A woman in her nineties was admitted to hospital with acute abdominal pain and clinical signs of diffuse peritonitis. She had a number of other illnesses for which she was taking medication. The examination showed an unusual cause of acute peritonitis, in which the use of tablets played a major role.
A woman in her nineties was admitted to hospital with acute abdominal pain. She had recently been discharged following treatment for severe acute cholecystitis with intravenous antibiotics and percutaneous biliary drainage. She was taking a number of drugs for other diseases, in addition to peroral antibiotics and analgesics following her former hospitalisation. She had reduced vision and used a dental prosthesis. On admission she was alert and aware of the situation, but her general condition was rather poor and she reported diffuse abdominal pain. She had a low-grade fever (38.3 °C), slight tachycardia (regular pulse of 83 beats per minute), slightly reduced oxygen saturation in ambient air (89 %) and normal blood pressure (151/83 mm Hg). Clinical examination of the abdomen revealed distension on palpation and general pressure and rebound tenderness.
Medical history and clinical examination pointed to an acute abdominal illness with peritonitis, raising immediate suspicion of inflammation or perforation of one of the hollow abdominal organs. A condition of this type often requires emergency surgery. Before any possible surgery, other conditions must be excluded that may present a similar clinical picture but for which surgery should not be performed: acute myocardial infarction, basal pneumonia, basal pulmonary embolism, renal and ureteral stones, and certain abdominal disorders for which emergency intervention is generally unnecessary – acute pancreatitis, acute cholecystitis and acute uncomplicated diverticulitis. Investigation of vascular causes of acute abdominal pain must also be considered: acute thromboembolism or visceral artery aneurism/rupture.
The patient was examined using laboratory tests, ECG and abdominal CT scan with intravenous contrast medium. The laboratory values on admission revealed elevated inflammatory markers, but otherwise normal values: Hb 11.5 g/l (11.4 – 15.3 g/l), leukocytes 19.5 · 10⁹l (3.5 – 8.8 · 10⁹l), CRP 210 mg/l (< 5 mg/l), Na 139 mmol/l (137 – 145 mmol/l), K 4.5 mmol/l (3.6 – 5.0 mmol/l), creatinine 87 μmol/l (56 – 110 μmol/l), amylase 21 U/l (10 – 60 U/l, bilirubin 18 μmol/l (< 25 μmol/l), alaninaminotransferase (ALAT) 22 U/l (10 – 45 U/l), alkaline phosphatase (ALP) 82 U/l (35 – 105 U/l). ECG showed sinus rhythm with no signs of ischaemia. Abdominal CT scan with contrast medium showed normal basal pulmonary cross-section. Signs were observed in the abdomen of local inflammatory changes in the small intestine with a space outside the gastrointestinal wall related to a foreign body in the intestinal lumen (Fig.1).
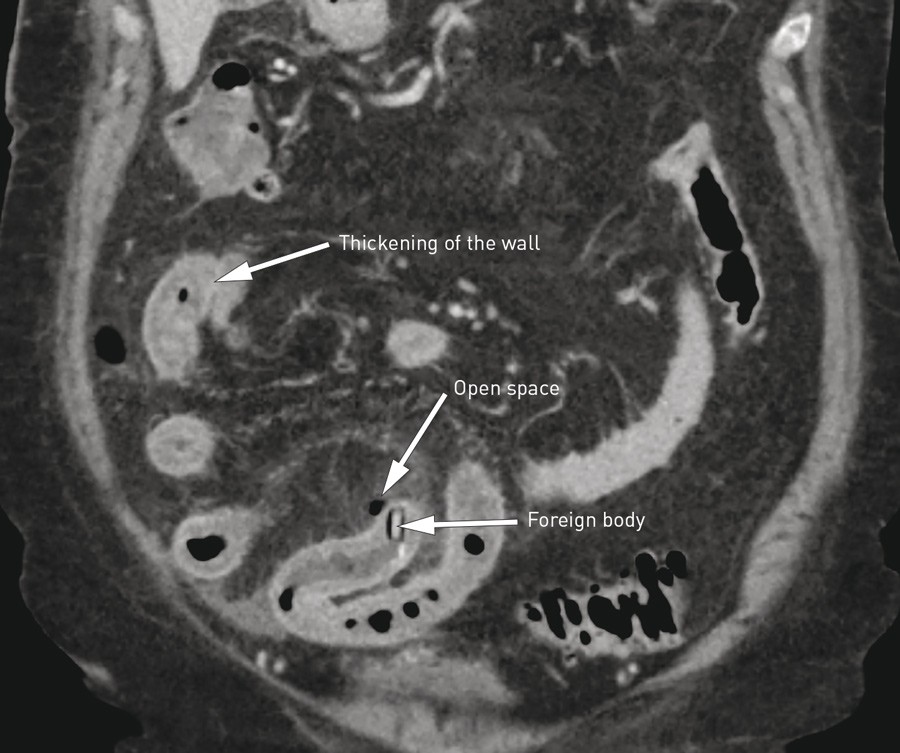
Figure 1 Abdominal CT scan shows perforation of the small intestine by a foreign body (tablet in blister pack) and thickening/oedema of the intestinal wall orally to the foreign body
The laboratory tests reinforced the suspicion of an inflammation. Normal haemoglobin values rendered a severe haemorrhage improbable, and normal ECG findings precluded acute myocardial infarction. Clinically the patient had diffuse peritonitis, in itself a classic indication for surgery. However, today an abdominal CT scan is usually performed on patients whose circulation is stable before treatment. A CT scan, preferably with intravenous contrast medium, is now the first choice for radiological assessment of acute abdominal pain and has replaced abdominal x-ray. If the patient has elevated creatinine values, the risk of contrast-induced nephropathy aggravation must be weighed against the additional benefit bestowed by intravenous contrast medium. If relevant, a CT scan can be performed without the use of contrast medium. Hydration prior to the examination may potentially reduce the risk of contrast-induced nephropathy. CT scans are now a widely available and rapid form of examination and often provides clinicians with a precise diagnosis and the possibility to target the treatment. In this patient, clinical findings and CT examination provided the diagnosis and the indication for surgery.
