A woman experienced exacerbation of headache that had started several months earlier. She was subsequently hospitalised after developing unusual cognitive symptoms.
The patient, who was in her forties, had a history of asthma and previous gastric bypass surgery. In the six months prior to hospitalisation, she had been on sick leave owing to occipital, bilateral headache which arose during a labour dispute, but which persisted despite her transfer to a new position. The headache had a fluctuating course, with headache-free days.
The month before she was hospitalised, however, the headache had become constant, and she had been taking paracetamol daily and sumatriptan and diclofenac frequently. Her general practitioner had recommended diagnostic imaging but the patient did not consider this necessary, attributing the headache to muscular tension caused by stress.
Headache is a common reason for GP consultations and can be a diagnostic challenge. The International Classification of Headache Disorders lists over 200 different types of primary and secondary headache (1). Primary headache with no other underlying cause can be difficult to distinguish clinically from headache that is secondary to another condition. Particular attention should therefore be paid during the history taking and examination to «red flags» that suggest secondary headache.
Key warning signs are summarised in the acronym «SNARET» in Norwegian (2), which is derived from the English-language acronym «SNOOP» (Table 1) (3). The patient’s headache had changed from episodic to constant, but this was the only «red flag» that was identified according to «SNARET». It is worth noting that the patient used analgesics on a daily basis, so complicating medication-overuse headache should also be suspected.
|
Table 1 Warning signs for headache summarised via the acronym «SNOOP» (3)
|
|
Systemic symptoms/signs/disease (fever, myalgias, weight loss, malignancy, AIDS)
|
|
Neurological symptoms or signs
|
|
Onset sudden (thunderclap headache)
|
|
Onset after age 40 years1
|
|
Pattern change (progressive headache with loss of headache-free periods or change in type of headache)
|
|
[i]
|
The day before admission, the headache had changed again. The pain was now right-sided and most intense around the ear, and radiated to the cheek and jaw. When her partner came home from work the next day, he found her to be confused. She was unable to tell the time, and did not understand the content of text messages. They attended the accident and emergency department, where she failed to recognise the building although she worked there on a daily basis.
Her own face, and that of her partner, had become unrecognisable to her. She explained that she knew perfectly well who her partner was, but that his face appeared completely alien. While watching TV in the waiting room, she had been unable to recognise any of the faces from the series «The Bridge», but could nevertheless identify the characters by their clothes. She had asked her partner why all of the actors had been replaced.
Somatic status and blood tests provided no evidence to suggest an internal medical condition. The patient was considered to be confused and was referred to the emergency ward for neurological assessment with respect to possible transient global amnesia (TGA).
A presentation including headache that has changed in character and an acute confusional state suggests a serious secondary aetiology. Relevant differential diagnoses in this context include infections, cerebrovascular disorders and expansive processes.
In the emergency ward, the patient was distressed and anxious. She could recount her own medical history, was oriented to place and time, and remembered her national identity number and the name of the prime minister. Her vital signs were normal – blood pressure 144/75 mm Hg, heart rate 60/min, oxygen saturation 97 % in room air and temperature 37.0 °C measured with a forehead thermometer. Somatic status was normal, and there was no stiffness of the neck.
Neurological status was also normal, including ophthalmoscopy and a Donders’ visual field test, and she showed preserved visual recognition of objects such as a pen, and tactile recognition of digits traced on the palm of her hand. Blood tests were within normal ranges, including D-dimer of 0.3 mg/l (0.0 – 0.5 mg/l).
The patient was oriented and non-amnesic, thus there were no grounds to suspect a confusional state or amnestic syndrome. Infection was considered unlikely in the absence of fever or neck stiffness.
Her medical history, with prolonged, slowly progressive headache, was not typical of subarachnoid haemorrhage. Other cerebrovascular disorders and a cerebral tumour remained plausible differential diagnoses.
Cerebral CT yielded no definitive findings, but raised suspicion of intracranial venous pathology. T1-weighted MRI of the posterior cranial fossa after contrast injection revealed a thrombus in the right transverse sinus (Fig. 1), but no obstruction on the left side.
Treatment with low molecular weight heparin in the form of enoxaparin 1 mg/kg × 2 was initiated. The day after admission the patient showed complete remission of cognitive symptoms, and was in good health upon discharge.
