Today there are Regional Committees for Medical and Health Research Ethics in every regional health authority. Their work is based on several laws, including the Health Research Act, the Personal Data Act and the Patients’ Rights Act (1), in addition to international guidelines on health research, like the Declaration of Helsinki (2).
The Committees preapprove research projects involving human subjects and human biological data, and projects that use health data that has been collected through clinical practice or research (3). In their work, the Committees assess the risk that research subjects are exposed to, whether the requirements regarding information and consent have been met, and whether the scientific quality and benefit justify the intervention in the lives of the research subjects (4).
The first Norwegian Regional Committees for Medical and Health Research Ethics were established in 1985. The process of structuring the Committees, and their early work, has been described previously (5). However, this process was a result of events that took place even earlier. This article will look at two such events, and show the role they played in the subsequent creation of the Committees: the revision of the Declaration of Helsinki in 1975, with a clear call for the use of research ethics committees, and the media coverage of the Gro case in 1974, which forced research ethics into the public discourse.
Material and method
In our work on this article, we have attempted to survey existing literature in the form of books and articles about the history of research ethics from the University Library at the University of Oslo and the National Library of Norway, the History of Science, Technology and Medicine database and old newspapers, by searching Retriever. We have also manually reviewed issues of the Norwegian newspaper Dagbladet from 1974 and relevant years of the Journal of the Norwegian Medical Association. Finally, the Norwegian Association of Higher Education Institutions and the Faculty of Social Sciences at the University of Oslo helped us search for material in their archives.
Research ethics in the wake of World War II
Medical research ethics was forced into the spotlight following the 1947 Doctors’ Trial in Nuremberg, which uncovered extensive medical experimentation on prisoners in concentration camps during World War II. The experiments were considered unquestionably ethically indefensible, based on their nature and the fact that they were conducted under direct or indirect duress.
One of the consequences of the trial was the Nuremberg Code, an appendix to the judgment, which was a set of research ethics principles for human experimentation (6, 7). A key component of the Code was informed consent. It stated that human experimentation must not be conducted on people who cannot or will not grant voluntary informed consent – regardless of the reason.
In 1964, the World Medical Association adopted the Declaration of Helsinki, which specifically provides ethics principles for medical research. It is generally accepted that the Nuremberg Code provided a foundation for the work on the Declaration (8). However, the Declaration differed substantially from the Nuremberg Code; it was written by doctors who planned to regulate their own activities, not an independent legal body, and the doctors had a different view of research ethics than the Nuremberg judges.
The Declaration consisted of general ethical guidelines for research, divided into clinical therapeutic research and non-therapeutic research. Informed consent was also a key component of the Declaration of Helsinki. The latter allowed consent to be obtained from the research subjects’ parents or guardians for clinical therapeutic research if the subjects were unable to grant consent themselves, unlike the Nuremberg Code. In other words, it was possible to circumvent the principle of informed consent if the research subject was deemed mentally or physically not competent, and the experiment was expected to be of great benefit. For non-therapeutic research, however, the subjects were required to have the mental, physical and legal ability to make their own independent decision (9).
The World Medical Association adopted the Declaration of Helsinki unanimously in 1964, following a decade of discussions and several revisions (8).
There were reports of unethical research in both the USA and the United Kingdom in the years following the Declaration of Helsinki. Renowned US doctor and researcher Henry Beecher published an article in the New England Journal of Medicine in 1966 (10), and British doctor Maurice Pappworth published his book the next year (11). They both mentioned concurrent cases of unethical research.
Beecher stated that «Nearly everyone agrees that ethics violations do occur. The practical question is, how often?». Both authors commented that only a few of the research articles discussed the extent to which informed consent had been obtained. Beecher examined the concept of «informed consent», and believed that it was difficult to obtain it in practice, but nonetheless asserted that it should always be sought, for sociological, ethical and legal reasons: «There is no choice in the matter» (10, p. 1355). Pappworth also argued in favour of research ethics committees at hospitals.
Both of these texts provided the foundation for a broader discussion among the authors’ colleagues. Many people took a defensive stance and claimed that the two authors were wrong, that such incidents did not occur, and that this critique should not take place in the public arena (12). The medical profession preferred not to air its dirty laundry in public.
