When patients have symptoms stemming from different organ systems, several specialists will often be involved in their treatment. Interdisciplinary thinking may be crucial for early diagnosis and life-saving prophylaxis.
A woman in her late thirties was electively hospitalised on suspicion of a locally advanced carcinoma of the right breast. Her medical history showed that she had had type 1 diabetes mellitus since she was 11 and had been found to have an extra, non-functioning renal system. A couple of years previously, ultrasound and CT throat had been used at a local hospital to examine her for bilateral goitre. The conclusion of these tests was colloid nodular goitre with no suspicion of malignancy. There is no information as to whether cytology tests were carried out. The patient had two children. Several of the patient’s maternal aunts and uncles had died of cancer.
Suspicion of locally advanced carcinoma of the right breast arose following mammography conducted by a private X-ray institute. The patient suffered from breast tenderness and had requested the examination. The examination of breasts and axillae revealed possible malignant changes in the right breast, possible lymph node metastasis in the right axilla and non-specific changes in the left breast. The radiological diagnosis was regarded as certain, and the patient was referred directly for hospitalisation. Biopsies taken in connection with hospitalisation revealed ductal mammary carcinoma in the right breast and lymph node metastasis in the right axilla.
A cytological sample from a radiologically benign-seeming lesion in the left mamma revealed papillary cell groups without atypical signs. No biopsy was taken from this lesion. A further X-ray examination of the thyroid yielded an image consistent with nodular colloid goitre, but cytological samples contained too little material and were non-diagnostic. The patient received pre-operative chemotherapy and lost her hair. It proved difficult to find a wig that was large enough for her head. Seven months after the start of chemotherapy, ablatio of the right breast was performed with subsequent post-operative radiotherapy.
Findings of synchronous tumour-like changes in the breasts and thyroid lobes of young people are unusual. When malignant neoplasms are found in one of these organs, it is important to determine whether tumours found in the second organ represent metastasis or a new primary tumour, because it may have consequences for treatment.
Because of pressure symptoms in the throat and respiratory discomfort, a further radiological examination was made of the thyroid, and cytological samples obtained, but these too failed to provide sufficient material for diagnosis. The patient’s left thyroid lobe was removed the year after she was treated for cancer of the right breast, although there was no preoperative cytological diagnosis. A macroscopic examination of the left thyroid lobe revealed multiple tightly packed nodules (Fig. 1). A histological examination revealed an unusual image with tightly packed follicular adenomas and adenomatous colloid nodules (Fig. 2). The changes are consistent with findings in the literature described as characteristic of Cowden’s syndrome (CS), which is a dominant hereditary condition characterised by multiple benign and malignant neoplasms and hamartomas. The histology report indicated that the image could suggest Cowden’s syndrome, and the patient was referred for genetic testing. The same year as the left thyroid lobe was removed, a cavernous haemangioma was also removed from the skin of the left thigh.
The phosphatase and tensin homologue gene, PTEN, is a tumour suppressor gene and plays a central part in controlling cell proliferation, differentiation and apoptosis (1). Mutation of the gene contributes to increased cellular proliferation, and somatic mutations of the PTEN gene are associated with a number of different types of cancer (2, 3). PTEN hamartoma tumour syndromes (PHTS) are rare, hereditary conditions and due to germline mutations in the PTEN gene. The condition includes Cowden’s syndrome, Bannayan-Riley-Ruvalcaba syndrome (BRRS), Proteus syndrome and Proteus-like syndromes and autism spectrum disorders associated with macrocephaly (4).
About two years after she had been found to have mammary carcinoma, the patient arrived with her mother for genetic counselling. Her mother related that the patient had been sick a great deal as a child. She was found to have nasal polyps during her childhood. She had a tonsillectomy and appendectomy, and was found to have diabetes mellitus. Her mother related that the patient had always had a large head, which was noticed for the first time when she was a newborn baby. The patient was monitored for a year on this account. The assessment during her childhood ruled out hydrocephalus as the cause of her large head circumference. The large circumference could be the reason why it was difficult to find a wig large enough for the patient’s head in connection with her chemotherapy.
It emerged that the patient had been referred for genetic evaluation 12 – 13 years previously because of a history of breast and ovarian cancer in her mother’s family. At that time the patient did not have cancer. Nor did her mother have cancer, and there was no indication for further genetic evaluation and testing. At that time, genetic testing options were relatively limited, and testing for PTEN gene mutation was not offered. The patient’s father died when he was in his mid-fifties, but not of cancer.
