Atlantoaxial rotatory subluxation is a rare condition which was described for the first time by Sir Charles Bell in 1830 (1). It appears for the most part only in children (2 – 4) (Fig. 1). When subluxation of the atlantoaxial joint persists and gives rise to torticollis, it is called atlantoaxial rotatory fixation (5, 6). The terms atlantoaxial rotatory subluxation and atlantoaxial rotatory fixation are both used to describe the condition in the literature (7). Chronic atlantoaxial rotatory fixation is defined typically as rotatory fixation with a duration in excess of 2 to 3 months (7). The frequency of the condition is rarely mentioned in the literature. In a material sample of 288 children with torticollis, only two had verified atlantoaxial rotatory fixation (8). The patients present with torticollis where the head is tilted over to one side and rotated to the other side and with slight flexion of the neck. This head position is quite typical and is known as the «cock robin» position (3, 6, 9 – 11), as it resembles the way in which the robin holds its head when listening for a worm (Fig. 2).
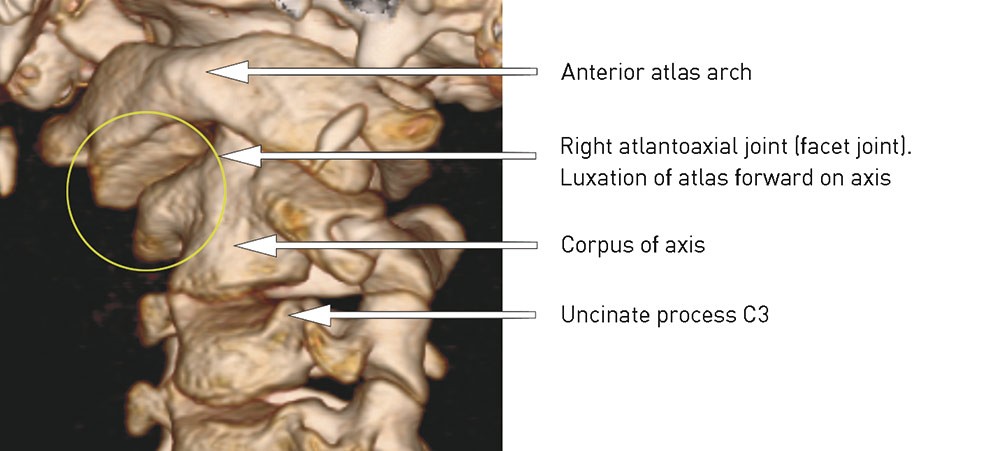
Figure 1 Subluxation of right atlantoaxial joint, viewed from left side/front
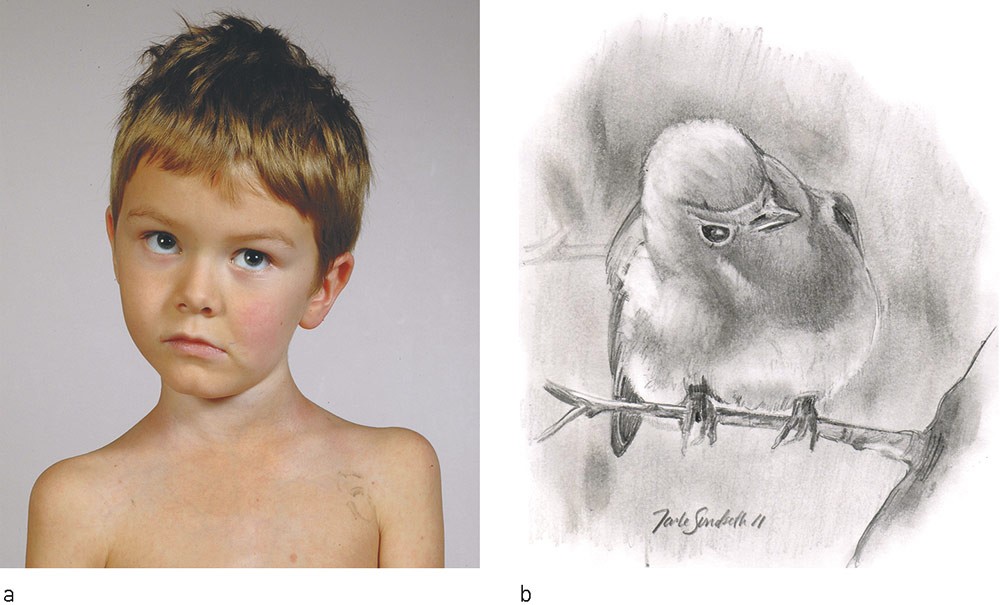
Figure 2 a) «Cock robin» position, thus named because it resembles the head position of a robin listening for a worm (b). The head is tilted to one side with rotation to the opposite side and flexion (C1 luxates forwards on C2). The patient and his parents have given consent for publication of the photograph
The contributory cause of torticollis may be minor neck trauma, an upper respiratory tract infection (Grisel’s syndrome) or surgical procedures in the throat and neck region (3, 9, 12 – 16). In one in four there is no known cause (9). The patient often has moderate pain when the head is kept motionless, while movement towards a normal position triggers pain (13). The neck and head pain usually abates gradually, but the torsion increases (9).
