Patients with pressure ulcers (decubitus) represent a group of patients who often need extensive nursing, management and other medical treatment. Health personnel should identify patients at risk of developing pressure ulcers at an early stage, and start prophylactic measures. If the ulcer has developed already, the wound should be assessed for further treatment. In this article we discuss the classification, prevalence, aetiology, pathophysiology, prophylaxis and operative treatment of pressure ulcers.
Material and method.
The article is based on a non-systematic search in the electronic databases Medline and Embase, where we have selected articles at our own discretion. We have also used our own clinical experience as a basis for assessment and treatment of pressure ulcers.
Classification and prevalence
A pressure ulcer is a localised area that is at risk of developing tissue necrosis or where tissue necrosis has already developed because of unilateral pressure, traction and/or exposure to friction over a certain period (1). Pressure ulcers usually develop over areas where the soft tissue coverage over a projecting bone is thin, for example over the sacrum, ischial tuberosity, trochanter, heels, and lateral malleoli. There are several classifications of pressure ulcers. The classification of the European Pressure Ulcer Advisory Panel (EPUAP) is often used. It is based on the depth and extent of the ulcer in the skin and underlying tissue (Frame 1, Figure 1) (1). This classification gives guidelines on how to treat ulcers.

Figure 1 Paraplegic patient who has developed an approximately 10 cm grade 3 pressure ulcer, over the greater trochanter (a), a 5 cm grade 4 pressure ulcer with undermined skin pockets over the ischial tuberosity (b), and an 8 cm grade 2 pressure ulcer over the sacrum (c). Photo Kim Alexander Tønseth
Frame 1
Classification of pressure ulcers
Grade 0 Transitory redness of skin caused by reactive hyperaemia, which disappears on finger pressure. The circulation is intact and the condition is reversible, but there is often pain.
Grade 1. Persistent redness in intact skin (> 1 hour), which does not fade on finger pressure (non-blanching). There is incipient tissue damage, inflammation and pain. The condition is reversible with relief of pressure.
Grade 2. Wound formation in the dermis, which usually heals with relief of pressure. Gives relatively severe pain.
Grade 3. Pressure ulcers that extend through the dermis down to the subcutaneous tissue, but above the fascia. There is a surrounding inflammation process, but little pain. Requires a long period of relief for healing or before surgical intervention.
Grade 4. The pressure ulcer extends down to muscle and possibly bone tissue. There are often undermining skin pockets and/or fistulas. There is a surrounding inflammation process, but almost no pain. A satisfactory result is seldom reached without surgical intervention
Assessment of a pressure ulcer is often difficult. For example, pathological changes may be hidden under the ulcer scar, where debridement is needed before making a complete assessment. Skin erythema may also be difficult to assess in patients with darkly pigmented skin.
Prevalence studies have shown that pressure ulcers develop in 1.4 to 36.4 % of patients admitted for acute conditions (2). Most of these ulcers are graded as 1 or 2. Primarily, these will heal without surgery. The prevalence is probably high because most attention is usually focussed on the primary diagnosis and pressure-relieving measures are neglected. The prevalence is even higher in different studies regardless of diagnosis group in the chronically ill (3.5 to 50 %) (3) Grades 3 and 4 ulcers also occur more frequently in these patients. 10 to 92 % (1) of hospitalized patients receive prophylaxis for pressure ulcers (1), indicating that the treatment differs considerably and that prophylaxis is often neglected.
Aetiology and pathophysiology
Three mechanical factors, pressure, traction and friction, are the primary causes of pressure ulcers. Other local and systemic factors also play a part in the development and maintenance of pressure ulcers.
Pressure
Pressure is assumed to be the most important single factor in the development of pressure ulcers. External pressure in excess of capillary pressure (12 – 32 mm Hg) leads to increased interstitial pressure and poorer oxidation and micro-circulation. The duration, degree and localisation of the pressure are all important factors affecting the development of tissue damage. The highest pressure is generated in the muscle-bone transition. An external pressure on the skin of 50 mm Hg may increase to over 200 mm Hg over a projecting bone. A pressure ulcer is therefore often deeper than the first visual impression.
