment
The choice of treatment is decided on the basis of degree of severity and how widespread the condition is. In comedogenic acne, local retinoids are the first choice, alternatively azelaic acid. In facial papulopustular acne, antibacterial agents, preferably benzoyl peroxide, should be added. Combination treatment is preferable with a view to reducing the risk of development of resistance during treatment with antibiotics. The medication should be applied 1 – 2 times per day for at least three months before assessing the effect. The vehicle should be chosen on the basis of the patient’s skin type. For those who have dry skin, a cream should be chosen, and gels should be used by patients with an oily skin type. Those who do not respond to the treatment should usually be referred to a dermatologist (8).
Retinoids
Adapalene 0.1 % and tretinoin 0.05 % are local vitamin-A-acid preparations that normalize the differentiation of the keratinocytes in the pilosebaceous canals. Their effect is comedolytic and to a lesser extent anti-inflammatory. Retinoids are best suited for comedoacne and for maintenance treatment. The effect does not lessen over time. Retinoids are contraindicated during pregnancy, because of the teratogenic properties of the vitamin A acids, even though their systemic absorption is minor. Contact with the mucous membranes should be avoided. The most frequent side effects include blushing, peeling, itching, a burning sensation or increased photosensitivity (8, 9). Adapalene is preferred to tretinoin, since it has fewer side effects, gives faster relief and has less systemic absorption.
Antibacterial agents
Azelaic acid cream, benzoyl peroxide gel and clindamycin solution inhibit P. acnes and have an additional anti-inflammatory effect. Clindamycin solution should be avoided as a monotherapy, because of the risk of development of resistance (8). Benzoyl peroxide reduces both P. acnes by 90 % after just a few days, and free fatty acids by 40 %. Development of resistance or reduced efficacy over time have not been described.
Local treatment with benzoyl peroxide protects against development of resistance to local and oral antibiotics, and should be included in a combination therapy when these preparations are used (8, 9). It is important that the patient is told that benzoyl peroxide can stain clothes (10).
Combination drugs
The combination drug adapalene/benzoyl peroxide has a synergetic effect on acne, and can ensure better follow-up of the treatment (8, 10). The drug is only used once daily, and an effect can be seen as early as during the first week. Side effects in the form of skin dryness, blushes and irritation have been described during the first 14 days.
Treatment of pregnant women
Clindamycin, benzoyl peroxide and azelaic acid can be used as local treatment during all stages of pregnancy. Retinoids are contraindicated.
Conclusion
Acne vulgaris is a disease of the sebaceous glands, where the microorganism P. acnes, sebaceous hypersecretion, abnormal keratinization and inflammation are key elements. Local treatment is used in mild or moderate conditions, especially when the skin eruptions are restricted to the face. Retinoids, such as adapalene, act keratolytically and are the first choice in mild cases with comedones and papules. If pustules occur, antibacterial agents such as benzoyl peroxide or clindamycin should be added.