Scaphoid fracture of the wrist is a common condition, and by far the most common carpal bone fracture (1). The cause is almost always a fall onto an outstretched arm with dorsal flexion and radial deviation of the wrist (Fig. 1). The problem is slow healing because of the poor blood supply, and risk of avascular necrosis.
Figure 1 The most common injury mechanism in cases of scaphoid fractures
The fractures show the full range of displacement. There is often little pain, with the result that the injury may be overlooked. Fractures may be difficult to detect on X-ray images, and oblique projections may be necessary. If uncertainty remains after an ordinary X-ray examination, it can be supplemented with a CT or MRI scan. In the case of uncertain diagnosis, it is also usual to take a further X-ray after about 10 days. The treatment is primarily plaster cast immobilisation, but the fracture may take a long time to heal because of a poor blood supply (2). Surgery may be indicated when there is relatively extensive displacement, delayed healing or pseudarthrosis (non-union), which about 5 – 10 % of these patients develop (3 – 5). With displacement of > 1 mm, surgery is usually indicated. Surgery should also be considered in the event of non-radiographic union after 4 – 6 months with a plaster cast (6).
Surgery entails screw fixation, a bone graft or both, as well as cast immobilisation (7). Pinning is also used. Suspicion of perilunar instability strengthens the indication for surgery (8). Primary surgical treatment with screw fixation of undisplaced or minimally displaced fractures has also been tried, but is not recommended as a routine approach (2, 9, 10). The operation can be performed using either open surgery, or combined percutaneous and arthroscopic technique. Undisplaced fractures can be operated upon with percutaneous screw fixation alone. Vascularised graft from the radius is also used for cases of non-union (11).
The purpose of this study was to map the incidence of scaphoid fracture generally and the treatment of this condition in our department, as part of our quality assurance work.
Material and method
All patients with scaphoid fractures who were treated in the Orthopaedic Section of Haugesund Hospital from 1987 up to and including 2011 were included in the study. Data were gathered by reviewing patient records according to diagnostic code. The data collected were used to create a separate data base which was cleared by the Data Protection Officer. Some of the material has been published earlier (12). The data were analysed by means of Statistica for Windows, Release 10 B (Stat Soft Inc., Tulsa, OK).
Results
415 patients with scaphoid fractures were included. 302 (73 %) were men. The average age at the time of the injury was 35 (range 9.5 – 97.4 years) and lower for men than for women (30.8 compared with 46.3). 48 % had a fracture on the right side. The injury mechanism is known for 410 patients. 345 (84 %) of them had had a fall. 65 patients had suffered various types of crushing injury or been in traffic accidents. Seven patients had another carpal fracture in addition – 16 radius fractures and three metacarpal fractures. Three had lunate luxation. 336 (81 %) received primary treatment of cast immobilisation including the basal phalanx of the thumb. 18 (4 %) underwent surgery within 24 hours due to the extent of the displacement. Open reduction with screw fixation using a Herbert screw was used as the primary surgical method. In cases of radiographic failure to heal or non-union, bone grafts were also performed with a corticospongioid graft and a plaster cast for at least two months. Both dorsal and volar approaches were used in the operations, according to the surgeon’s preference.
61 patients (15 %) had fractures that went untreated for a long time – from several months to a year – either because the patient himself or herself ignored the injury or because the injury was initially incorrectly evaluated by the primary contact. Because of persistent pain in the wrist, X-rays were subsequently taken which showed a fracture.
30 patients were followed up at other Norwegian or foreign hospitals. We have information about the final outcome for 385 patients (93 %), including 77 who had surgery. Only these 385 patients with a known final outcome are included in the following analysis of results (Fig. 2).