Despite this, research ethics was gradually institutionalised in several Western countries during this period. In the USA, ethical peer review was introduced in the early 1950s. From 1966, all research projects involving experiments on human subjects were required to be presented to a research ethics committee (13, 14). In order to receive funding from the U.S. Public Health Service, research projects had to undergo an external assessment of the researcher’s ethical judgement before the projects could begin. The intention of the assessment was to review the rights of research subjects and the methods used to obtain informed consent. The assessment would weigh the risks and possible benefits associated with the project (13).
As several British research communities also received funding from the U.S. Public Health Service, this requirement, in conjunction with the discussion initiated by Pappworth, played an important role in the establishment of permanent research ethics committees in the United Kingdom in 1972 (13). Sweden had had institutional research ethics committees since 1966 (5).
In Norway, it became necessary to establish ad hoc committees whenever this was required by commissioners of research or for publication in international journals (15). Despite the scientific debate and the institutionalisation of research ethics in other countries, Norway did not appear to be in a hurry to establish permanent committees. A further two factors played a critical role here in Norway: a recommendation in the revised Declaration of Helsinki to establish research ethics committees in all countries, and external pressure in the form of the so-called Gro case.
Revision of the Declaration of Helsinki
The decades following World War II saw tremendous growth in the amount of research (16 – 21). The medical knowledge base increased enormously, leading to better, more effective diagnostic tools and treatment, both in terms of drugs and surgery. There was an explosion in new treatment methods, like antibiotics, antihypertensive drugs, antipsychotic drugs and organ transplants.
Medical treatment became a commercial goldmine, and the pharmaceutical industry grew massively (21). There was a corresponding increase in the need for documentation of the efficacy and safety of new treatment methods. At the same time, new challenges arose, and they were summarised thus by Peter F. Hjort in 1967: «At the beginning of the century, young people died, and they died from tuberculosis and other infections; today it is old people who die, and they die from cardiovascular disease and cancer» (18 p. 1664).
This was part of the backdrop for the World Medical Association’s decision to revise the Declaration of Helsinki in 1975 – about ten years after it was adopted. A Scandinavian working group was tasked with revising it by their respective country’s medical association. The group consisted of Dane Povl Riis (born in 1925), Swede Clarence Blomqvist (1925 – 1979) and Norwegian Erik Enger (1927 – 2016) (22, 23).
Riis later wrote that the Nordic region was unfamiliar with the original Declaration, which explains why it had not been fully implemented (22, 24). The gradual transition from small therapeutic experiments to a new gold standard for medical research – clinical trials using control groups – also made the original Declaration of Helsinki less relevant to researchers’ everyday work as it became better known (14 – 16, 22, 24). Enger considered the unconditional requirement of consent in the original Declaration to be problematic. Like others, he believed that consent should be subject to discretion in certain cases (16, 19, 25).
The Declaration of Helsinki was considerably expanded and reworked in the 1975 revision (6). The new version replaced the term «clinical research» with «biomedical research» in order to cover other types of research on humans or human material. It allowed research on etiology and pathogenesis, in addition to therapy alone. The new Declaration also explicitly mentioned the use of control groups. Journals were advised against publishing the results of research that did not comply with the principles in the Declaration.
The largest and most striking change in the 1975 Declaration of Helsinki can be found in part I, points 2 and 12 (6, 23, 26). These points plainly stated that experiments must be clearly described in a research protocol to be submitted «for consideration, comment, guidance and approval to the concerned research ethics committee». The protocol was to contain a discussion of ethical matters and confirmation that the principles in the Declaration had been met.
The revision made it possible to omit to obtain consent if information about the research would have a negative impact on the patient. However, the research protocol needed to discuss and explain this in great detail, and then be approved by a research ethics committee. The requirement of informed consent thus became less and less absolute – going from the unequivocal directive in the Nuremberg Code through the Declaration of Helsinki’s option to obtain the consent of the parent or guardian to the opportunity in the revised Declaration to fully omit to obtain consent, with a good justification and approval from an independent committee.
The new demand for research ethics committees emerged as the research ethics guidelines placed persistently less value on the subject’s consent. There was a need for greater room to exercise discretion in ethical assessments, while avoiding the sole discretion of the researcher.
