Almost 60 % of cancer patients are cured by cancer treatment (1). This group does not require special guidelines for CPR (2) in the event of cardiac arrest (3). For patients in a palliative phase of the disease, however, the question whether the patient is a candidate for CPR becomes increasingly relevant with shorter life expectancy. Approximately a quarter of those who die in Norway are in this group (1), and all of them will eventually suffer cardiac arrest. So when should CPR not be administered?
Both Norwegian and international guidelines have been drawn up for CPR in cases of serious illness (5 – 7). The Norwegian guidelines National guidelines for decision-making processes for restricting life-prolonging treatment in the seriously ill and the dying, hereafter called the National Guidelines (5), can be summarised as requiring that at least one of three criteria must be met to justify refraining from possible life-prolonging treatment in a palliative care patient:
The patient, or family if the patient is not able to give informed consent, must have stated that he/she does not want it
The personnel in charge consider, if possible in consultation with the patient/family, that the treatment, if successful, will prolong or worsen the suffering
The personnel in charge consider such treatment to be futile
This study focuses on criterion 3, i.e. when CPR will not be able to help a cancer patient in the palliative phase to survive cardiac arrest. The objective was to answer the following questions: What is the effect of in-hospital CPR in palliative care cancer patients? In addition we wished to consider which pre-registrable patient factors might influence the result of CPR in this patient group.
Knowledge base
We conducted literature searches in PubMed for the period 1989 – 2010 as shown in Fig. 1. Some searches also turned up studies under «related citations» and «reviews» in addition to the term search, and one article that satisfied the criteria was included in this way. The inclusion criteria were:
Studies presenting the results of administering CPR to hospital inpatients, with cancer patients with metastatic disease or in palliative care forming the whole or part of the patient population
Studies on factors that are registrable prior to cardiac arrest and which influence the outcome of CPR, when cancer is mentioned in particular
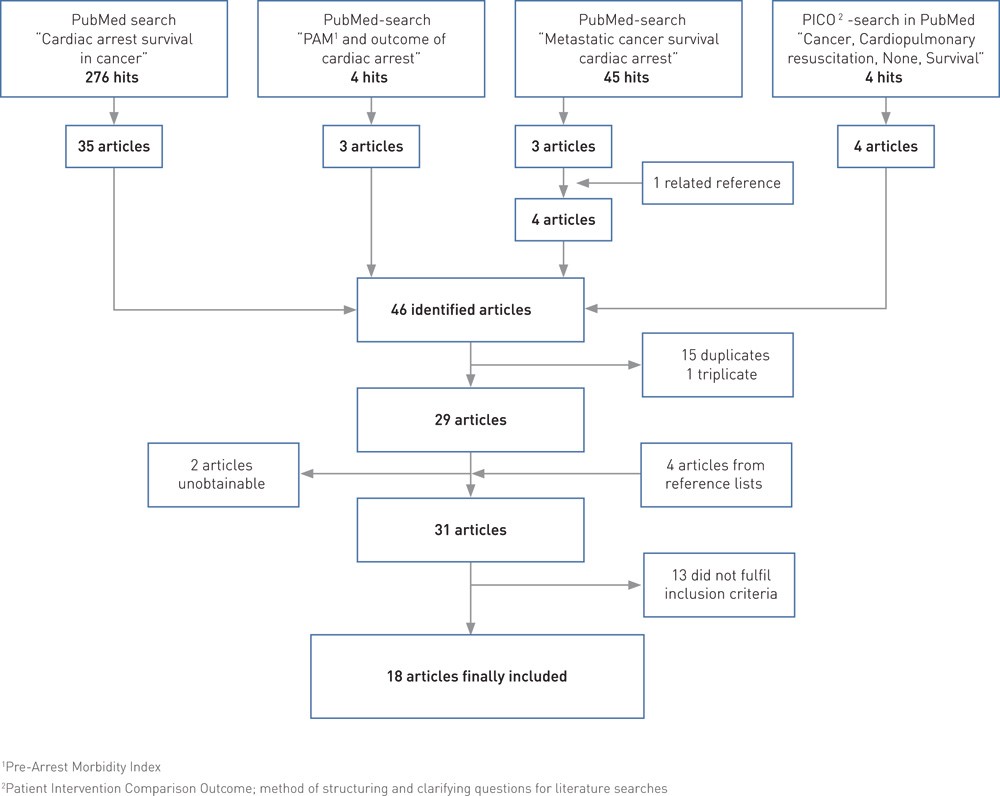
Figure 1 Flow chart for literature searches and selection of articles
Exclusion criteria were studies on persons aged under 18, with fewer than 20 patients included, published in a language other than English, or that could not be retrieved in full text (electronically or manually when ordered through the university library).
