The increased risk of terrorist acts that could involve the use of radioactive sources calls for us to be prepared that a major radiation incident may occur in our country as well. On the basis of a manual published recently by the Norwegian Center for NBC Medicine, Oslo University Hospital Ullevål, a centre for disaster medicine, we here present the main principles for medical treatment of radiation injuries – from first aid at the scene of injury to hospital treatment.
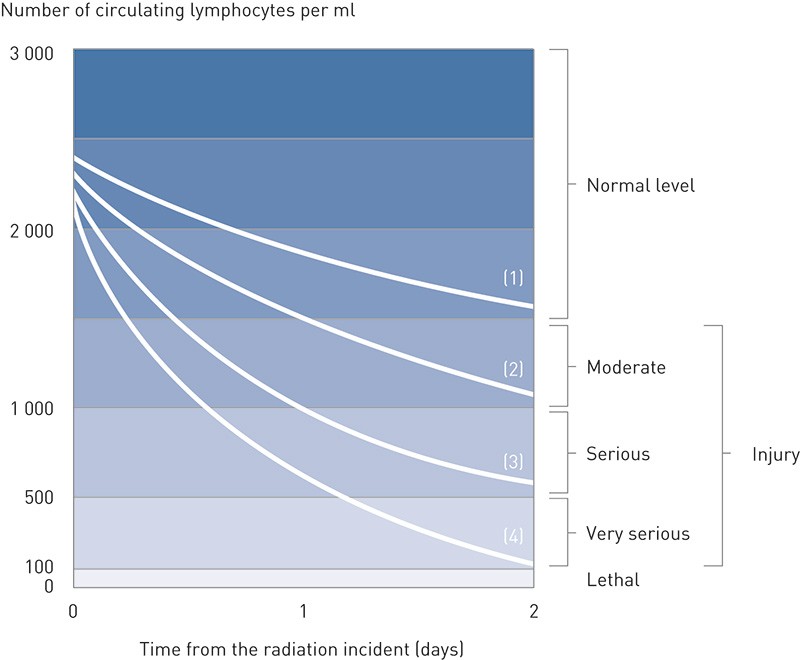
Figure 1 Changes in the lymphocyte count during the two first days after whole-body irradiation as an indication of the degree of severity of an expected radiation injury (12)
Exposure to harmful radiation occurs very rarely in our country, and only one case resulting in serious health injury is known to date (1). The risk of a major nuclear disaster that would involve a large number of people has been deemed to be minor, since Norway has no nuclear power plants or other nuclear industries. The changed threat picture, with an increased risk of terrorist acts involving the use of radioactive sources (2, 3), calls for the preparation of clear plans for responses to major radiation incidents.
Sources of radiation can be used for terrorist attacks in various ways. One possible variant would be to place a hidden source of radiation in a public location. This was used for a theoretical exercise arranged by the Norwegian Radiation Protection Authority in 2008, the scenario for which was that members of a terrorist organization had placed a radioactive source under a seat in an underground train. It was stated that the source had been hidden there for approximately 18 hours, and its strength was estimated so that if a person had been sitting in this seat for the entire stretch of the underground line in question, he or she would have received a radiation dose equal to approximately 5 Gy. This radiation dose is life-threatening, but survival is possible if intensive treatment is provided. In this imaginary example, it was reported that two persons had been exposed to this radiation dose. In addition, it was assumed that another 52 passengers had been exposed to harmful radiation, but in somewhat smaller doses (Øyvind Gjølme Selnes, Norwegian Radiation Protection Authority, personal communication).
Another possible use of a radiation source for terrorist purposes involves so-called «dirty bombs», i.e. conventional explosives mixed with radioactive material. When such a bomb goes off, people in the vicinity will be exposed to radioactive dust. In those who are injured, wounds may become contaminated. Moreover, the site of the explosion and the adjacent area would be contaminated with radioactivity. Detonation of a dirty bomb would be likely to generate widespread fear, although this would probably expose the public to far smaller radiation doses than in the case of deployment of a radiation source (4). It is also assumed that a terrorist group with competence in nuclear physics may have a realistic possibility of producing and detonating an improvised nuclear device (5).