Traction
Displacement of bone and subcutaneous tissue in relation to the skin, for example an oblique sitting position in bed (> 30°), gives rise to traction forces resulting in reduced circulation to the tissue. In ulcers that are already established, this traction may result in undermined pockets of skin in the ulcer. The ulcer is then considerably more extensive than seen from the surface.
Friction
When the skin is rubbed over another surface, friction arises, which may lead to intraepidermal blisters and erosions of the skin. This may initiate or accelerate the development of pressure ulcers. In clinical practice friction may arise when for example a patient is pulled across the bed.
Moisture
If the skin is exposed to moist surroundings, for example excessive sweating, urine or faecal incontinence or wound fluid, tissue damage develops more easily when the skin is exposed to pressure, traction or friction (4). Moisture alone gives macerated skin, while urine and faeces have an additional decomposing effect.
Bacterial infection
The concentration of bacteria increases in tissue that is exposed to pressure and has a reduced micro-circulation (5). The affected tissue may thus be exposed to further decomposition, and infection may then arise more easily. Synergism with other factors may also occur. In grade 4 ulcers the underlying bone may be affected, with gradual development of chronic osteomyelitis. Both superficial and deep infections should be treated to ensure optimal conservative treatment and/or surgery.
Neuropathy
Healthy people seldom develop pressure ulcers as pain occurs when pressure is exerted on the skin for a long period (> 2 – 3 hours). This results in the person changing the position of his/her body, leading in turn to satisfactory micro-circulation and disappearance of pain. Patients with reduced sensation or paraplegia will thus be particularly exposed to pressure ulcers, as they do not register this type of pain. Paraplegic patients also tend to develop muscle spasms, with increased pressure on some skin areas, thus increasing the risk of developing pressure ulcers. Satisfactory relief of pressure and mobilisation may also be problematic in these patients. This increases the risk of recurrence after surgical treatment of the ulcer. Spasms are considerably more frequent in cervical and high thoracic spinal damage than in more caudal injuries (5).
Prophylaxis and non-operative treatment
In order to optimize ulcer healing, satisfactory treatment of other supplementary diseases, particularly heart failure, diabetes and spasms, is of vital importance. Physiotherapy should be considered in patients who are confined to bed. The great majority of patients will benefit from physiotherapy for mobilisation and adaptation of exercises in bed, passive mobility training, or related to their lung capacity.
Prophylaxis includes optimising pressure relief and other general measures. Superficial pressure ulcers (grades 1 and 2) should primarily be treated conservatively by intensifying prophylaxis and local wound treatment.
Relief of pressure
Relief of pressure is by far the most important factor both in the prevention and treatment of superficial pressure ulcers. In patients who are confined to bed, pressure points should be distributed over as large an area as possible. Specific pressure points may be protected using extra pillows, so that the pressure on the skin is less than the capillary pressure. Assistant nurses/caregivers play a very important part here, whether the patient is treated at home, in hospital, or in a nursing institution. Many patients need practical help to relieve pressure by for example turning over and extra pillows under pressure points. High priority should be given to this work. There are various special mattresses for different beds, enabling distribution of pressure.
Paralysed patients should generally be turned over every 2 to 3 hours, depending on clinical status and type of mattress in use (6, 7). Sensors are available which register when the patient should change position when lying or sitting, depending on the pressure exerted and how long the skin has been under pressure. Studies have shown that relief of pressure and satisfactory local wound treatment have led to healing in 65 % of type 2 pressure ulcers, and about 14 % of type 3 pressure ulcers, but have no effect on type 4 pressure ulcers after six weeks follow up (8).
Nutrition
Satisfactory nutrition is important in both the prophylaxis and treatment of pressure ulcers. There is an obvious connection between undernourishment and the development of pressure ulcers (9). The protein intake has been shown to be one of the best predictors of the development of pressure ulcers (10). The intake of vitamins and minerals should be adequate. We recommend orientating blood tests to assess the nutritional status, and starting supplementary treatment if necessary.
