«According to the preliminary investigation by the local police, the child is said to have been born on Friday the 14th of this month between 11 and 12 at night. The child’s body was found in the bed at the home of the mother by Jan OE and Josef HE, whose wives had received a confession from the maid that she had given birth to a child in secret. The accused later told the police that when she came to her senses after the birth, she saw the child lying with its head between her knees, and the legs (of the child) up against her genital area with the umbilical cord and afterbirth attached. She understood then that the child was dead and laid it on its right side in the bed. These men took it in the clothes in which it was wrapped and brought it to a nearby storehouse, where it has lain until now. She is 28 years old and has not previously given birth.» (1).
Forensic examination of the body, or so-called «legal autopsy», was performed by the district medical officer and a court-appointed doctor in private practice one week after the birth in November 1912.
This story was part of everyday life in Norway a hundred years ago, and forensic examinations of deceased newborns were not an uncommon task for doctors. In Francis Gottfred Harbitz’s (1867 – 1950) textbook of forensic medicine of 1915 he states that 20 – 25 % of all forensic autopsies concerned possible «infanticide»; however a review of the autopsies carried out in the period from 1910 to 1912 showed that as many as 36 % of the forensic autopsies were related to this issue (2 (p. 322), 3). The forensic examinations were devoted to deciding whether the child was full-term or premature, but viable; whether it had been alive during and after the birth; whether it had died within 24 hours of the birth; and what was the cause and manner of death, that is, whether the death was the result of disease, accident or murder (Fig. 1) (2). An important criterion for deciding whether the child was alive after the birth was that the lungs floated in water, the so-called «lung test» or «lung flotation test». In the absence of visible injury or malformation, the cause of death was often considered to be suffocation or asphyxiation (Box 1).

Figure 1 Typical formulation of a conclusion from the autopsy of a full-term newborn (Case 136/1912)
BOX 1
Textbook of Forensic Medicine 1915 (2)
Criteria for the child having breathed post partum (Chapter XII):
Positive lung test: Lung tissue floats in water. To be first tested with all the thoracic organs including trachea, thymus and heart, thereafter with each lung, pulmonary valves and single sections of lung tissue
Air in the gastrointestinal canal: Air in the stomach, possibly in the small intestine (to be tested if relevant using the water flotation test)
Criteria for death by asphyxiation (by whatever cause) (Chapter VI):
Petechiae and ecchymoses, primarily in mucosa and over internal organs
Hyperaemia of internal organs (venous hyperaemia)
Liquid blood
Pulmonary oedema
Although others are said to have observed the phenomenon previously, the «lung test» is traditionally attributed to the German doctor Johannes Schreyer (1655 – 1694) (4, 5). In 1690 Schreyer described a case of suspected infanticide in which the lungs of the exhumed child’s corpse sank, resulting in the acquittal of the 15-year-old mother (5) (Fig 2). It is uncertain how early this type of examination was used in Norway, but it was in any case performed in 1782 by the regimental surgeon Rasmus Hess (1734 – 1803) in Kongsvinger (6). In earlier times the outcome of the test could literally be a matter of life and death for the mother: if a child born clandestinely had not been born alive, the mother could not be convicted of infanticide. In brief, the basic principle is that if a newborn child has breathed, the lung tissue at autopsy will be inflated with air and float in water, but if the child was stillborn, the lungs will not float. In clear-cut cases not only the lungs but the whole block of thoracic organs (lungs with trachea, thymus and heart) will float. Interpretation of the test is difficult when there is decomposition because this can produce gas which may give a false positive flotation test result. If resuscitation has been attempted with artificial respiration, the test will of course be positive as well.