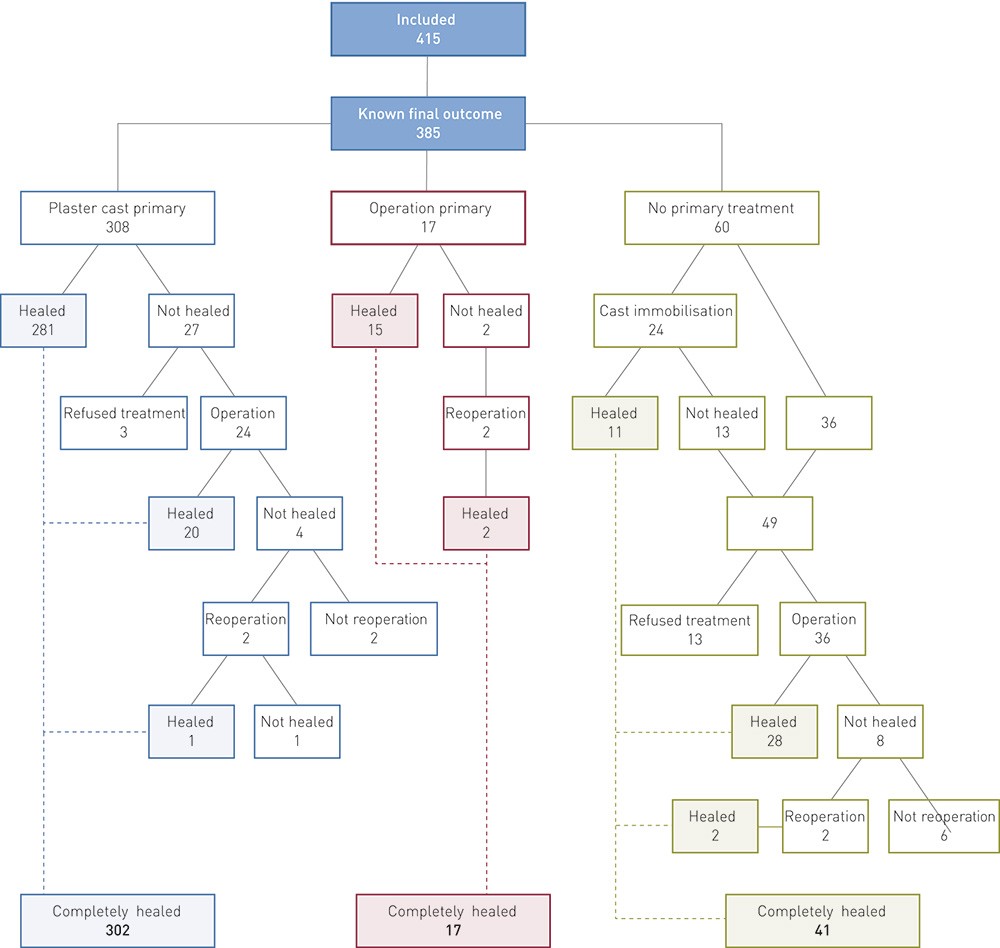
Figure 2 The course of treatment for the 385 patients with a known final outcome
Primary cast immobilisation of 308 patients gave satisfactory radiographic union in 281 (91 %). Failure to heal or non-union were observed in 27. Three refused further treatment. 24 underwent surgery, and the fractures of 20 of them were found to have healed. Two of the remaining four were re-operated upon, and one of them healed. The final outcome for this group was healing of 302 of 308 (98 %), while six (2 %) had persistent non-union.
17 underwent surgery as primary treatment do to the extent of the displacement, and the fractures of 15 (88 %) healed. The remaining two underwent successful reoperation, so that all members of this group were ultimately healed.
60 patients went a long time without treatment (ranging from one month up to several years); 24 patients were treated with cast immobilisation after a relatively short delay (> 3 months) and 11 were healed. 13 of the remaining 49 refused further treatment and 36 underwent surgery, with healing in 28 cases. Two were successfully reoperated upon, so that the final outcome was healing of 41 of 60 (68 %) in this group. 19 patients (32 %) developed persistent non-union.