Defined radiological criteria to enable the diagnosis of atlantoaxial rotatory fixation were established in 1979 and are based on a cessation or considerable reduction of movement between the atlas and axis on rotation of the neck during dynamic CT scanning (17). However, the literature provides no clear-cut answer as to the degree to which the movement between atlas and axis is reduced (18). Normally, the atlantoaxial complex is responsible for 60 % of the rotation in the neck and the atlanto-occipital joint for 3 – 8 %, while the remaining rotation takes place below the axis (11). The atlantoaxial joint is stabilised by the transverse ligament, which prevents over-flexion, and the alar ligaments, which prevent over-rotation (3). The pathophysiology of atlantoaxial rotatory subluxation/fixation is not fully understood. A combination of high elasticity of the ligaments and more horizontally oriented facet joints in children may be predisposing factors. In addition, children have a more convex upper joint surface of the axis which articulates with the lower concave joint surface of the atlas, and the uncinate process is poorly developed. Together these may permit greater movement, especially for rotation and lateral bending (3, 9). In children, the head is also larger in relation to the neck than in adults, and the musculature is not as well developed. A combination of these factors may be the reason why the condition appears almost exclusively in children (19).
Atlantoaxial rotatory fixation can be divided into acute and chronic types (7). In acute cases, the displacement often reduces spontaneously in connection with examination or after simple conservative treatment which involves administering analgesics and anti-inflammatory medication (7, 10). In the remainder of cases, careful manual traction followed by a cervical collar result as a rule in reduction, although some patients relapse and have to be treated again (9). However, if the diagnosis is made too late, subluxation between the atlas and axis may be irreversible.
Atlantoaxial rotatory fixation has been written about previously in Tidsskriftet (the journal of the Norwegian Medical Association) (20). Too many children are still going too long with undiagnosed torticollis, which is why we wish to bring this condition and its treatment once more to the attention of the medical community. In this article we present our experiences with surgical treatment of late-diagnosed atlantoaxial rotatory fixation in children. Clinical presentation, radiological findings and surgical treatment will be discussed against the background of the literature.
Material and method
We have reviewed the case notes of patients undergoing surgery for atlantoaxial rotatory fixation at the Department for Neurosurgery, Oslo University Hospital, Rikshospitalet, during the period 2004 – 10. The patients were found after a search on diagnostic codes and by reviewing all the relevant surgical descriptions. We also reviewed the case notes of all patients who had been admitted with the diagnosis code torticollis during the same period and found no more than the six who had undergone surgery and who are referred to in this article.
The surgical techniques used were different methods of posterior atlantoaxial fixation, including Gallie fusion (titanium wire and iliac crest bone graft) (Fig. 3) and the Harms technique (fixation with polyaxial screws and rods) (Fig. 4). The surgical technique was selected on the basis of the individual patient’s anatomy. It was chiefly the bone conditions and the risk of damaging the A. vertebralis which determined the technique employed. Using titanium or stainless steel wire and an iliac crest bone graft is nowadays considered old-fashioned, but these are nevertheless good techniques (21) and are used in our department where screw fixation is considered risky or unsuitable. There may furthermore be significant lateral differences in individual patients which permit screw fixation to be done only unilaterally, but nevertheless with sufficiently stable fixation to make it preferable to the earlier more commonly used methods such as Gallie fusion.
