The scaphoid bone (os scaphoideum) is one of eight bones in the wrist. About half of the bone is covered with cartilage. It articulates with the radius, lunate, capitate, trapezoid and trapezium bones. Earlier cadaver studies revealed the major blood supply to the scaphoid to be retrograde, with entry into the bone around the distal pole. It was assumed to result in vulnerable circulation in the proximal part of the bone (1), like the femoral head in adults. In more recent cadaver studies, however, less vulnerable circulation has been found, with anastomoses to all parts of the scaphoid (2). This explains the good healing capacity given early diagnosis and treatment. With the exception of very distal fractures through the scaphoid tubercle (which almost without exception heal within six weeks with casting) all fractures are intra-articular. The combination of a small contact surface between the fracture fragments and extensive movement around the scaphoid when the wrist is flexed or extended result in a high risk of non-union if the fracture is not stabilised with a plaster cast or internal fixation (3).
Men suffer scaphoid fractures four times as frequently as women, with a peak in the age group 20 – 40 years. The estimated Norwegian incidence is 1 800 – 2 200 (4, 5), of which approximately 5 % are newly detected pseudarthroses (6). In 2006, almost all Norwegian hospitals and clinics treated acute fractures with cast immobilisation for 8 – 12 weeks. Most scaphoid pseudarthroses were referred to hand surgeons and underwent surgery with bone graft and internal fixation followed by cast immobilisation (7). The purpose of this review is to provide an overview of the assessment, treatment and outcomes of scaphoid fractures.
Method
We conducted the following literature searches in PubMed with given exclusion criteria:
«scaphoid» and «fracture» (filter: randomized controlled trial): 36 hits, 14 after exclusion.
«scaphoid» and «fracture» and «treatment» (filter: English, human and abstract available, last 40 years, search term in title or abstract): 281 hits, 111 after exclusion. 50 of the 111 were review articles.
«scaphoid» and «nonunion» or «non-union» (filter: English, human and last 40 years, search word in title or abstract): 159 hits, 59 after exclusion. 12 of the 59 were review articles, two were randomised studies.
We excluded articles in which scaphoid was not the subject and cadaver studies of anatomy, biomechanical or surgical techniques. Publications in which scaphoid fractures were mentioned as part of more extensive hand injuries (radial fracture, wrist fracture, ligament injury) were excluded. Epidemiological studies, articles on sequelae, individual case reports, expert opinions and reports were also excluded. After excluding duplicates, we were left with 160 articles. We read the abstracts of all these articles. The authors have extensive experience of treating wrist injuries and fractures of the scaphoid bone. This review is based on the prospective studies and what we regard as the most relevant and representative review articles/meta-analyses and retrospective studies, a total of 37 articles, in addition to our own experience of the issue.
Results
The quality of the studies
Despite the many publications about scaphoid issues, there are few randomised studies and none have been conducted with blinding of patients or follow-up health personnel. Most studies are retrospective or low-quality case series. The method problems involve varying degrees of preoperative assessment, lack of comparison and no randomisation of the treatments, different radiological assessment and follow-up, varying follow-up time and different preoperative and follow-up parameters. It is difficult to produce good review articles and meta-analyses, and there are no Cochrane recommendations.
Assessment of scaphoid fractures
Patients with wrist pain following falls should undergo clinical examination with scaphoid fracture in mind. The clinical examination must include palpation of the «anatomical snuff box» with the wrist ulnar-deviated, so that the whole central portion of the scaphoid can be palpated between the extensor pollicis longus and the abductor pollicis longus/extensor pollicis brevis. The volar scaphoid tubercle is also palpated, and the thumb compressed in the longitudinal direction of the scaphoid (Fig. 1). The tests have high sensitivity (100 % when all three tests are positive (8)) and accordingly high negative predictive value. The positive predictive value is lower (58 %). A positive test must therefore lead to further tests (8, 9).