Prophylaxis of infection
Satisfactory healing depends on the prevention of infection. The ulcer should be assessed regularly depending on the size and how much secretion is being produced, varying from once daily to once weekly. The ulcer is usually cleansed with physiological saline. Antibiotics are only used if infection has been established. Uncritical use of antibiotics increases the development of resistance, and antibiotics may also be cytotoxic and thus delay healing (11). Use should in any case be limited to a maximum of 14 days. A bacteriological test should be taken before starting treatment with antibiotics.
Local ulcer treatment
Removal of necrotic material from the ulcer is necessary for optimal granulation and re-epithelialisation of the edges, which is 1 mm per day under optimal conditions (4). Necrosis results in the body trying to break down the material (catabolic phase), thus delaying healing (anabolic phase). In exceptional cases, small dry necroses (< 3 cm) may be left without revision. Small revisions can be performed in the patient’s bed with anaesthetic gel and a curette. Alternatively, products that decompose small necroses, either by enzymes or a hyperosmolar gel may be used.
Local wound treatment consists of keeping the wound clean and moist. If tendons or bone have been exposed, it may be beneficial to cover the wound with iso-osmolar wound gel. A bandage that occludes the wound may also be useful, for example films, hydrocolloid bandages, foam bandages and alginates. This has been shown to promote re-epithelialisation, reduce pain, increase autolytic breaking down of necroses, and to create a barrier against bacteria (12).
Other local treatment
During recent decades, several different wound products have been developed to promote healing of pressure ulcers. Many of the products lack good documentation, and there are no good studies comparing different alternatives in the treatment of pressure ulcers. In some patients these products may give good results and should be assessed either as treatment alone or for pre-surgery use. In some studies, use of various fibroblast growth factors and platelet derived growth factors have been shown to improve healing compared with wounds not treated in this way (13, 14). Extracellular matrix contains structural and functional proteins that play an important part in the maintenance of normal cell and tissue structure during wound healing (15), but there is no good documentation of the effect.
High energy acoustic pressure waves (120 – 480 pulses/min) and electric impulses (16) liberate proteins that promote healing and may have a beneficial effect on migration and proliferation of fibroblasts in several types of chronic wound (13). Hyperbaric oxygen treatment improves wound healing by increasing the oxygen content of the wound. Indirectly, collagen production and fibroblast proliferation are then increased, and leukocyte function is improved (17).
Negative pressure therapy is a dynamic, non-invasive procedure that has been much used during recent years. The wound is covered with a sponge or similar material and a semi-occlusive film and suction are applied thus exerting a negative pressure of 50 – 150 mm Hg. The procedure creates a closed and moist wound atmosphere, preventing bacteria from entering the wound and allowing the healthy cells to dry out (18). The pressure reduces the wound volume, superfluous secretion (bacteria and wound fluid) are removed, and granulation growth is stimulated (19). The treatment can be used to prepare for surgery and for stabilisation and promotion of healing of skin transplants.
Cultured keratinocytes are used to some extent in the treatment of chronic wounds, but give a relatively vulnerable epithelialized surface, which is not appropriate with pressure ulcers (13).
Operative treatment
Operative treatment of pressure ulcers is based on three principles:
Excision of the pressure ulcer, bursa and possible calcification
Partial or complete osteotomy to reduce the bony pressure point
Reconstruction of the defect with tissue that gives satisfactory coverage
Before deciding on surgical intervention, it is extremely important to have a plan for the postoperative period and that this is thoroughly discussed with the patient in advance. Successful operative treatment depends on a motivated patient with a positive attitude to postoperative prophylaxis, even if it may involve limitations for the patient, for example a long stay in bed. The consequence of misunderstanding and poor cooperation by the patient may even result in a still larger and more extensive pressure ulcer after surgery.