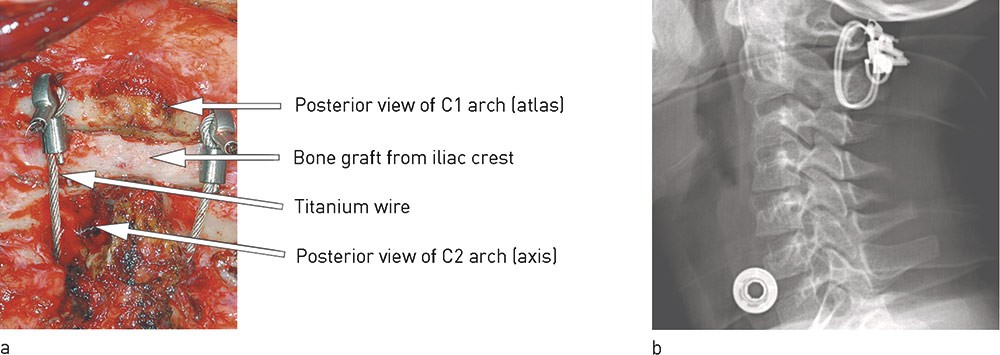
Figure 3 The C1 and C2 arches are fixed to one another with stainless steel or titanium wire bilaterally with a bone graft from the patient’s iliac crest in between (Gallie fusion). a) Peroperatively and b) X-ray taken from the side
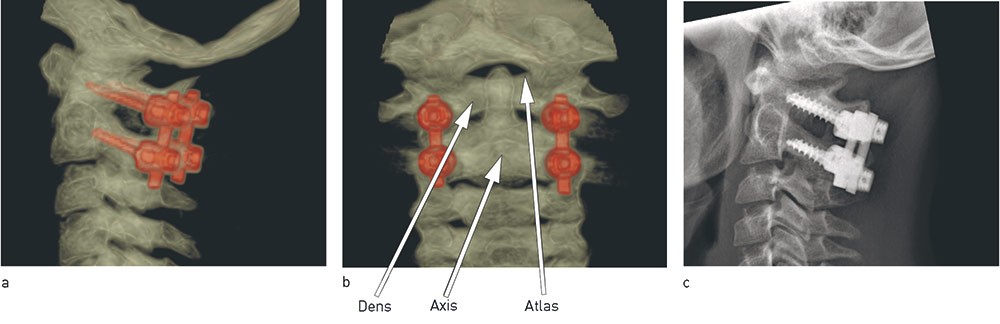
Figure 4 Atlas and axis are fixed with screws and rods bilaterally (Harms technique). CT images from a) the side and b) posteriorly (with screws and rods in atlas and axis marked in red). c) Normal X-ray taken from the side
Five of the patients were fitted with a hard cervical collar and one with a halo vest (Fig. 5), which the patient wore for 8 to 12 weeks postoperatively. The patients were followed up clinically and with control CT scans for at least one year. The case note data reported are from this first postoperative year.

Figure 5 Postoperative external fixation in halo vest. The patient and her parents have given their consent for publication of the photograph
Ethical considerations
The data protection officer at Oslo University Hospital, Rikshospitalet, has approved the use of personal data for the purposes of this article. The parents have provided informed consent for the use of the medical histories and photographs. Patients over the age of 12 have in addition given their own written consent.
Results
Six children, three girls and three boys between seven and 14 years of age, were surgically treated. Five of them had previously suffered minor neck trauma, while one had had an upper respiratory tract infection (tonsillitis). CT scans showed displacement of the atlantoaxial joint in all six. The degree of displacement, evaluated from the CT images, varied (Table 1). One patient had preoperatively total luxation of the atlantoaxial joint unilaterally (Fig. 6).