A total of 66 patients (17 %) were found to have non-union, which was associated with delayed immobilisation (75 % versus 6.5 %). 50 patients with non-union underwent surgery. Of these, 39 (78 %) were healed after the first operation and 42 (84 %) after reoperations. 42 of the patients with non-union (63 %) were ultimately healed. 41 of 325 patients (13 %) who had received appropriate treatment, and 36 of the 60 whose primary treatment had been delayed (60 %), were regarded as requiring an operation. A total of 77 patients underwent surgery, 17 of them as primary treatment. Ten underwent surgery for failure to heal and 50 for non-union after an average of 23 months. Of the 77 who were operated upon, satisfactory healing was found in 63 (82 %) after the first operation and in 68 (88 %) after six reoperations. Whether the operations were for displacement, delayed healing or non-union made no difference to the frequency of healing.
Six patients first underwent surgery for displacement, failure to heal or non-union and were then reoperated upon with a further bone graft and fixation after an average of 15.3 months. Five of them were healed.
In total, the fracture was healed in 360 of 385 cases (93 %). The remaining 25 patients (7 %) with symptom-free or almost symptom-free non-union refused further treatment. 19 of these came from the group with delayed primary treatment.
Discussion
The age and gender distribution in this material is approximately the same as in other material (4, 13, 14). We only had one patient who was less than 10 years old. This is consistent with scaphoid fracture being relatively uncommon in children (15 – 17). 15 % of our patients had fractures that went untreated for a long time – this is consistent with the fact that scaphoid fractures are often overlooked because there are few symptoms and few clinical findings (18). The diagnosis is often uncertain, and only about one third of the patients for whom there was clinical suspicion of scaphoid fracture had a definite fracture. This is also roughly consistent with other reports (19). Early follow-up with special images or an MRI scan (19) are therefore often necessary, and in the majority of cases will disprove the suspicion or show fractures of other carpal bones (6, 16, 18),
The number of patients presenting annually rose during the inclusion period (data not shown), which may be due to the introduction of MRI scanning at our hospital in 2002 leading to fractures that would not have been discovered in ordinary X-ray images now being registered. The hospital’s catchment area was also expanded during the inclusion period. Our routine treatment for undisplaced fractures involves immobilising the proximal phalanx of the thumb. Whether it is necessary to immobilise this phalanx is a matter of controversy (14, 19). According to a number of studies, immobilisation can be carried out as for a common radius fracture (14, 20, 21). The duration of the immobilisation will depend on both X-ray images and clinical findings (6). The fact that immobilisation resulted in healing in about 90 % of the patients in our material is consistent with other reports (6, 9). We did not use surgery for undisplaced fractures, as some recommend (22). Whether surgery is indicated for undisplaced scaphoid fractures is a controversial issue (2, 23).
We only used reduction and screw fixation as the primary treatment for displaced fractures (> 1 mm diastasis), and this was in combination with cast immobilisation. Screw fixation may also be used with percutaneous technique (10) or with a combination of percutaneous and endoscopic technique (24). Surgery may be performed from both the volar and the dorsal side (25). In theory, operation from the volar side is safer for the circulatory system, while a dorsal approach gives readier access (25). No difference in final outcome has been documented (25). The conclusion that late (over a month delayed) immobilisation leads to a higher incidence of non-union, as in our material, is consistent with other studies (6, 7, 18, 26). The finding that approximately 90 % of non-union operations result in healing is consistent with another study (27). About 12 % of our patients had to have an operation, and some of them reoperation, because of non-union. This is also consistent with other reports (3, 4). An extra check-up after six months is recommended for early detection and treatment of non-union (3).
Bone grafts with and without screw fixation are the principle surgical method for the treatment of non-union (3). We have no experience of vascularised bone grafts, which have yielded good results (11). Some are of the view that asymptomatic or accidentally discovered navicular non-unions can remain untreated (16); others recommend operation of symptom-free non-unions to prevent the development of radiocarpal arthrosis (3, 6). With regard to this latter condition, there is often little consistency between X-ray images and clinical findings (4).