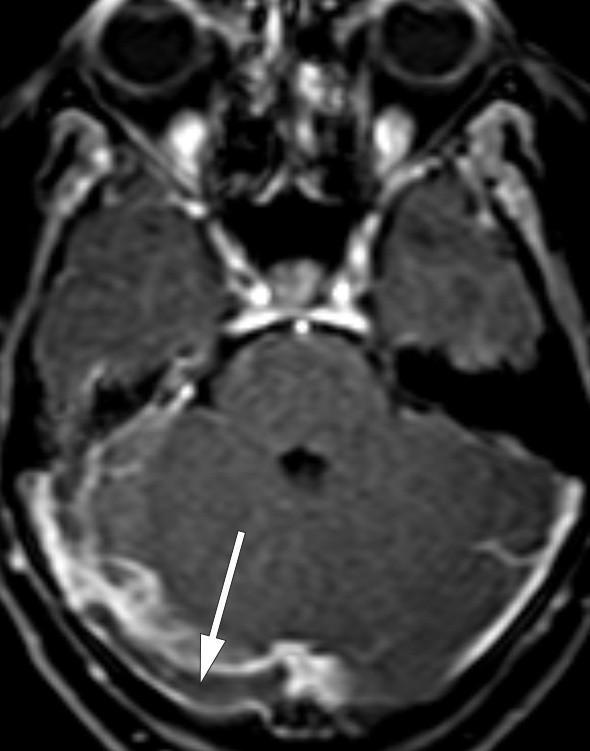
Figure 1 Thrombus in right transverse sinus (arrow) on T1-weighted MRI after contrast injection
Discussion
This case history is an example of the extensive variation that can be seen in the presentation of cerebral venous thrombosis (CVT). This condition encompasses thrombosis in cerebral veins and dural sinuses, and in the latter case it is often referred to as cerebral venous sinus thrombosis.
CVT is rare but probably underdiagnosed, with an estimated incidence of less than 1 in 100 000 population per year. Less than 1 % of all cases of stroke are due to CVT complicated by haemorrhagic infarction (4). Pathophysiological mechanisms in all venous thrombus formation can be explained on the basis of Virchow’s triad: factors relating to the vascular endothelium, haemodynamics and/or coagulability of the blood itself (5). Key risk factors for thrombosis are infections, congenital thrombophilia, and hypercoagulopathy as seen in conditions such as malignancy and systemic rheumatic diseases. In the general population, venous thrombosis occurs most frequently in persons under the age of 40 and is more common in women than in men, probably due to oestrogen-containing oral contraceptives and pregnancy (4).
Our patient did not have congenital thrombophilia, and screening with chest X-ray, mammography and gynaecological examination raised no suspicion of malignancy (6). The patient was using the hormonal coil intrauterine system (non-oestrogen-based), in addition to daily adrenergic and corticosteroid inhalers (salmeterol-fluticasone) and prednisolone cures to treat asthma exacerbations.
A Danish registry-based case-control study described a dose-dependent increase in the risk of venous thromboembolism in the lower extremities and lungs following glucocorticoid therapy (7). The risk was greatest with systemic use but was also found to be increased with other routes of administration, including inhalation. Patients with venous thrombosis in other locations were not included in the study, but glucocorticoid use has been listed elsewhere as a risk factor for CVT (8). Thus, a possible connection between our patient’s steroid use and CVT cannot be ruled out.
D-dimer has a diagnostic sensitivity of 94 % and specificity of 90 % for CVT. Our patient had a false-negative D-dimer test. False negative D-dimer is most often seen in association with isolated headache, prolonged symptoms and limited sinus involvement (9). Imaging is therefore recommended upon clinical suspicion of CVT, with cerebral MRI with venous angiography as the gold standard (4).
The most frequently reported symptom of CVT is headache, which is present in up to 90 % of cases and in 9 % is the only symptom. More than half of patients have a subacute onset with headache that increases in inensity over a few days. One third of cases have an acute onset over the course of 24 hours, whereas only a minority have a chronic course. In addition to headache, elevated intracranial pressure may cause vomiting, papilloedema and visual disturbances. CVT may also cause a focal syndrome, with focal neurological deficits and seizures, or an encephalopathy syndrome, with bilateral or multifocal signs and possible disturbances of consciousness (8).
Our patient had clear cognitive symptoms that suggested involvement of one particular area of the brain. The most striking finding was her inability to recognise faces and familiar surroundings. Deficits in the brain’s ability to interpret visual stimuli can be divided into those that reflect disruption to the association fibres projecting from the occipital lobe to the parietal lobe («where» pathway deficits) and those that reflect disruption to the association fibres projecting to the temporal lobe («what» pathway deficits) (Fig. 2) (10, 11). The visual agnosias belong to the latter group. They are usually defined as an inability to recognise objects that is not due to sensory impairment or general intellectual impairment (i.e., «what» pathway deficits).