In connection with the genetic counselling for which she was referred on account of suspected Cowden’s syndrome, skin manifestations were detected that were characteristic of PTEN mutation (papillomas and trichilemmomas). The genetic test revealed a mutation of the PTEN gene. This, coupled with the clinical picture, fitted Cowden’s syndrome.
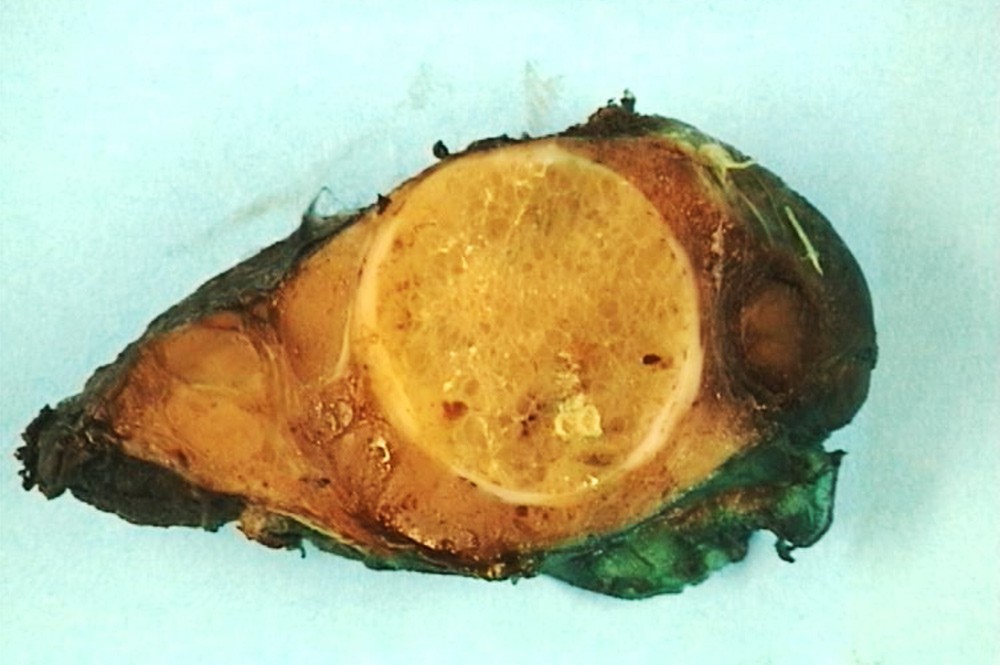
Figure 1 Image (macroscopic) of left thyroid lobe with one large and several small nodules. Both photos: Krystyna Kotanska Grøholt
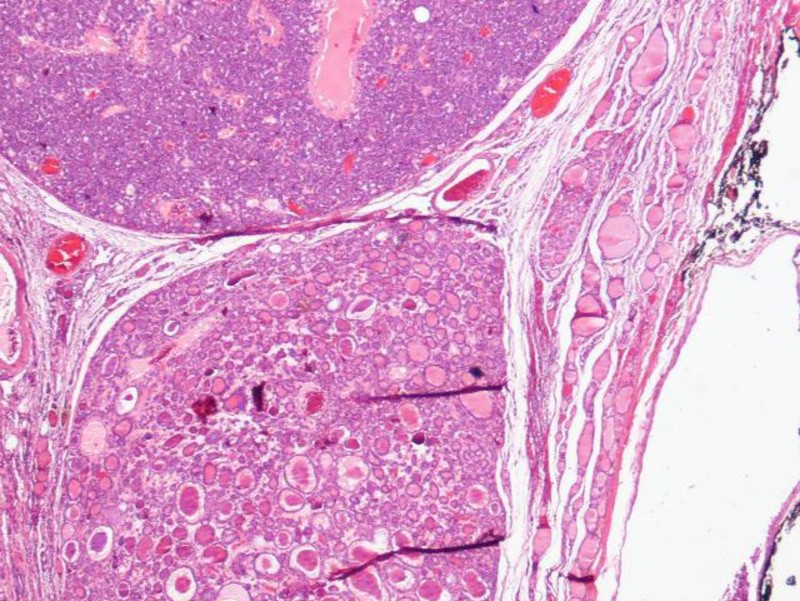
Figure 2 Image (microscopic) of left thyroid lobe with two tightly packed follicular adenomas
Cowden’s syndrome is a dominant hereditary condition characterised among other things by numerous hamartomas, which represent overgrowth of tissue components that should normally be present at the locality in question. Skin changes may consist of papillomas in the mucous membrane of the mouth and on the tongue, trichilemmomas, most frequently on the face, particularly around the nose, eyes and mouth, and/or thickened skin on the hands and feet, so-called acral keratosis (5, 6). Haemangiomas, lipomas and neurofibromas are also common. Benign changes in the thyroid (colloid nodules, adenomas), breast (fibroadenomas, fibrocystic changes) and intestines (hamartomas, ganglioneuromas) occur frequently (5, 6). Almost all individuals with Cowden’s syndrome have a head circumference larger than the 97.5 percentile (7). Macrocephaly in connection with Cowden’s syndrome is probably secondary to megencephaly (7). Many individuals with the syndrome have learning disabilities, some have impaired mental capacity and also motor changes. Individual variation is substantial (5, 6).