Guidelines for handling of radiation injuries
In 2012, the Norwegian Center for NBC medicine, commonly referred to as the NBC center (N = nuclear, B = biological, C = chemical), published a manual for the provision of medical assistance in the context of such incidents (6). The part of the book dealing with harmful effects of radioactivity (6, pp. 73 – 101) is largely based on existing international action programmes (7, 8). The manual describes principles for assessment of the scene of injury in the case of radiation accidents, criteria for selection of patients with regard to their treatment priority (triage), procedure for decontamination of patients who have been exposed to radioactive pollution and guidelines for medical treatment. Some of the main points in the action programme are outlined below.
In a radiation accident, a distinction is made between external radiation from a point source and the radioactive pollution described above. Primarily, external radiation is able to inflict acute health injury. External radioactive pollution, i.e. deposition of radioactive material on skin and clothing, will as a rule not entail any significant health injury if decontamination is undertaken quickly. It is desirable for decontamination to be undertaken before the patient arrives in the hospital, but treatment of life-threatening traumas or other serious medical conditions will have top priority. In such emergencies, a simplified decontamination is undertaken by removing all items of clothing. In dry weather, the degree of contamination will then be reduced by approximately 80 % (8).
In some radiation incidents, internal contamination may occur, i.e. a radiation source has entered the body, either by ingestion, inhalation or by penetration of the skin by radioactive material. In these cases, it is essential that treatment with antidotes is started as early as possible. Antidotes are drugs that can dilute or neutralise the source of radioactivity to limit absorption into the bloodstream or increase excretion. In Norway, the most relevant antidotes are stored at the NBC Center at Oslo University Hospital Ullevål.
Acute radiation syndrome
Acute radiation syndrome (6, pp. 93 – 101) is a clinical condition occurring when the entire body or large parts of it have been exposed to a dose of ionising radiation equal to 1 Gy or more (9). The most frequent cause will be external irradiation, but one case resulting from internal contamination is also known: Alexander Litvinenko developed acute radiation syndrome after having been poisoned with polonium mixed into a cup of tea (10).
Acute radiation syndrome is a well-defined disease entity that develops through multiple clinical stages in a dynamic process. The disease manifests itself initially through so-called prodromal symptoms, mainly nausea and vomiting, as well as stomach pains, diarrhoea and other symptoms. The prodromal symptoms are reversible, and are assumed to be caused by an excitation of the autonomic nervous system (7). The time that elapses before onset of the prodromal symptoms and their degree of severity reflect the radiation dose received. In the exercise scenario described above, it was assumed that in the two persons who had been exposed to the largest radiation doses, the prodromal symptoms would have appeared within approximately one hour.
eIt is assumed that radioactive radiation may affect all organs in the body (11), but the clinical consequences are likely to be greatest in the most radiation-sensitive organ systems, such as the bone marrow and the digestive tract. The time elapsing before the onset of symptoms depends on the dose rate and the radiation dose. In the exercise scenario described above, it was calculated that symptoms of bone marrow failure with granulocytopenia (infection) and thrombocytopenia (haemorrhage) would have appeeared in the two most heavily irradiated patients approximately 10 – 14 days after the radiation incident.
Mature lymphocytes are among those cells in the body that are most sensitive to radiation. After even moderate radiation doses, a reduced lymphocyte count in the blood can be detected within 1 – 2 days. This phenomenon is primarily used as a factor for estimating the radiation dose received during the acute stage (Figure 1) (12). After radiation doses in excess of approximately 2 – 3 Gy, symptoms of bone marrow failure can commonly be observed. Animal studies have shown that rapidly initiated treatment with granulocyte-colony stimulating factor that stimulates the remaining haematopoietic stem cells reduces the fall in neutrophil granulocytes and shortens the time in granulocytopenia after exposure to radiation. This is consequently regarded as the standard treatment in the case of acute radiation syndrome (13).
Allogeneic haematopoietic stem cell transplantation is considered in cases where the bone marrow is unlikely to regenerate spontaneously and other organ systems are not affected to a life-threatening degree (14). After radiation doses exceeding approximately 5 Gy, symptoms from other organ systems in addition to the bone marrow will also appear, primarily from the digestive tract, followed by the skin, the central nervous system and other organs (7). With the exception of drugs that stimulate the bone marrow, only supportive treatment is relevant, including empirical antibiotic treatment, prophylactic transfusions of thrombocytes to prevent haemorrhaging, monitoring of the fluid and electrolyte balance, and use of antiemetics for nausea, vomiting and similar.