The revised Declaration of Helsinki did not say anything about how to organise the committees or who would sit on them. According to Erik Enger (23), the General Assembly where the revision was adopted agreed that the World Medical Association would recommend the establishment of such committees, but that the details surrounding their organisation should be up to each country. He also commented that the revision «means that it is now time, also in our country, to discuss the matter of establishing such committees and to address the question of their function» (23). The Norwegian Medical Association adopted the Declaration (23), and it remained in place with only minor changes until the next comprehensive revision in 2000 (6).
The Gro case – Torture in Norwegian science
From the end of the 1960s and into the 1970s, the public became increasingly sceptical towards «experts» and no longer had blind faith in trained professionals like doctors and researchers having a reliable moral compass (27, 28). The media gained a more active role in the debate on research and treatment, and doctors were urged to be more aware of how they presented themselves, in order to avoid «sensationalised information to the press» (29).
In the winter of 1974, Dagbladet focused on «the place of science in the society in which we live» (30) (fig. 1). As part of this debate, the newspaper conducted a focused campaign against unethical research, with journalists Arne Skouen and Gerd Benneche leading the way. On 19 February, the first revelation was made in what was later called the Gro case: Skouen’s article Tortur i norsk vitenskap (Torture in Norwegian science) (31). In the article, Skouen made reference to a research report published in the journal Nordisk psykologi (32), which introduced «Gro».
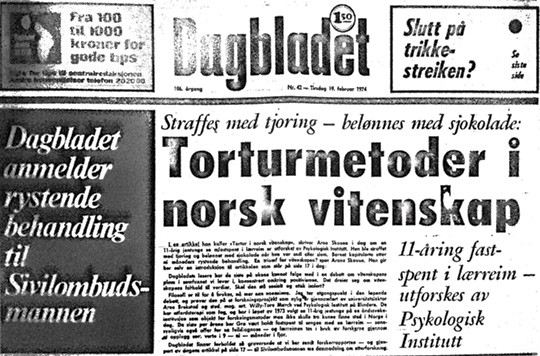
Figure 1 Cover of Dagbladet, 19 February 1974
Gro had lived in an institution from the age of five (fig. 2) (33). Upon admission, she was diagnosed with «oligophrenia, retardatio mentalis», which Skouen translated as «intelligence defect with associated mental retardation». Researchers Arne Brekstad and Willy-Tore Mørch met Gro when she was eleven. At that point, she had been restrained with leather straps for two years around the clock, except for when she was being cleaned.

Figure 2 Solbakken at the Klæbu nursing home, the institution where Gro lived. Photo: Ingar Johansen, Adresseavisen, 1983. Reproduced with the permission of the Klæbu historical association (33)
In the article, Skouen described how the researchers used the 11-year-old’s situation as a starting-point for experimenting with behavioural therapy – giving her a reward if she behaved the way they wanted her to and punishing her if she did not. He concluded by writing that Dagbladet had written to the Parliamentary Ombudsman, asking it to «open an investigation into the Gro case».
In the article, Skouen argued strongly against the researchers’ attitudes and lack of reflection on Gro’s situation. The research article did not contain any ethical or legal discussions regarding the extent to which they had obtained consent – from Gro or her parents or guardians – or the extent to which the researchers’ methods could otherwise be defended from an ethical perspective: «Scientific philosophy and responsibility is not their area of expertise». And further: «When they describe the nine-month period of torture, they leave us as social individuals».
Skouen’s article led to a major debate in Dagbladet over the following few days. Experts from different fields discussed the case, including lawyers, educators, psychiatrists and politicians. The case was also discussed on national broadcaster NRK’s programme Kveldsforum.
The Directorate of Health began looking into the case a few days after the first revelations (34 – 38). Willy-Tore Mørch was also given an opportunity to respond to the accusations (39). He was a student at the Department of Psychology at the University of Oslo while he shared responsibility for the research project, but he pointed out that the Department had not been informed about the project. According to Mørch, the fact that the Department’s name was written under the author’s name in the research report was only a formality, because Brekstad worked there.
The same issue contained a letter from Department Head Leif J. Braaten at the Department of Psychology (40). He pointed out that it was common practice at the Department that «scientific experiments are facilitated and conducted by one or more people from our academic staff, without the main bodies of the department generally being involved (the board and council). In general, each researcher has a scientific and ethical responsibility for his/her work. What the department takes responsibility for is each researcher being employed on the basis of an assessment of his academic and educational qualifications».