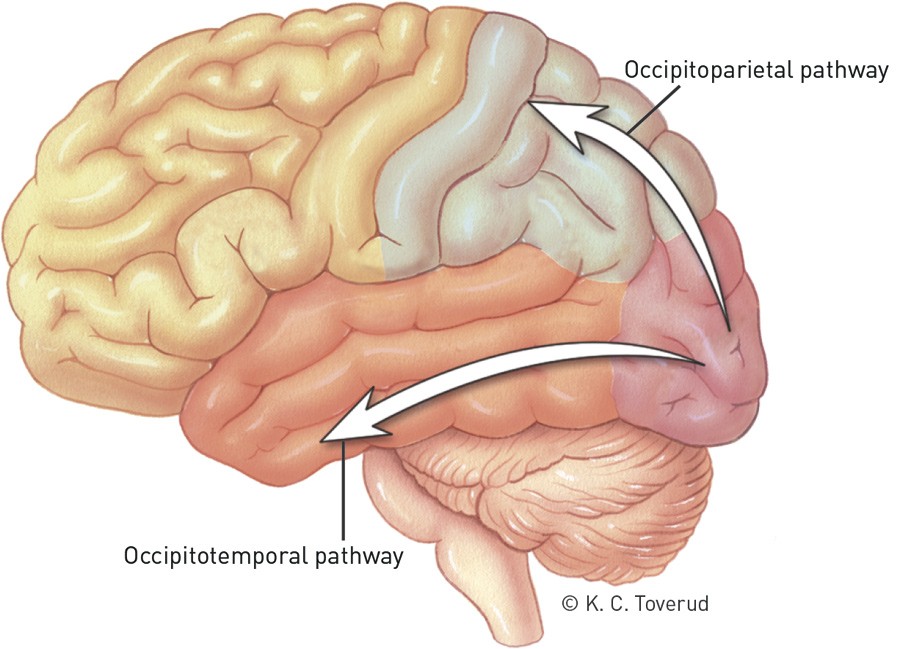
Figure 2 According to the two-streams hypothesis, the final visual image is the result of processing in two pathways. The association fibres of the occipital lobe project via these pathways to the parietal lobe (arrow) and temporal lobe (arrow). The deficits in our patient suggested disruption of the occipitotemporal pathway
Prosopagnosia (from the Greek «prosopon» for face and «gnosis» for knowledge) is a specific visual agnosia in which affected individuals are unable to recognise a familiar face from looking at the person or an image, even though they correctly identify the object as a face and can point out distinguishing features such as glasses, facial hair or voice (12). The neurologist and author Oliver Sacks described a patient with prosopagnosia in his essay «The man who mistook his wife for a hat». While visiting the patient at home, Sacks commented on the pictures of different people hanging on the wall: «By and large, he recognised nobody: neither his family, nor his colleagues, nor his pupils, nor himself. He recognised a portrait of Einstein because he picked up the characteristic hair and moustache.» (13).
A small number of cases that have been examined anatomically and with CT or MRI scans indicate that prosopagnosia is usually associated with bilateral medial occipitotemporal lesions. There are also rare cases caused by unilateral injury, almost always on the right side (14). Our patient’s thrombus was in fact in the right transverse sinus (Fig. 1). Venous drainage from the temporal lobe into the transverse sinus occurs via the vein of Labbé (inferior anastomotic vein), and venous stasis here can cause circulatory disturbances in associated brain tissue. MRI revealed no diffusion abnormalities or other parenchymal changes. However, no signal was detected in the vein of Labbé on the side in question, whereas a good signal was obtained in the contralateral vein (Fig. 3). On balance, we consider it likely that the MRI findings are related to the patient’s cognitive symptoms.