Figure 2 In 1690 «the lung flotation test» was described as being used in a case of suspected infanticide. The lungs of the exhumed corpse of a child born of 15-year-old Anna Voigt sank, resulting in the girl’s acquittal (5)
In Norway, practice with regard to the examination of newborns was defined in the textbook of forensic medicine by Michael Skjelderup (1769 – 1852) of 1838 (7). Professor Francis G. Harbitz, who was a member of the Norwegian Board of Forensic Medicine from the time of its inception in 1900 and a resident expert witness at the Department of Pathology at the Rikshospitalet, led the way in his time in the training of Norwegian doctors (Fig. 3). At around the turn of the century Harbitz published works dealing with the so-called «lung test» and «death from asphyxiation» in Norwegian journals (8, 9). He set examination assignments on the subject for Norwegian medical students and as a member of the Board he described in annual reports the criteria for assessing whether newborns had breathed post partum (10, 11). In the same period a debate was escalating in Germany and France about the validity of the lung flotation test, and Harbitz commented on this discussion in detail for Norwegian readers (8). Based on individual cases there was also a debate in Great Britain about the problems of ascertaining whether the child was alive post partum (12, 13). The debate centred as much around findings of false negative lung tests, that is, lungs that sank even thought it was proven that the child had lived, as around the possible false positive results.

Figure 3 Francis Gottfred Harbitz (1867 – 1950), professor of pathology and a permanent member of the Norwegian Board of Forensic Medicine 1900 – 1946. Photo: Wikimedia Commons
Sources of error in the criteria used for assessment of life and cause of death are discussed in detail in Skjelderup’s book. In Harbitz’s article from 1902, as well as in the textbook from 1915, caution is advised in drawing a conclusion as to the extent to which a child has or has not lived post partum. Based on these warnings, we have looked more closely at how forensic examination of deceased newborns was practised in Norway 100 years ago.
Material and method
We have reviewed all cases concerning full-term deceased newborns in the archives of the Norwegian Board of Forensic Medicine at the National Archive in Oslo, from 1910 up to and including 1912. The review of the archived material is described in detail in a previous work (3). We recorded gender, weight, length, result of the lung test and signs of suffocation /asphyxiation, as well as the conclusion and any comments by the Board members. We divided the period from birth to autopsy into four groups: 1 – 2 days, 3 – 7 days, between one week and one month, and more than one month. Cases for which no interval of time was given, but where decomposition was mentioned in the text, were also recorded as a separate group. Because the cases were more than 100 years old, no waiver of confidentiality was necessary.
Results
Ninety-five cases concerned deceased newborns. Seventy-five of the newborns were assessed as full-term. One child had evidently suffered intrauterine death (macerated at birth) and was therefore excluded from the analysis. Altogether 74 newborns, of which there were 33 males, 33 females, and eight whose gender was not indicated, were therefore included. Average weight and length was 3200 g and 52 cm for boys, 3005 g and 51 cm for girls.
Figure 4 shows the conclusions with regard to whether the child had breathed, compared with time elapsed post partum, and autopsy. There was generally a correlation between the conclusion from the forensic examination on the extent to which the child had lived, and a positive lung test, but also other criteria, such as intestinal gas, were included in the assessment. Only few of the children were assessed as not having breathed, even when significant decomposition was described, and the decomposition of other organs was seldom taken into consideration when the lung test was assessed.
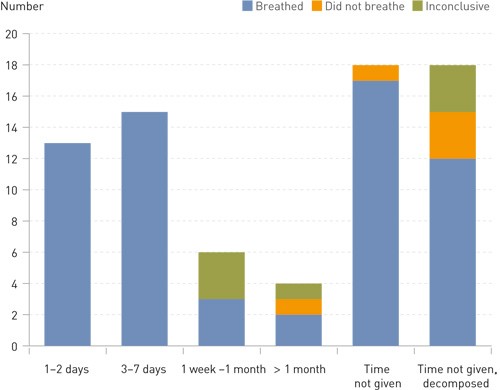
Figure 4 Assessment of whether the child had breathed post partum viewed in relation to time between birth and autopsy. Full-term newborns (n = 74)
Case 162/1910 is a typical example: «Forensic dissection of the body of a newborn child, found in the lake at Grönlien – The body of a child who, although the genital organs are very decomposed, can still be recognised as a male child – The lungs are set far back in the air sacs, which also contain large quantities of a red-coloured, clear fluid. On the surface of the lungs, particularly on the upper sections and along the front edge, there are numerous large, tightly packed bubbles of gas, partially in the lung tissue, and partially and significantly on the surface beneath the pleura. The majority, and the largest, of these bubbles of gas are in the right lung. – The lungs float with the greatest ease, together with the heart and the thymus. –With regard to the adrenal glands and pancreas, which like the other organs show themselves to be severely decomposed, there is nothing to remark. – All the intestines are extremely bloated with gas. – Conclusion: – Although the decomposition in this case is very pronounced and presents obstacles for the assessment of the finding in the external organs, we nevertheless believe we may conclude, taking into account the condition of the lungs and the gastrointestinal tract, that the child has lived and breathed after birth.»