It has been shown that if one or more organ systems in addition to the haematopoietic system are affected, the patient’s condition will be significantly exacerbated (15), and in many cases a terminal stage with multiple organ failure will develop, similar to that seen, for example, in multiple-traumatised patients. At the time, this observation gave rise to a change in notions about the pathophysiological mechanisms involved in acute radiation syndrome. Previously, each organ system was considered in isolation, whereas it has now become clear that acute radiation syndrome is a manifestation of a generalised process involving interplay between several affected organs, mediated by cytokines and other signal molecules (16). As of today, no established course of treatment that has an effect on the mechanism behind multiple organ failure is available.
Prognosis assessment at the acute stage
If an acute radiation incident should occur, it is crucial to obtain an early overview of the magnitude of the radiation doses to which the patients have been exposed to be able to predict the course of illness and assess the medical care each patient will need. In the case of a major radiation incident involving a large number of people, it will also be essential to be able to assess the level of resources required, given the total extent of the situation. Assessments at the acute stage are mainly based on so-called clinical dosimetry, i.e. data regarding the prodromal symptoms and changes in the lymphocyte count during the first two days (Figure 1).
As an aid in such situations, an international working group has prepared a scoring system in which the patients are tentatively divided into three prognosis groups on the basis of a total assessment (Table 1) (17). In addition to clinical dosimetry, the initial dose assessment is also based on so-called biological dosimetry, i.e. an investigation of specific chromosome changes in the circulating lymphocytes. The proportion of affected chromosomes reflects the radiation dose (18). In the Nordic countries this investigation is undertaken by the Finnish radiation protection authority. Five days are needed before a response is available.
|
Table 1 Prognostic scoring system for the first 48 hours, based on prodromal symptoms and lymphocyte measurements. Group 1 comprises patients who judging from their symptoms are assumed to have received a radiation dose of less than 3 Gy. They will not require hospitalisation. Group 2 has symptoms consistent with an irradiation of 3 – 5 Gy. They will need hospital treatment, although in a regular ward or as outpatients. Patients in Group 3 are assumed to have received a radiation dose in excess of approximately 5 Gy, a potentially life-threatening dose. These patients should be provided with intensive care. After Gorin and collaborators (17).
|
|
Group 1 (< 3 Gy)
|
Group 2 (3 – 5 Gy)
|
Group 3 (> 5 Gy)
|
|
Time to symptom onset
|
< 12 hours
|
< 5 hours
|
< 30 minutes
|
|
Erythema
|
None
|
Moderate
|
Prominent
|
|
Asthenia
|
Minor
|
Moderate
|
Prominent
|
|
Nausea
|
Minor
|
Moderate
|
Prominent
|
|
Vomiting
|
Once
|
1 – 10 times
|
> 10 times
|
|
Stools/diarrhoea
|
2 – 3 times, firm
|
2 – 9 times, soft
|
> 10 times, watery
|
|
Stomach pains
|
Minimal
|
Strong
|
Intense
|
|
Headache
|
None
|
Moderate
|
Prominent
|
|
Fever (°C)
|
< 38
|
38 – 40
|
> 40
|
|
Blood pressure
|
Normal
|
Periodic hypotension
|
< 80 systolic
|
|
Lymphocytes/ml
|
|
|
|
|
24 h
|
> 1 500
|
> 1 500
|
> 500
|
|
48 h
|
> 1 500
|
< 1 500
|
< 100
|
|
Follow-up
|
Outpatient
|
Regular ward/outpatient
|
Intensive care
|
The NBC manual has been prepared partly to provide guidelines for the centre’s own work and partly as an aid to doctors and other medical personnel who will assess the condition of people who have been exposed to radiation. In such situations, the NBC centre can also be contacted for direct consultations. The content of the NBC manual represent the centre’s own viewpoints. A proposal for a national action programme for NBC medicine is currently being prepared.