In the studies, the post-CPR outcome was usually measured in terms of return of spontaneous circulation (ROSC) and/or as a percentage of those subsequently discharged alive. This study places emphasis on discharge alive as an outcome measure.
The Pre-Arrest Morbidity Index (PAM Index) is based on different weighting of 15 patient factors (Table 1) and was introduced by George et al. in 1989 to predict the result of CPR in unselected patient groups (8). Cancer is included as a separate factor, and the index is based on several factors that often occur with advancing malignancy.
|
Table 1 Pre-Arrest Morbidity Index (PAM index) for use in predicting the results of cardiopulmonary resuscitation in unselected patient groups (8). The score is the sum of the numerical values of the factors shown.
|
|
PAM index factors
|
Numerical value
|
|
Hypotension, systolic pressure < 90 mm Hg
|
3
|
|
Renal failure; S-creatinine > 220 micromol/L
|
3
|
|
Malignancy
|
3
|
|
Pneumonia
|
3
|
|
Homebound lifestyle
|
3
|
|
Angina pectoris
|
1
|
|
Heart failure, NYHA class III and IV
|
1
|
|
Acute MI
|
1
|
|
S3 gallop rhythm
|
1
|
|
Oliguria, urine production < 300 ml/24 h
|
1
|
|
Sepsis
|
1
|
|
Mechanical ventilation
|
1
|
|
Recent cerebrovascular event
|
1
|
|
Coma
|
1
|
|
Cirrhosis of the liver
|
1
|
Physical performance status as defined by WHO/ECOG/Zubrod (Box 1) is commonly used for cancer patients (9) and is regarded as a possible predictor in several studies. Karnofsky performance status is also used; this scale ranges from 100 (no evidence of disease) to 0 (dead) (10).
BOX 1
Grading of physical performance status in cancer patients (simplified by the authors). Prepared by the Eastern Cooperative Oncology Group (ECOG) (9), used by the World Health Organisation (WHO)
-
WHO
0 Fully active
-
WHO
1 Restricted in physically strenuous activity
-
WHO
2 Must rest a good deal, but less than 50 % of waking hours
-
WHO
3 Must rest more than 50 % of waking hours
-
WHO
4 Completely disabled. Confined to chair or bed
The result of the searches and selection of articles for inclusion are shown in Fig. 1. The 18 included studies consisted of four meta-analyses, one of which also had a separate, retrospective patient study (11 – 14), eight clinical studies (8, 15 – 21), and six literature studies or review articles (22 – 27). Ten of the articles considered CPR administered to all patient categories («unselected») (8, 11 – 13, 15, 17, 22 – 25), and eight considered CPR administered to cancer patients only (14, 16, 18 – 21, 26 – 27).
Results
The cancer disease
Table 2 shows post-CPR survival rates in those studies that provide exact figures. Both individual studies and meta-analyses show that cancer patients have poorer survival to discharge than unselected patient groups, and that survival is even less with metastatic disease. Early studies showed no survivors with metastatic cancer (12, 22), but in a meta-analysis from 2006 with cancer patients only, Reisfield et al. found higher survival with metastases than older studies gave reason to expect (14).