If we follow these arguments, it was possible for a researcher to practically do whatever they wanted, as long as there was scientific justification for it, without their Department being held responsible. For its part, the Department could claim that it had no knowledge of projects carried out by its employees. The Department’s management had done its job in terms of ensuring ethical compliance when it employed researchers that it believed met its scientific and educational standards. The rest was up to the researcher.
The repercussions of the Gro case
The Gro case provided a foundation for a broader discussion on the organisation of research in Norway. In 1977, Gerd Benneche published a book based on the case (41). She pointed out the lack of accountability that came to light in the Gro case, where a student under the supervision of an employee could run a research programme without the knowledge of the Department. It thus became difficult to determine who was responsible for assuring the ethical aspects of the work.
The Department of Psychology drew up ethical guidelines and established an ethics committee in 1975 (42, 43). Research at the department would be based on ethical discussions within the relevant unit, and more widely, if necessary. Benneche mentioned this in her book (41), and believed that it was to some extent a result of the Gro case. She did ask whether this form of organisation was good enough, and made reference to the revised Declaration of Helsinki and Erik Enger’s call in the Journal of the Norwegian Medical Association for the establishment of research ethics committees in Norway. (23).
In 1977, the Norwegian University Rectors’ Conference (later the Council of Universities) established a commission to discuss ethical guidelines and ethics councils (the so-called Andenæs commission) (15). In 1979, the Council for Research in the Social Sciences in the Norwegian General Scientific Research Council presented a report on research ethics and personal data (44). Both of these measures were partly due to the Gro case (15, 44).
The Andenæs commission recommended the establishment of ethics councils to help researchers reach decisions on ethically equivocal matters (45). The councils would have their roots in the research institutions, i.e. the universities. The commission recommended that the ethics councils only review cases of doubt, where researchers believed they needed help to determine whether their projects were ethically sound, and that the councils be able to investigate planned and ongoing research projects on their own initiative. However, the commission did not propose that all projects be submitted to the councils before their implementation, which was contrary to the requirement in the Declaration of Helsinki. The Council of Universities adopted the recommendation in May 1979 (46). That year it asked the Ministry of Church and Education to enact the proposal in the form of regulations (15).
The recommendations of the Andenæs commission, together with the report on research ethics and personal data and several other initiatives, provided the foundation for the establishment of the National Research Ethics Committees and their current form. The studies were quoted and discussed in a report from a subcommittee of the Central Committee for Norwegian Research in 1981 (15). The report is deemed to have played an important part in accelerating the establishment of research ethics committees following a period of little activity (5). It outlined several measures that had been implemented, but not followed up. The requirement in the Declaration of Helsinki regarding research ethics committees was discussed in great detail. The report described the measures that had been implemented at that point to meet this requirement, and the further steps to be taken.
The Gro case was mentioned specifically in an argument that discipline-specific research ethics committees were not enough; there was also a need for an interdisciplinary coordinating council in order to prevent issues related to collegiality. The Gro case was thus part of the argument made in favour of the establishment of research ethics committees by various parties, several years after the revelations in Dagbladet.
Gaining pace
Whistleblowers like Beecher and Pappworth have traditionally received much of the credit for having laid the international groundwork for the establishment of research ethics committees (12, 47). However, one could question how large a role was played by individuals and individual events. A different view is that individual events are merely visible representations of far more gradual bureaucratic processes that are the result of pragmatic considerations – and that the relevant individual events appear to play a key role when social developments have made society receptive to such changes (14). It is possible to argue that both these arguments are true of the Gro case.
The revised Declaration of Helsinki served as a backdrop to the discussions regarding research ethics committees, as a reminder that in Norway the Norwegian Medical Association had undertaken to establish such committees, but it was not enough to start the process. Norway lagged behind other countries here, and for a long time was content with having ad hoc committees and otherwise placing the responsibility for ethics onto each researcher. The closed discussion regarding the requirement in the Declaration of Helsinki for research ethics committees gained pace thanks to a sharp public debate on the moral status of research, which had been made possible by the contemporary general scepticism towards authorities and the establishment. Two discourses, one professional and one public, coalesced into a joint demand for a clearer ethical regulation of research.