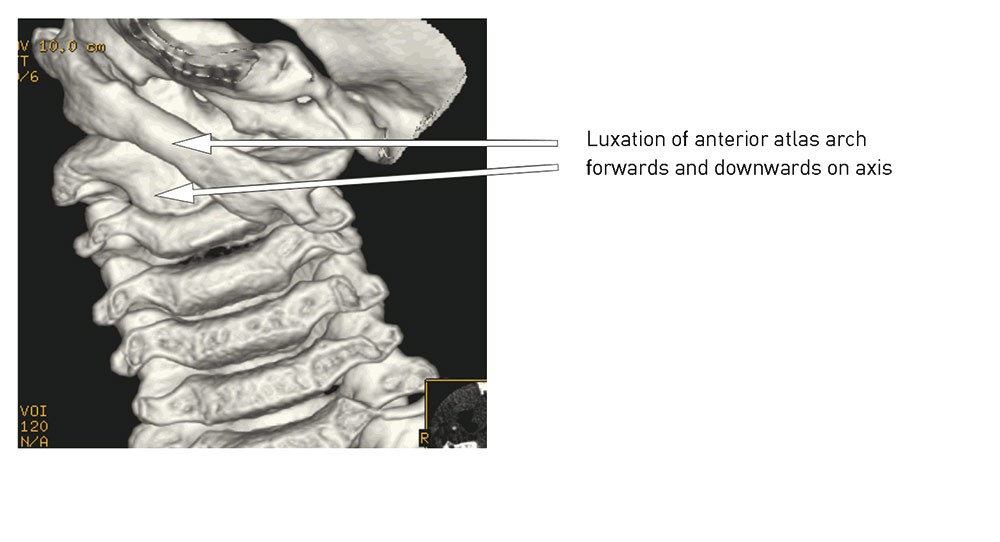
Figure 6 Total luxation left C1/C2 joint (anterior view)
The diagnosis was made between 5 and 36 months after symptom onset. In three of the children, juvenile rheumatoid arthritis was suspected before the CT scan with three-dimensional reconstruction showed subluxation of the atlantoaxial joint. Two of these three were later diagnosed with juvenile rheumatoid arthritis.
In three of the patients, closed reduction was initially attempted using skull traction (Gardner-Wells) for up to 15 days, but without achieving successful correction of the displacement. The diagnosis in these patients was made after five, five and six months respectively. The other patients, where diagnosis was delayed by five, eight and 36 months respectively, therefore went straight to surgery without any attempt at closed reduction. Five of the patients had surgical fixation. The sixth had a fixation that it was not possible to correct, and the operation was concluded without surgical fixation. No serious postoperative complications in the form of bleeding, infection or neurological outcomes were registered.
CT scans performed one year postoperatively showed full reduction in two patients and partial reduction in three of the patients who had had surgical fixation (Table 1), in addition to bone fusion in the facet joint and/or posterior structures (laminae and spinosi) in all six. The sixth patient had bone fusion already at the time of surgery.
At the one-year check-up little pain was reported, apart from in the case of the child who was diagnosed 36 months after symptom onset. All six patients had a certain reduction in rotational movement of the neck when clinically examined. Where we had achieved complete reduction, the reduction in rotational movement was approximately 25 – 30 % in both planes. One child had had repeated botox injections in the sternocleidomastoid muscle because of marked contracture of the muscle, without any significant effect.
Discussion
During the period 2004 – 10, six children between seven and 14 years of age underwent surgery for atlantoaxial rotatory fixation at Oslo University Hospital, Rikshospitalet. Full reduction was achieved in two of the children and partial reduction in three. The sixth child had bone fusion at the time of the operation, and it was not possible to correct the damage surgically.
Five of our six patients had suffered minor neck trauma, while the sixth had had tonsillitis. In a large material sample the condition was normally found to be related to upper respiratory tract infection (35 %), minor trauma (20 %) or surgical procedure of the throat or neck (20 %), while in the remainder of cases the cause was unknown (9). While the male sex is overrepresented in spinal injuries (22, 23), in the case of atlantoaxial rotatory fixation there is a preponderance of females, some 70 – 80 % (9, 23). In our material sample, half the patients were girls.
Prior to the introduction of CT scanning, diagnosis of atlantoaxial rotatory fixation was based on conventional X-ray examination (24). However, the results are frequently difficult to interpret in a child with displacement of the atlantoaxial joint (6, 24 – 26), although X-ray examination is still regarded as a useful supplement to the assessment in order to exclude other pathology, such as congenital malformations or spinal tumour (27). A static CT scan is able to show a displacement between the atlas and axis, although it has its limitations in that it is unable to demonstrate the dynamic relationship between the atlas and axis on rotation (27, 28). A dynamic CT scan of a child who rotates its head maximally to one side will as a normal finding show the atlas rotating approximately 23° on the axis before it starts rotating with the atlas (29). To verify a fixed rotational displacement, a dynamic CT scan, where the images are taken with the head rotated maximally to the right, the left and straight forward, is the best method. Only then is it possible to see whether the displacement in the joint can be corrected by rotation of the neck. If there is little or no change in the displacement subluxation at rotation, the radiological conclusion is atlantoaxial rotatory fixation (27, 28, 30). This method of examination is recommended for mapping the anatomical conditions in the upper cervical spine in children (31).