Francis Harbitz, who incidentally was one of the two expert witnesses, and the other members of the Norwegian Board of Forensic Medicine, signed the declaration without comments.
In only two cases does decomposition result in a positive lung test being overridden. Municipal medical officer Einar Stoud Platou (1861 – 1946) and district medical officer Hakon Knudtzon (1857 – 1926) determined a positive lung test when performing the autopsy on a female child who was found in Stjørn Fjord in the middle of summer and concluded that the result «could be caused by gas produced during decomposition, taking into account the high level of decomposition of the other organs» (14). The Board made no comments about this conclusion. A similar conclusion, made two years later by district medical officer Konrad Adolf Haug (1868 – 1935) and Anders Falck (1873 – 1961) from the autopsy on the bodies of two infants found in a sack in a lake in Namdalen, was discussed by the Board. They assessed whether the conclusion would have been the same if the bodies had not been sunk in the lake, but agreed that it was not possible to draw any definite conclusion as to whether the children were born alive or not (15).
The expert witnesses were more reserved in their statements on cause of death, especially after some time had passed. Asphyxiation was given as the possible cause of death for less than half of the full-term infant corpses (33 of 74). Nevertheless, reports giving asphyxiation as the probable cause of death in highly decomposed corpses were signed without comments by the Board, even in cases where few criteria were fulfilled:
«The body appears to be in an advanced state of putrefaction and gives off an intense odour. –The face and left side of the head are contaminated with more or less dried blood mixed with sawdust, so that the contours of the face are indistinguishable, and eyes, nose and mouth may only be distinguished by way of suggestion. – There is no exudation of blood on the conjunctiva palpebrarum. – no exudation detected – The membranes of the mouth, larynx and trachea are blue-red. – Conclusion: – The cyanotic condition of the respiratory organs and their membranes indeed point to the possibility of death by asphyxiation immediately after the birth – (16).
Moreover, it is «congestion of the internal organs and exudation of blood on the surface of these, and the dark, liquid blood» that essentially make for the description of cases of death from asphyxiation, irrespective of the condition of the body (17).
«Asphyxiation» was given as the cause of death for 33 full-term newborns. Of these, autopsies were performed on 15 within seven days after the birth, three were the subject of autopsy between one week and one month post partum, and for 15 the time of autopsy was not given. Five of these 15 are described as being in a state of decomposition.
Only in one case did the Board make a comment on a conclusion of assumed death from asphyxiation. The body, for which the time of birth was unknown and which had to be thawed for two days before it could be examined, showed some «ecchymoses» on the pericardium and liquid, non-coagulated blood in the heart. The blunt statement of cause of death (Cause of death: asphyxiation) was criticised by the Board, which had no objections to the conclusion itself, but recommended a less direct phraseology (18).
Discussion
One hundred years ago, examination of dead newborns constituted a large proportion of forensic autopsies. This reflects the extent to which the textbooks were devoted to the topic. In Michael Skjelderup’s Lectures on legal medicine from 1838, as many as 44 of 211 pages are devoted to the subject of newborns, while Francis Harbitz in 1915 devotes 58 of 450 pages to a description of the topic (2, 7).