There is a substantially elevated risk of cancer, the most prevalent types being breast, thyroid, uterine and renal cancer (8).
It is usually assumed that more than 90 % of individuals with Cowden’s syndrome present with the phenotype in their twenties. The diagnostic criteria for the syndrome have been revised several times (6, 9) (Box 1).
BOX 1
Clinical criteria for Cowden’s syndrome
The patient must meet ≥ three major criteria, one of which must be macrocephaly, Lhermitte-Duclos disease or gastrointestinal hamartomas, or two major and three minor criteria. The box is modified from Pilarski et al. (6).
Major criteria
Breast cancer
Endometrial cancer, epithelial
Thyroid cancer, follicular
Gastrointestinal hamartomas, incl. ganglioneuromas, excl. hyperplastic polyps, ≥ 3
Lhermitte-Duclos disease, adult
Macrocephaly, ≥ 97th percentile: 58 cm for women, 60 cm for men
Macular pigmentation of glans penis
Multiple mucocutaneous lesions:
Multiple trichilemmomas (≥ 3, at least one verified by means of biopsy)
Multiple palmoplantar keratoses (≥ 3)
Mucocutaneous neuromas (≥ 3)
Oral papillomas (≥ 3)
Minor criteria
Autism spectrum disorder
Bowel cancer
Oesophageal glycogen acanthosis (≥ 3)
Lipomas (≥ 3)
Intellectual disability (IQ ≤ 75)
Renal cell carcinoma
Testicular lipomatosis
Thyroid cancer, papillary or follicular
Other thyroid lesions, e.g. adenomas, nodular goitre
Vascular anomalies
Further genetic tests were conducted on the family. The patient’s mother was tested, but she did not have a genetic defect in the PTEN gene. Because of the maternal family history of breast and ovarian cancer, an analysis was performed of her BRCA1 and BRCA2 genes, which did not reveal a mutation. The possibility that the PTEN genetic defect stemmed from the patient’s deceased father cannot be dismissed. Alternatively, it may have arisen de novo in the patient.
After being assessed by a medical geneticist, the patient was referred for examination of the remaining left breast. Two years had passed since carcinoma was diagnosed in the right breast. An MRI scan of the left breast revealed a suspected malignant lesion. A biopsy revealed infiltrating ductal carcinoma, and the patient underwent ablatio of the left breast. In parallel with the detection of the mammary carcinoma of the left breast, a further ultrasound of the right thyroid lobe found multiple nodules, some of them large and indeterminate. Cytological sampling from a small nodule in the right thyroid lobe revealed a cell picture consistent with a colloidal nodule, while the material from a large nodule was not diagnostic. In view of increasing pressure symptoms and throat discomfort, the remaining right thyroid lobe was removed a few months after ablatio of the left breast. The histology of the right thyroid lobe revealed a 90 mm follicular adenoma and several adenomatous colloidal nodules, consistent with findings in the left thyroid lobe.
MRI and CT scans of the patient later the same year showed changes consistent with skeletal metastases in the spinal column and pelvis and multiple small changes consistent with pulmonary metastases. Clinically, these changes were interpreted as spreading from the patient’s mammary carcinoma, and chemotherapy was started. The patient is alive, and receiving regular follow-up and treatment.
Discussion
Cowden’s syndrome is named after Rachel Cowden, the first patient who was described as having many of the characteristic changes found in this patient group (10). Cowden’s syndrome is rare. A Dutch clinical epidemiological study from 1999 estimated its prevalence to be between 1 : 200 000 and 1 : 250 000 (11), but as the syndrome has a variable clinical presentation and is often difficult to recognise, this is believed to be an underestimation (9). Increased possibilities for genetic testing may help to determine the prevalence of the disease, also in subjects who do not meet the classical clinical criteria. It is estimated that 10 – 47 % of persons with PTEN mutation have a de novo mutation (12), i.e., neither of the patient’s parents has the mutation.