The patient underwent an emergency laparotomy, during which a sharp corner of foil from a blister pack was found protruding from the gastrointestinal wall (Fig. 2). This was treated with intestinal resection and primary anastomosis. Inside the intestine we found a blister pack with a tablet (Fig. 3). This had moved down the intestine and created longitudinal ulcerations before finally perforating the small intestine. The postoperative course following the intestinal resection was uncomplicated. However, choledochus calculi were revealed, which were removed by endoscopic retrograde cholangiopancreatogram (ERCP) over two sessions. This prolonged the hospitalisation somewhat, but 14 days after the surgery she was able to be discharged in a healthy condition.

Figure 2 Photo of small intestine with blister pack protruding

Figure 3 Photo of tablet in blister pack (retouched to avoid identification of the brand) in opened small intestine, with longitudinal traumatic ulceration and thickening of the intestinal wall
Discussion
The great majority of smaller foreign bodies that are ingested will pass through the gastrointestinal tract without giving rise to problems. Intestinal injuries can occur when the foreign body is sharp or indigestible, such as chicken bones, fish bones, toothpicks, nails or small, angular cake decorations (1 – 3) which can cause bleeding, ulceration, formation of fistulas or perforation. Gastrointestinal complications due to tablet packaging are uncommon, but have been described previously (4). Intestinal perforation often occurs in the terminal ileum, a few centimetres above the ileocaecal valve. Perforations can also occur in other parts of the small intestine – the caecum, sigmoid colon or duodenum (5 – 8). Children, as well as elderly people with reduced vision and/or other serious illnesses, are more susceptible to this risk.
Tablets are often sold in boxes containing tablets in plastic cavities sealed within a card covered with aluminium foil (blister packs). The tablets are intended to be pushed out through the aluminium foil before ingestion. Sometimes there are perforations between the individual blisters to make it easier to press a dose or a tablet out while still protecting it. Many cards do not have these perforations and may need to be cut away from the card if single-dose units are desired. Our patient had swallowed a single tablet in its blister pack. The blister pack was broken or cut loose from the card and consisted of a hard, square-shaped object with very sharp corners which she was handed and swallowed together with her other regular drugs. The fact that she had just undergone another illness which had left her weak, and that she had poor vision and reduced sensitivity in her oral cavity due to dental prostheses, were among the reasons she did not notice that the tablet was still in its blister pack and therefore swallowed it whole.
Clinically it is impossible to distinguish perforations of the small intestine from perforations in other parts of the gastrointestinal tract. An abdominal CT scan with contrast medium is the best form of examination for rapid determination of the cause of acute conditions of the abdomen, in this case a foreign body, and for localisation of the intestinal perforation (8). Laparotomy with small bowel resection is necessary. Laparascopic intervention may be an alternative method.
In future years the number of elderly, ill patients taking tablets will steadily increase. One way of preventing this condition is to use other forms of single-tablet packaging than blister packs.