|
Table 2 Post-CPR survival rate in different studies, review articles and meta-analyses
|
|
Patient group
|
First author, year published (reference)
|
Type of study/article
|
Number of patients
|
Return of spontaneous circulation ( %)
|
Discharged alive ( %)
|
|
Unselected patients
|
George, 1989 (8)
|
Clinical study
|
140
|
|
24.3
|
|
Ballew, 1994 (15)
|
Clinical study
|
313
|
|
16.0
|
|
Hamill, 1995 (23)
|
Review article
|
|
|
15
|
|
Ebell, 1998 (13)
|
Meta-analysis
|
9 398
|
43.1
|
14.6
|
|
Varon, 2007 (27)
|
Review article
|
|
31
|
15
|
|
Larkin, 2010 (17)
|
Cohort study
|
49 130
|
|
17.4
|
|
Cancer patients, undifferentiated
|
Vitelli, 1991 (20)
|
Clinical study
|
114
|
65.8
|
10.5
|
|
Ebell, 1992 (12)
|
Meta-analysis
|
276
|
|
5.8
|
|
Ebell, 1998 (13)
|
Meta-analysis
|
3 733
|
|
6.7
|
|
Varon, 1998 (19)
|
Clinical study
|
83
|
66.3
|
9.6
|
|
Ewer, 2001 (16)
|
Clinical study
|
243
|
|
6.6
|
|
Wallace, 2002 (21)
|
Clinical study
|
406
|
37
|
2
|
|
Reisfield 2006 (14)
|
Meta-analysis
|
1 707
|
|
6.2
|
|
Cancer patients, localised disease
|
Reisfield 2006 (14)
|
Meta-analysis
|
295
|
|
9.5
|
|
Cancer patients, metastatic disease
|
Ebell, 1992 (12)
|
Meta-analysis
|
141
|
|
0
|
|
Dautzenberg, 1993 (22)
|
Review article
|
|
|
0
|
|
Ebell, 1998 (13)
|
Meta-analysis
|
2 367
|
|
3.0
|
|
Reisfield 2006 (14)
|
Meta-analysis
|
411
|
|
5.6
|
|
Cancer patients, haematological disease
|
Ewer, 2001 (16)
|
Clinical study
|
130
|
|
1.5
|
|
Reisfield 2006 (14)
|
Meta-analysis
|
400
|
|
2.0
|
|
Cancer patients, haematological or metastatic disease
|
Larkin, 2010 (17)
|
Cohort study
|
5 494
|
|
7.8
|
|
Cancer patients, solid tumours
|
Ewer, 2001 (16)
|
Clinical study
|
114
|
|
12.3
|
|
Wallace, 2002 (21)
|
Clinical study
|
131
|
|
2
|
|
Reisfield 2006 (14)
|
Meta-analysis
|
718
|
|
7.1
|
In a study by Wallace et al., 2 % of cancer patients who received CPR in the Intensive Care Unit were discharged alive (21), while Staudinger et al. found «very high mortality» (18). A number of studies show very poor survival for patients with haematological malignancies compared with solid tumours (14, 16, 21).
Larkin et al. found that anticipated cardiac arrest increases the chance of survival for unselected patients (17), while Ewer et al. did not find any survival at all among 171 cancer patients with anticipated cardiac arrest (16).
PAM index
The PAM index, shown in Table 1, was considered in several studies of unselected patients (8, 11, 12, 22). In the total material in the present study there were no survivors with a PAM index of > 8. In a meta-analysis of CPR to around 7 500 patients, Cohn et al. found only one survivor with a PAM index of > 7 (11). In a review article including studies with a total of 11 825 patients with different diagnoses who received CPR, Dautzenberg et al. recommend reducing the weighting in the PAM index for cancer, uraemia, pneumonia and homebound lifestyle from 3 to 2, increasing the weighting for cerebrovascular episode from 1 to 2 and introducing a weighting of 1 for age > 70 and of 2 for severe dementia. At the same time they write that patients with advanced malignancy are among those with the least chance of survival (22).
Ebell also recommends adjusting the weighting in the PAM index to 10 for metastatic cancer while retaining a weighting of 3 for cancer without metastases (12). Two new factors were also proposed: dependent functional status, with a weighting of 5, and age > 70, with a weighting of 2 (12).
Performance status
In some unselected studies, performance status was found to be crucial as a single factor. Ebell validated dependent functional status to 5 in a modified PAM index (12). In a study of 313 patients, Ballew et al. found that only reduced performance status and sepsis were associated with non-survival (15).
A number of studies indicate that performance status has an even more pronounced effect in cancer patients. In performance class WHO/ECOG/Zubrod > 2 or Karnofsky performance status < 50, Vitelli et al. found only 2.3 % survival after CPR (20). A number of articles cite this finding. The author is of the view that the cancer diagnosis in itself is not a significant variable, but may give that impression because of the influence of more important factors, such as performance status. Reisfield et al. claim in their meta-analysis that performance status, critical illness and reduced general condition are more negative predictors of survival than whether or not a cancer patient has metastases (14). In a study on cancer patients, Varon et al. found survivors after six weeks in WHO performance classes 1 – 2 only (19).
Can the outcome be predicted?
A number of studies attempt to assess the predictive value of their findings. Pre-arrest factors in a fixed index have been found useful in many of the unselected studies, but with various reservations against allowing such an index to have final deciding power (8, 11, 12, 22).
Cohn et al. stress in their meta-analysis that the PAM index is a better predictor of death than of survival, and that CPR can be withheld if the PAM index is > 8 (11). Ebell is of the view that a modified index could identify those patients for whom CPR would be futile (12). Dautzenberg et al. write that survival after CPR appears to be predictable, and that a PAM index with the modifications referred to previously would appear to be effective for this purpose (22). Other studies with all patient groups conclude that existing pre-arrest scores alone are not reliable enough for CPR decisions (17, 25).