The great variation in clinical expression of Cowden’s syndrome makes diagnosing it a challenge. Not all patients found to have a defective PTEN gene meet the clinical criteria for the syndrome. Similarly, there may be patients who meet the clinical criteria for Cowden’s syndrome, but who do not have a detectable PTEN gene mutation (13). Many features of Cowden’s syndrome are subtle and occur frequently in the general population. Clinical findings in various organs such as the skin, thyroid, breast, bowel, central nervous system and soft tissue, including the vascular and urogenital systems, result in patients being attended to by a variety of medical specialists, with a risk of the overall picture not being seen. Dermatologists are often the first to meet patients with the syndrome (14, 15). Detection of a PTEN mutation makes it possible to treat premalignant conditions and thereby improve survival. The patient’s relatives (parents, siblings and children) should be offered genetic testing. In rare cases, children with PTEN gene defects may develop cancer in addition to benign nodules in the thyroid gland (8). It is therefore permissible to test children for this defect. In the event of findings of multiple mucocutaneous papules in young patients, Cowden’s syndrome should be ruled out. Breast and endocrine surgeons who treat breast and thyroid lesions should also have Cowden’s syndrome in mind as a possible diagnosis.
Pathologists have a key and vital part to play in detecting the syndrome (16). New and improved pathology databases with an overview of all specimens submitted for testing from each patient have given pathologists an important diagnostic means of identifying patients who should be tested for PTEN mutation. From a histopathological point of view, findings of a large number of tightly packed follicular adenomas and adenomatous colloid nodules should result in a remark in the results urging clinicians to consider referral for genetic study with Cowden’s syndrome in mind. Follow-up is recommended for patients in whom PTEN mutation is detected with a view to preventing malignant neoplasms or detecting neoplasms at an early stage. Guidelines for follow-up have changed over time, and vary somewhat across institutions. As a result, we have established guidelines during the past few years (8, 13) (Box 2).
BOX 2
Recommended checks
The box is modified from Tan et al. and Gammon et al. (8, 13)
Annual thyroid ultrasound is seldom relevant before the age of ten. Prophylactic thyroidectomy can be considered if it is difficult to assess the gland because of multiple nodules.
Annual mammography and MRI scan of the breasts from the age of 25. Prophylactic mastectomy should be considered.
Annual uterine screening with ultrasound and possibly endometrial cytology tests from the age of 30.
Basic cutaneous examination after genetic testing. Follow-up as needed or about every fifth year.
Annual renal ultrasound from the age of 40.
Colonoscopy every five years from the age of 40.
The patient presented in this case history had a complex of clinical symptoms and findings for several years without their arousing suspicion of a genetic connection. The pathologists reacted to the histological appearance of the thyroid specimen, as a result of which the patient was referred for genetic study. Knowledge of, and focus on Cowden’s syndrome has been increasing both in Norway and internationally over the past ten years, not least as a result of steadily improved multidisciplinary cooperation. The patient in this case history developed her first symptoms many years before diagnostic criteria and follow-up for this rare disease had been established. Cowden’s syndrome was not mentioned in the patient’s therapy programmes from the period when she was diagnosed with breast cancer. According to today’s breast cancer treatment programme, the patient should have been referred for genetic study. Since histological findings for this patient led to genetic testing and detection of a PTEN mutation, several patients with a PTEN mutation have been found at the Department of Pathology, Oslo University Hospital, following findings of characteristic histological features in thyroid specimens.
When the patient in question was referred for genetic study 12 – 13 years earlier because of her family history, she had not yet been found to have cancer. This, coupled with the fact that the testing options were limited at that time, meant that there was no indication for further genetic study. In the case of this patient, early suspicion of Cowden’s syndrome on the part of one or more of the clinicians who treated the patient and subsequent genetic testing might have led to prevention or early diagnosis of her mammary carcinomas.
This case study shows that interdisciplinary cooperation on patients with a complex of symptoms and findings is important. Multidisciplinary meetings at which medical history, symptoms, and clinical, radiological and pathological findings are presented and discussed could contribute to syndromes like Cowden’s being detected so early that prophylactic measures can be implemented.