Artefacts of decomposition were a major problem, and in the annual report from 1911 of the Norwegian Board of Forensic Medicine, an attempt was made to set out the procedure regarding rotten corpses: «With regard to the significance of bubbles of air and gas in the lungs of a decomposed infant, the Board makes the following general statement on the matter: when a decomposed infant is produced for examination, a finding of bubbles of gas or air in the decomposed lungs will as a rule indicate that respiration has occurred and that the child therefore was alive post partum. Notwithstanding, when the decomposition is very advanced, this cannot be stated with certainty» (19, p. 4).
However, no definition was given of what was meant by «very advanced». In the textbook from 1915 Harbitz emphasised that the finding with regard to the lungs had to be seen in connection with the extent of decomposition of the other organs:
«In this context it must be remembered that lungs that contain no air decompose more slowly; a stillborn child with no air in its lungs and intestinal canal decomposes from the exterior. On the other hand, if the lungs contain air, they will decompose rapidly, and more rapidly than the other internal organs, whose signs of decomposition must always be described in detail in such cases. (A flotation test should always be performed on the liver, spleen and kidneys.) – If the decomposition is very advanced, so that the lungs are completely saturated with gases produced by decomposition which are also present in the other internal organs, the circumstances are difficult to judge and it is impossible to arrive at a conclusion with any certainty» (2, p. 339).
In addition, Harbitz made reference to his article on the subject from 1902, in which it was emphasised that the custom in Christiania had been to assume that foetal lungs could produce gas during decomposition and that a cautious approach was therefore recommended (8). Nevertheless, the conclusions reached in the majority of the expert witnesses’ declarations that we studied indicate that neither the expert witnesses nor the members of the Board followed these recommendations for a cautious approach in practice.
The effect of decomposition was only discussed in relation to the lung test. The significance of decomposition for the criteria for asphyxiation was not queried, either in the textbooks or in Harbitz’s articles. When it came to signs of asphyxiation in general, Harbitz was again cautious. Both in the article from 1899 and the textbook from 1915 he urged a significantly moderate interpretation and concluded that none of the signs of asphyxiation were pathognomonic, but could also be seen in a number of other causes of death (2, 9). Examples of differential diagnoses of asphyxiation mentioned in the textbook are death as a result of skull fracture or cerebral hemorrhage, congenital syphilis, sudden death in general or from diseases of the mother. However, these stipulations were not embodied in practice in this area either. The Board had no comments on the fact that the medical expert witnesses repeatedly used dark, liquid blood, empty heart chambers and other dubious criteria as arguments for their conclusions on presumed death by asphyxiation.
The absence of association between theoretical knowledge and practice is striking. The explanation may lie in the fact that the expert witnesses were imprinted by circumstances outside of the examinations themselves, namely by the social conditions. Clandestine births and infanticide were a major problem at that time (3). There was therefore a high probability that the infant had been killed or left to die, irrespective of the condition of the infant’s corpse. If the expert witnesses had taken seriously the warnings about the artefacts of decomposition and uncertain signs of asphyxiation, they would have been unable to form a definite conclusion in the majority of the cases. It was, and is, difficult to repeatedly express no fixed opinion, not only before a court, but also in terms of one’s own self-image as a doctor and a scientist.
Today many of the same criteria are still used to assess cases of death in newborns, but with a significantly greater degree of caution. The lung test is still controversial and is not performed where there are traces of decomposition (20, 21). The test is generally supplemented by x-ray images for better assessment of the extent of air in the lungs. For the assessment of deaths by asphyxiation, only petechiae and cyanosis/stasis in the face are relevant signs today, but still with the same stipulations indicated by Harbitz: that there are no specific signs of asphyxiation. An important difference from practice one hundred years ago is also that suspected infanticide is now investigated by doctors with special competence in forensic pathology and not by individual district medical officers.
A result of the statements by expert witnesses was that women were imprisoned for infanticide. There is reason to believe that many of these may have been innocent. The material from the archives of the Norwegian Board of Forensic Medicine is therefore a useful reminder that science is constantly changing. In their role as administrators of scientifically based facts, doctors have a particular responsibility, not least when they use their knowledge in the role of expert witnesses.