Vitelli et al. hold the view that a simple performance status in these patients would quickly determine their chances of surviving cardiac arrest (20). Reisfield et al. stress the poor prognosis for post-CPR survival for the sickest cancer patients, with emphasis on performance status (14). Ewer et al. believe that CPR should not automatically be administered to cancer patients with anticipated cardiac arrest or advanced disease (16). In both their studies, Varon et al. view the survival of cancer patients as extremely poor and CPR as possibly futile, and they advise against CPR in cases of advanced, uncontrollable cancer or multi-organ failure (19, 27).
Sculier concludes in a review article that the survival of patients with less serious cancer disease will be as high as in individuals without cancer (26). If tumour-directed therapy has been abandoned, on the other hand, the survival rate is so poor that CPR is advised against.
Discussion
A number of the included studies are older than one might wish, but these were the ones that emerged from our systematic searches. It is uncertain whether other search terms would have added more. Two articles from 2007 stress that the post-CPR survival rate after inhospital cardiac arrest has been largely unchanged for the past 30 years (25, 27).
Large, well-designed prospective studies are needed to enable unfailing prediction of who would not survive CPR. Prognostic instruments based on retrospective materials will not always provide reliable prediction in a future patient group (17). Decisions must nonetheless be made on the basis of available information, and the present material clearly points in one direction.
The figures for survival of cardiac arrest are described by several authors as «a moving target», rising with the number of patients deselected in «DNR» (do not resuscitate) orders (15, 22). Some believe that deselecting the oldest patients by these decisions masks the age factor (15, 25). In some studies far more cancer patients are deselected than are included in the study (20, 21). This is skewed selection which a number of authors believe results in overly high survival figures (15, 22). Reisfield et al. are of the view that the higher than previously found survival rate with metastatic cancer in their meta-analysis may be partly due to an increase in this type of selection (14).
We believe that the included studies and articles provide substantial information about the chances of palliative care cancer patients surviving CPR. The disease factors examined imply different stages of the cancer disease, and we have therefore found it correct to view the findings as expressions of the change in post-CPR survival as the disease progresses:
Metastasis may range from a single lymph node to large tumour masses in many vital organs, but often characterises the palliative care phase.
The PAM index contains many of the complications that may arise in a late stage of cancer, and can say something about the extent of the disease.
Discontinuation of tumour-directed therapy will normally indicate advanced disease.
A poor physical performance status tells a great deal about the patient’s remaining strength to tolerate new stresses.
Anticipated cardiac arrest is normally part of the terminal stage.
The more advanced the cancer that these factors express, the poorer the survival is found to be, until it is zero. The factors are not mutually independent, but the combination of extensive metastasis, terminated tumour-directed therapy and a poor performance status must be expected to result in very poor chances of survival. If we then take into account the extensive skewing of selection in many of the studies, we believe the findings provide a basis for concluding when CPR will no longer be of benefit to our patient group.
Futile treatment
This concept may be self-fulfilling, and the definition of what is futile must therefore be constantly adjusted as new and applicable medical knowledge becomes available. Nor can anyone demand to be given futile treatment (5). The doctors’ power of definition is then final, and controversial.
A number of authors have attempted to define futility quantitatively. The National Guidelines specify a <1 % chance of success (5). Schneiderman et al. define an intervention as futile when it has failed the last 100 times (28). Statistically, the 95 % confidence interval for such a finding is 0 – 3 % successful interventions (28). Many believe that these quantitative requirements are too strict. They maintain that it must be possible to apply the concept in cases of coma, dementia, advanced cancer, and terminal disease (22, 24, 29). Thus the concept of «futile treatment» is also connected to an evaluation of quality of life and life expectancy and is of a more discretionary nature.
The National Guidelines refer to this in their discussion of futile treatment, but then say the following about CPR: «With cardiac arrest there are no definite criteria for maintaining that cardiopulmonary resuscitation will be futile, apart from in cases of extensive multi-organ failure without reversible causes» (5). The statement is short and categorical, and in light of the present results on palliative care cancer patients could easily be understood too restrictively.
Conclusion
Cancer results in reduced survival after cardiopulmonary resuscitation. As the extent of the malignant disease increases, the survival rate falls towards zero. Given terminated tumour-directed treatment, extensive metastasis and a performance status poorer than WHO 2, the findings provide a basis for maintaining that cardiopulmonary resuscitation will be unsuccessful. A PAM index of > 8 in a palliative care cancer patient points in the same direction. The National Guidelines can be interpreted as more restrictive in their use of the concept ‘futile’ for cardiopulmonary resuscitation than is indicated by the findings of this literature study.