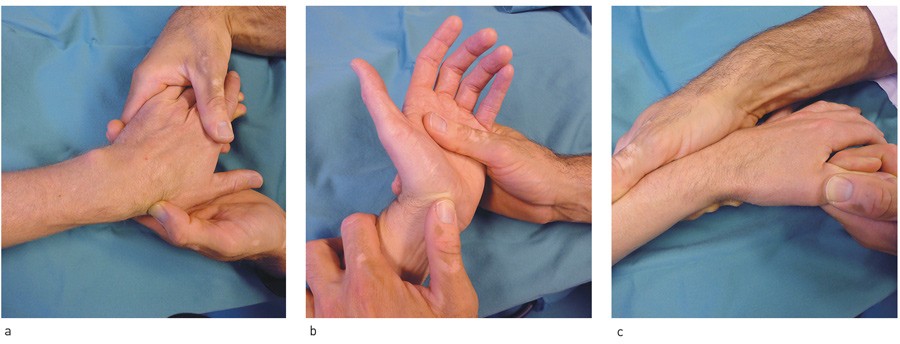
Figure 1 Clinical examination of suspected scaphoid fracture. a) Palpation of scaphoid in the «snuff box» with ulnar-deviated wrist, b) compression of scaphoid tubercle, c) longitudinal compression of scaphoid along the thumb
The four standard radiological projections (Fig. 2) detect the majority of fractures, but some fractures are not visible in the initial pictures. Patients with positive clinical findings and negative X-ray findings must therefore undergo further testing. The situation can either be resolved immediately with MRI/CT or the patients can be cast immobilised and undergo clinical and X-ray tests after two weeks. If there is still clinical suspicion but negative X-rays, a CT or MRI scan must be taken to confirm or discount a fracture (Fig. 3). MRI and CT are both 100 % sensitive. CT is better at revealing dislocation and signs of an older fracture or pseudarthrosis (10). If possible, the situation should be clarified immediately with supplementary diagnostic imaging, to spare the patient unnecessary immobilisation. See the flow chart for evaluation of suspected scaphoid fractures (Fig. 4).
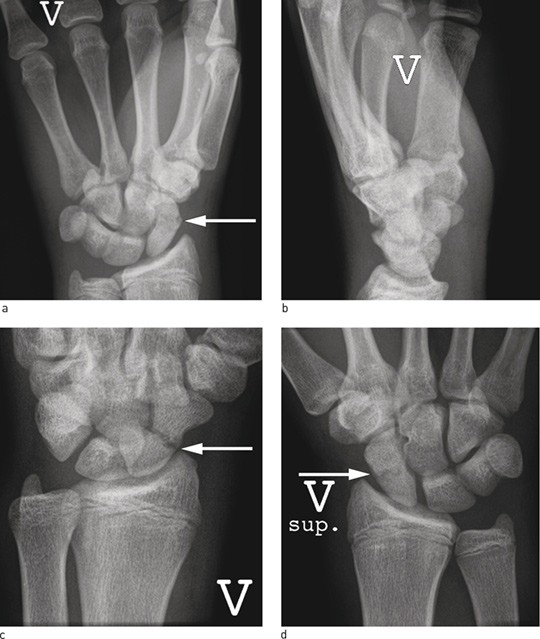
Figure 2 Standard X-ray projections on suspicion of scaphoid fracture, arrow where the fracture is visible. a) Frontal projection, b) lateral projection (difficult to identify fracture), c) oblique projection, d) supine projection
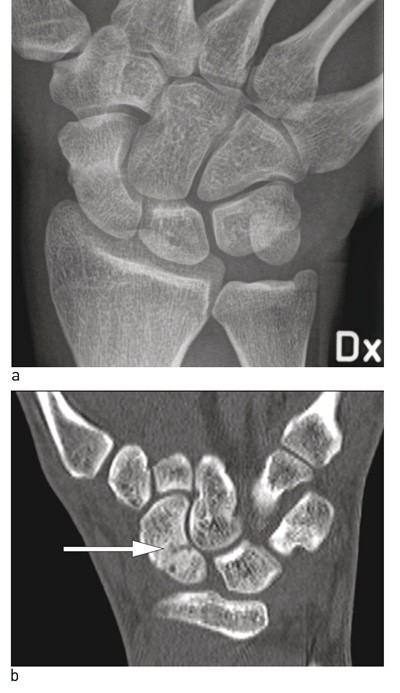
Figure 3 Acute scaphoid fracture, not visible on standard X-ray images. a) Frontal projection, overview picture (difficult to see fracture lines in scaphoid, b) CT we see fracture line, marked with arrow
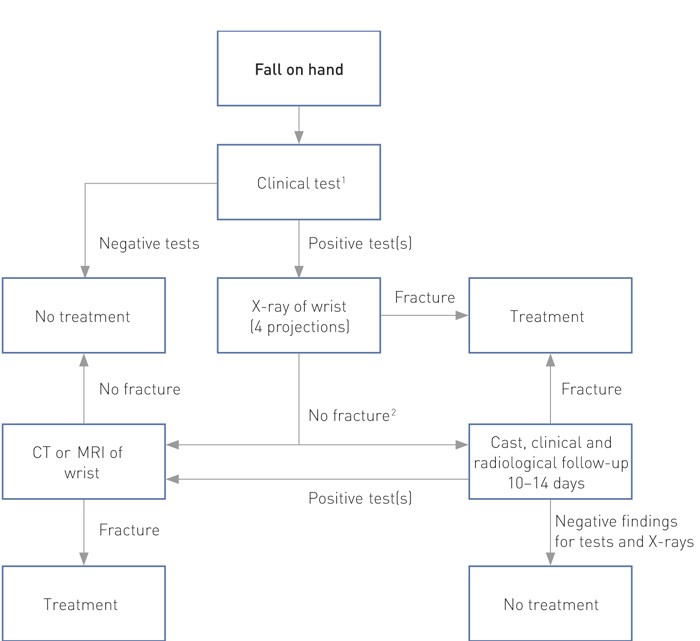
Figure 4 Proposed assessment of suspected scaphoid fracture
¹ Clinical tests consist of palpation of the anatomical snuff box, palpation of scaphoid turbercle and longitudinal compression along the thumb.