Wound revision and excision of pressure ulcers
Even if the ulcer has been given satisfactory local wound treatment and is considered to be «clean», excision of the ulcer and the fibrous pocket (bursa) is almost always necessary before closing the wound. Chronic pressure ulcers will almost always contain epidermal cells or possibly micro-abscesses, which facilitates wound infection or unsatisfactory healing unless the ulcer is completely removed. In some cases there may also be subcutaneous channels (sinuses) that must be excised. In order to facilitate the assessment of the wound’s limits, the cavity can be filled with methylene blue. It will then be relatively easy to see whether satisfactory amounts of tissue have been removed. The edges of the wound are also often fibrotic, making good healing more difficult.
Osteotomy
If the pressure ulcer and bursa involve bone (grade 4 ulcer), this area should be included in the excision. The fibrotic pocket is dissected down to the bony region, and the fragment is removed using a bone chisel. Osteotomy is important in grade 4 ulcers as the bone is often contaminated and/or osteomyelitis is present. The bone fragment should be sent for culture to clarify the bacteriology with a view to making treatment with antibiotics as specific as possible. Although the ulcer does not always extend down to bone, removal of bone tissue to reduce pressure from the pressure point may be relevant, but care should be taken not to remove too much tissue resulting in bleeding, instability or increased pressure on other adjacent structures.
Wound closure
Direct closure of the wound may occasionally be relevant, but there is usually a tissue defect making it necessary to add tissue to the area. Direct closure may then leave a subcutaneous cavity where blood collects leading to healing problems. In superficial pressure ulcers, i.e. grades 2 and 3, skin transplants may sometimes be appropriate, but in most cases this gives too thin coverage with a high risk of recurrence. In the great majority of cases the tissue defect should be covered by local cutaneous or musculocutaneous flaps.
Different types of flaps are used depending on the localisation of the pressure ulcer. Ischial pressure ulcers can be covered with medial or lateral skin flaps from the posterior side of the thigh (fig. 2a). If there are large volume defects, musculocutaneous flaps from the gluteal area or posterior thigh, such as rotation flaps, advancement flaps or V-Y flaps (Figs 2b, 2c) may be appropriate. The secondary defect can often be closed directly, or with a skin transplant. In some cases a pedicled flap with a skin eye based on the tensor fascia lata (fig 2d) or local or free perforator flaps (fig 2c) can be used. Many of the same techniques are used in pressure ulcers over the sacrum and trochanter, while flaps from the posterior side of the thigh are seldom used.
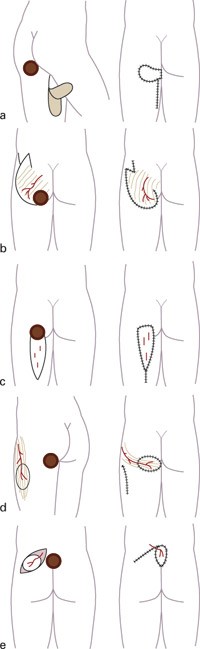
Figure 2 Various surgical procedures used to cover tissue defects after excision (and possible osteotomy) of pressure ulcers. a) Medial adipocutaneous transposition flap from the thigh, b) Gluteal rotation flap based on the gluteus maximus muscle with Z plasty prolongation, c) fasciocutaneous displacement flap with V-Y plasty, d) tunnelled pedicled fasciocutaneous flap based on the tensor fasciae latae muscle, e) local adipocutaneous flap based on the superior gluteal artery
Socio-economic perspectives
The course of the disease in patients with pressure ulcers is undoubtedly resource-demanding, and is often prolonged, thus leading to high socio-economic costs for the community. There are few studies that provide reliable figures on the actual costs incurred in connection with pressure ulcers. There is much room for improvement in the prophylaxis. Start of treatment at an early stage could shorten a long-lasting and resource-demanding condition and thereby promote major savings in the national economy. At a time when the hospitals have limited financial resources and have to make strict priorities, this group of patients deserves more attention and should be given higher priority. According to the Health Directorate’s priority guidelines (20), patients with pressure ulcers have the right to health assistance for a maximum of 26 weeks.