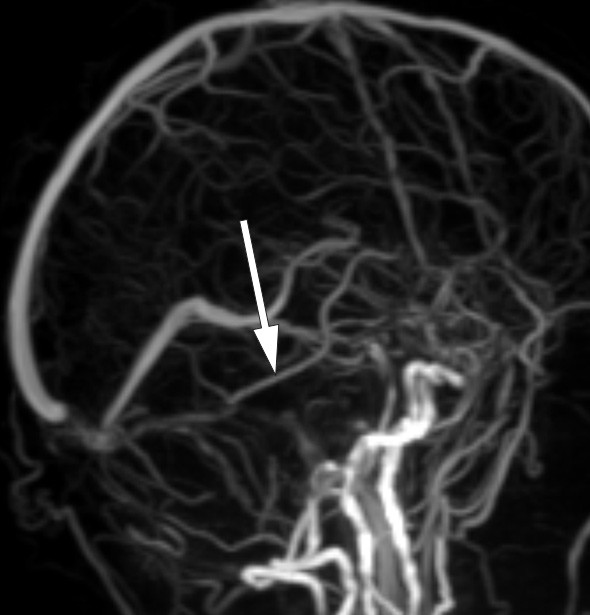
Figure 3 Venous MR angiogram (TOF sequence) shows good filling of the contralateral vein of Labbé (arrow), but no signal in the ipsilateral vein
Human studies using techniques such as functional MRI (fMRI) have provided strong evidence for the existence of a small area within the fusiform gyrus of the temporal lobe where most of the neurons are face-specific (Fig. 4) (15). The idea of a «face area» in the fusiform gyrus is an oversimplification, but one which is conveyed uncritically in popular culture and which turned up in the James Bond film «Spectre» during the patient’s convalescence. In a scene in which Bond is strapped to a chair loaded with sophisticated drilling equipment, the arch villain threatens to drill into Bond’s fusiform gyrus and thus destroy his ability to recognise faces. As well as further cementing the aforementioned oversimplification, an even graver offence, neuroanatomically speaking, is that the drill was pointed too low and was aimed at the mastoid process and not the fusiform gyrus. The Bond villain was subjected to a neurosurgical reprimand in Nature (16).
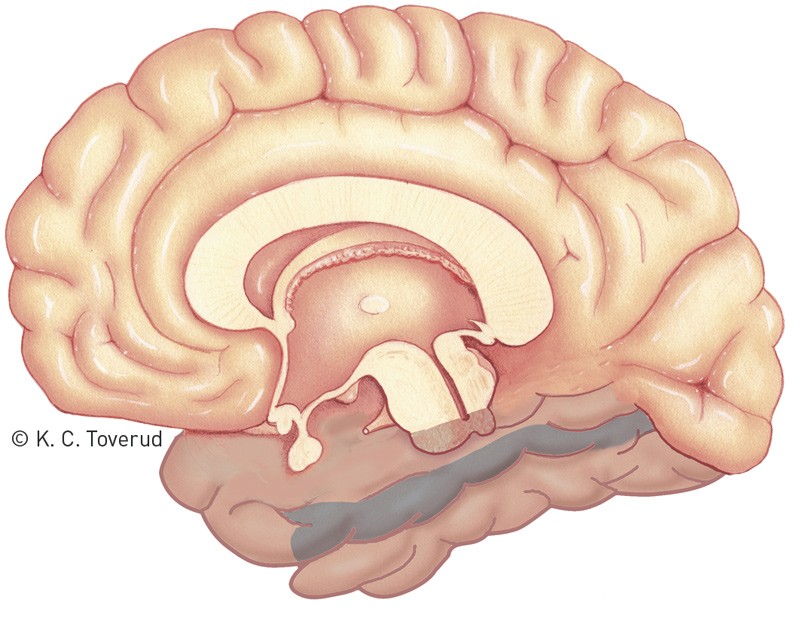
Figure 4 Medial view of the right hemisphere, with the fusiform gyrus of the temporal lobe marked in blue. Functional MRI studies have implicated an area within the fusiform gyrus in face recognition, often referred to as the «fusiform face area» (FFA) (not marked on figure)
In addition to prosopagnosia, our patient also had difficulty recognising familiar places, so-called environmental agnosia. This symptom is closely linked to and often associated with prosopagnosia. As in prosopagnosia, it is the occipitotemporal connections that are affected, typically on the right side, although some patients have bilateral lesions. The patient can describe a place from memory or locate it on a map, but will fail to recognise the place once there and will lose their way. They thus have problems with the «what» aspect of their surroundings, but not the «where» (17). Our patient had no difficulty intellectually in understanding that she was inside the building that contained her office, but she experienced no feeling of recognition.
At a check-up a month later the patient had no symptoms other than occasional episodes of low-grade headache. As the association between steroid use and the CVT was uncertain, we considered the condition to be idiopathic and, in line with recommended practice, initiated 12 months of anticoagulation therapy with warfarin (18).
This case report illustrates an unusual clinical presentation of CVT, marked by curious cognitive symptoms that have also found their way into popular culture. As far as we are aware, this is the first report of prosopagnosia as a symptom of CVT.