² Immediate CT/MRI is preferable to cast immobilisation if possible in practice
Treatment of fresh scaphoid fractures
Most retrospective follow-up studies show a high healing frequency (89 – 100 %) and good wrist function both after immobilisation and after surgery (4, 11, 12). Immobilisation must start early. A delay of four weeks results in a dramatic increase in the frequency of pseudarthrosis and delayed union (> 80 %) (13).
Different cast types (with or without the thumb immobilised, slightly flexed or extended wrist, below or above the elbow) were compared in three randomised, controlled studies (14 – 16) without a difference in the rate of union (89 – 96 %) or wrist function. In six randomised, controlled studies without blinding, 8 – 12 weeks’ cast immobilisation was compared with screw fixation (17 – 22). The fracture was regarded as united if bone trabeculae bridged the fracture line of the four named projections. In cases of doubt, the healing was determined with CT. Surgery resulted in somewhat better wrist function after three months, but not after 6 – 12 months. Both groups achieved excellent wrist function, but those who underwent surgery developed more arthrosis in the trapezium-scaphoid joint where the screw was introduced. With the exception of one study, which also included displaced and comminuted fractures (23), no significant differences were found in the rate of union (87 – 100 %). Several meta-analyses and review articles have been based on the literature, including the few existing prospective studies. Three meta-studies found no difference in the rate of union. One study found a slightly increased relative risk of pseudarthrosis in connection with cast immobilisation, but not when account was taken of patient dropout during follow-up. The complication frequency is significantly higher for surgery, but most complications are mild and transient (24 – 27). There is consensus that displaced fractures and fractures that are parts of wrist fracture displacements should have internal fixation (28, 29). If displacement is seen on X-rays, the fracture should be evaluated with a CT scan and considered for surgery. In such cases, casts do not provide enough stability for healing. The safest is to immobilise all patients with casts for 12 weeks before running an X-ray check.
Treatment of scaphoid pseudarthrosis
A scaphoid fracture that shows no signs of union after 3 – 4 months in plaster will not heal with further conservative treatment, and should be referred for surgery (13). A review of 270 scaphoid pseudarthrosis cases showed that almost half the patients did not go to a doctor when they were injured. Only 53 of the 270 were diagnosed as having an acute scaphoid fracture, while 93 fractures were overlooked by the doctor. X-ray pictures were taken in 60 of these cases. Only 30 scaphoid fractures were cast immobilised and treatment carried out according to plan, but seven of these fractures were displaced and should have been operated upon in the first instance (3). Forty-seven of the 270 patients received were unnecessarily immobilised for 2 – 4 months after they were diagnosed with manifest pseudarthrosis.
Pseudarthrosis with incongruence and displacement causes arthrosis, which starts radially with ulnar and mid-carpal progression. Arthrosis is seen in the majority of patients in the course of 5 – 10 years (30 – 32). With advanced arthrosis involving considerable pain and mobility loss, there is no point in operating upon the pseudarthrosis. Depending on the pain, extent of the arthrosis and functional requirements, these patients should be offered a wrist prosthesis, or alternatively partial/total wrist arthrodesis (33 – 35).