Torticollis in children can have different causes, and a persistent twisted neck position should always be more closely investigated. The most common cause in children is congenital muscular torticollis (8). This condition is caused by the contraction and gradual contracture of the sternocleidomastoid muscle on the opposite side of the one to which the head is rotated. Such muscle spasm is not normally found in atlantoaxial rotatory fixation (20). However, our patient with total luxation of the atlantoaxial joint did have contracture of the muscle. Three of our patients had suspected juvenile rheumatoid arthritis prior to surgery, and two have since been given that diagnosis. It is uncertain whether there is a connection between these conditions, but one theory is that rotatory fixation can occur as a result of greater laxity of the ligaments and synovial thickening in juvenile rheumatoid arthritis (32).Concurrence is also described in a case study from 2011 (33). We believe, therefore, that it is important to undertake a broadly based assessment of children with atlantoaxial rotatory fixation in order to exclude juvenile rheumatoid arthritis. If the cause of torticollis in children cannot be found, the possibility of tumour must be excluded. Tumour of the skull base (posterior fossa tumour) can compress/affect nerve structures which innervate the neck muscles and thus give rise to secondary torticollis (34).
Most cases of torticollis caused by ligament or muscle damage respond well to analgesics and anti-inflammatory medication. Most frequently, spontaneous improvement and normalisation of the displacement are achieved within a week (35). However, when the cause is atlantoaxial rotatory fixation the condition may persist despite medication or a cervical collar. Where an early diagnosis is made, it is however possible for most patients with this condition to be treated successfully with closed reduction without sequelae. Some patients in the early phase even achieve reduction during light manipulation in connection with examination and X-ray diagnostics. With a case history of up to 30 days, anti-inflammatory and, possibly, muscle-relaxant medication should be tried for 1 – 2 weeks combined with light traction and a cervical collar (22). Where traction is started within 30 days of symptom onset, the result in 90 % of cases is reduction and normal movement at the atlantoaxial joint (11).
If attempts at reduction and to relieve pain and improve movement are unsuccessful, one should attempt closed reduction with skull traction, physiotherapy and muscle relaxants. Patients lie in skull traction for an average of two weeks. After a CT scan has confirmed that the displacement is reduced, the patient wears a cervical collar for six weeks. Individual patients do however reluxate twice on average (11), and some doctors then recommend a renewed attempt at reduction (9, 22). It has been shown that for up to 2 – 3 months after the onset of torticollis, traction combined with a cervical collar is usually sufficient to correct the displacement (6, 9, 36 – 38). Where atlantoaxial rotatory fixation persists for more than 2 – 3 months, most attempts at closed reduction are unsuccessful (9, 36, 38 – 40), and surgical treatment with open reduction and internal fixation may be necessary (2, 6, 39, 41, 42).
To our knowledge, only one prospective study has been done of the diagnosis, treatment and outcomes of atlantoaxial rotatory fixation (42). The recommended therapeutic strategy is otherwise based chiefly on retrospective follow-up studies.
Our experience with unsuccessful attempts at closed reduction in three patients with symptom duration of more than five months is in line with reports that skull traction is not sufficient to reduce late-diagnosed atlantoaxial rotatory fixation (14, 37). The condition can be life-threatening (2) and instances of «sudden death» have been described in connection with attempts at closed reduction of a fixed abnormal rotational position of the atlantoaxial joint (6).
Surgical treatment of atlantoaxial rotatory fixation does not lead to normalisation of the anatomical conditions in the neck. Rotational movement after surgical fixation is reduced by about 25 % (6). In 30 % of patients it has also been shown that a process of degeneration arises at the adjacent level within ten years of surgical fixation (16). The consequences of unsuccessful reduction and persistent displacement are however so great that we believe surgery is the best therapeutic alternative after one unsuccessful attempt at closed reduction. In the case of severely delayed diagnosis, open reduction and fixation should be done without first attempting closed reduction.
Limitations in this review are owing to the small and selective patient sample, that the data were obtained retrospectively and that we have had no comparison groups. Thus it is difficult to create guidelines for the treatment of this patient group on the basis of our material. However, there is an international tendency towards surgical treatment of atlantoaxial rotatory fixation in excess of three months, although the point in time for recommended surgical intervention varies (6, 42).