It is generally agreed that scaphoid pseudarthrosis in the middle and distal part without arthrotic changes should be treated surgically with an avascular bone graft from the crista iliaca or distal radius, internal fixation with metal pins or screws (Fig. 5). The surest is to have a cast for 12 weeks post-operatively. The rate of union is 85 – 95 %, patients report little pain and achieve excellent wrist function, but accompanying arthrosis results in reduced function (36 – 38). A lower rate of union has been described for outdated methods, where only bone grafts are used without simultaneous internal fixation (39). Two prospective randomised studies have been conducted of scaphoid pseudarthroses where pedicled vascularised radius bone grafting was compared with non-vascularised crista and radius grafting. The patients in the first study had plaster casts for four weeks, and the healing frequency for avascular bone grafts (73 %) was lower than for vascular bone grafts (89 %), but also lower than in most retrospective studies where patients spent 8 – 12 weeks in casts. The study has not led to a change in the choice of bone graft in connection with pseudarthrosis treatment (40). In the second study, union rates were similar, and the gain offered by vascularised bone grafting was too small to justify the more resource-intensive and technically demanding procedure (41).
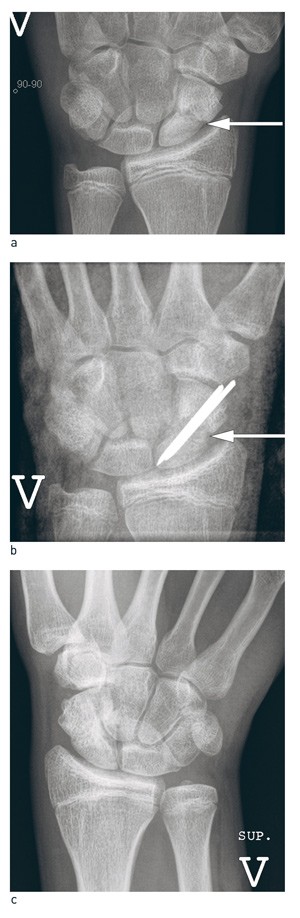
Figure 5 Treatment of scaphoid pseudarthrosis. a) 18-month old scaphoid pseudarthrosis (white arrow) in young man, b) Operated with bone graft from crista and 1.6 mm smooth metal pins. Post-operative picture with cast, arrow on bone graft, c) Final check-up after 14 months. Normal wrist function, no secondary wrist arthrosis, bone graft incorporated in scaphoid
There is lack of consensus regarding treatment of the most proximal scaphoid pseudarthroses. Reduced blood circulation, a limited contact surface between the fragments, small fragments that provide little grip for fixation, and strong forces acting over the pseudarthrosis gap, can reduce union. Standard pseudarthrosis surgery as described above is used by many, while some prefer technically demanding vascularised bone grafts from the distal radius. The results vary, and there is no evidence that one method is superior to others. Lack of consensus on the definition of non-vascularisation of the scaphoid (sclerotic proximal fragment on the x-ray, non-vascularised fragment seen on the MRI with contrast, the surgeons’ intraoperative assessment of vascularisation in the fragment) makes it difficult to compare the patient series and the results (37, 42 – 44). The most proximal scaphoid pseudarthroses account for a very small percentage of patients. In our view, these should be referred to specialist hand surgery departments.
Discussion
Assessment and treatment of scaphoid fractures in Norway as reported in 2006 (7) are consistent with internationally documented good practice. Faster rehabilitation and the possibility of earlier wrist activity are the benefits of performing scaphoid surgery in the acute phase. This must be balanced against the risk of complications. The patients in the published studies have been operated upon by dedicated hand surgeons with long experience, so that the results and frequency of complications must be assumed to represent the very best that can be achieved.
The Norwegian approach with cast immobilisation from the lower arm to the interphalangeal joint of the thumb as first choice and offer of surgery to patients who need earlier mobilisation and who accept the risk of surgical complications, is prudent in the absence of larger and better studies to differentiate treatment. With surgery, the fracture is fixed with a screw (stable fixation) to avoid the need for cast immobilisation. Screws can be difficult to place correctly, which is crucial in an area with cartilage surfaces on all sides. The patients should be operated upon by surgeons with experience of procedures on scaphoid/wrist bones. Cast immobilisation alone should be the standard treatment for non-displaced, fresh scaphoid fractures, regardless of where they might be located.
Scaphoid pseudarthrosis is distinguished from acute fractures through the history of the injury (time elapsed since the injury) and radiological findings (resorption in fracture crack, sclerotic fracture ends, cysts and increasing displacement. These do not unite with cast immobilisation. It is worth scrutinising X-ray images and history of illness to pick out older injuries. Long-term outcomes following successful pseudarthrosis surgery are good, given early diagnosis and normal joint surfaces. Re-operation and secondary arthrotic changes result in a less favourable clinical outcome (38, 42). If the secondary arthrosis is sufficiently painful and includes the radioscaphoid joint facet or major parts of the joint, the patient can be offered partial arthrodesis of the wrist (four-bone arthrodesis), a wrist prosthesis or total arthrodesis.
