On one of the hottest days of the Norwegian summer, a man collapsed in a field. He was admitted to hospital where he underwent a wide range of tests owing to reduced consciousness and high body temperature. He went on to develop an unusual disease course with multiple organ failure and neurological deficits.
The man, who was in his forties and of foreign origin, was in Norway as a seasonal agricultural worker. On the day he was hospitalised, after working in the fields for a few hours he had stated that he felt unwell – before collapsing. He was admitted to the nearest hospital in an unconscious state.
Upon admission, the only information available about the patient was that he had suddenly collapsed. He had apparently been in good health earlier in the day. The ambulance call report was not scanned into the medical records, and information about how he had been found unconscious was not relayed to the hospital personnel.
Upon admission, he had greatly reduced consciousness, a Glasgow Coma Scale score of 3–4 points, and in a preliminary neurological workup his pupils were non-reactive to light. The ambulance personnel had provided partial ventilatory support during his transport to the hospital. Upon arrival in the emergency department, he was not breathing unaided. He was immediately intubated without prior sedation and responded only with some coughing.
Tympanic temperature was measured at 41.2 ºC, rectal temperature was not measured. He showed signs of circulatory shock – with cold, moist and blue-mottled skin, hypotension and tachycardia (blood pressure 70/30 mm Hg, pulse 175 beats/min, sinus tachycardia). He was considered to be critically ill and in need of intensive care.
Echocardiography showed normal left ventricle contractility. The inferior vena cava had completely collapsed and there was very poor filling of both ventricles. CT head, CT thorax and CT abdomen were normal. Blood tests, blood cultures and cerebrospinal fluid analysis were performed. The blood tests revealed severe renal impairment, heart failure and high creatine kinase levels (CK) (Table 1). No cooling interventions were performed in the acute phase.
Table 1
Blood test results upon hospitalisation and over the first five weeks
|
Blood tests
|
Reference levels
|
Admission
|
Day 1
|
Day 2
|
Day 3
|
Days 6-8
|
2 weeks
|
5 weeks
|
|
Leukocytes
|
3.5-11.0 ∙ 109/l
|
14.4
|
9.0
|
8.3
|
6.8
|
9.8
|
8.3
|
7.2
|
|
CRP
|
0-5 mg/l
|
23
|
21
|
20
|
16
|
6
|
3
|
< 1
|
|
Thrombocytes
|
145-390 ∙ 109/l
|
115
|
35
|
78
|
50
|
481
|
690
|
399
|
|
Creatinine
|
60-105 umol/l
|
337
|
143
|
166
|
189
|
68
|
61
|
88
|
|
eGFR creatinine
|
> 60 ml/min/1.73 m2
|
17
|
46
|
63
|
33
|
> 60
|
> 60
|
> 60
|
|
Creatine kinase
|
50-400 U/l
|
7 143
|
21 012
|
14 444
|
8 340
|
1 145
|
-
|
-
|
|
ALT
|
10-70 U/l
|
NA
|
720
|
1 488
|
3 398
|
419
|
-
|
116
|
|
Troponin I
|
< 30 ng/l
|
1 747
|
7 108
|
5 128
|
-
|
-
|
-
|
-
|
|
Bilirubin
|
5-25 umol/l
|
27
|
52
|
69
|
111
|
33
|
-
|
15
|
|
PT-INR
|
0.8-1.2
|
1.2
|
1.8
|
2.3
|
2.4
|
1.2
|
-
|
-
|
|
Fibrinogen
|
2.0-4.0 g/l
|
2.2
|
1.0
|
1.5
|
1.5
|
5.6
|
-
|
-
|
|
APTT
|
25-32 seconds
|
-
|
42
|
36
|
38.5
|
24
|
-
|
-
|
Upon admission, the patient’s medical records were not available and nor was there any information from those who knew him. Health care professionals had no details about what had happened that day, other than that the patient had collapsed. No information was available about previous illnesses, substance use or medications. On the basis of the loss of consciousness and high body temperature, the episode was interpreted as sepsis with unknown focus and severe dehydration.
CRP and leukocytes were only slightly elevated. The patient did not have a stiff neck. He was given antibiotics (penicillin and gentamicin), in addition to high-dose intravenous fluid replacement owing to severe dehydration, renal failure and suspected onset of rhabdomyolysis.
Blood tests, diagnostic imaging and cerebrospinal fluid analysis upon hospitalisation failed to provide a definitive aetiology for the patient’s clinical state with unconsciousness, renal failure, and circulatory and respiratory collapse. Over the following days, he developed multiple organ failure with involvement of the liver, heart and kidneys, as well as disseminated intravascular coagulation (DIC) (Table 1).
CK levels increased up to day 2, and peaked at 21 012 U/l. He underwent forced diuresis for the first few days. His troponin I level increased to a peak of 7 108 ng/l (Table 1), but the patient had no arrhythmias and no changes were detected upon echocardiography or in an electrocardiogram. The patient was kept sedated and intubated in the intensive care unit for seven days and received nutritional and fluid support. He did not require dialysis or vasopressor support.
He underwent repeated CT and MRI scans of the head, without notable findings. Several EEG tests were also performed, which showed generalised background slowing, without epileptic activity. This was interpreted as medication-related. Muscular cramps/spasms were reported, but not tonic-clonic seizures. PCR analysis of the cerebrospinal fluid yielded no evidence of neurotropic viruses (herpes simplex virus/varicella zoster virus/enterovirus), and cultures were negative.
Information from those who knew the patient only became available several days later. It emerged that the patient had previously been in good health. There were no known diseases in the family, and he was not taking any regular medication or using any intoxicants.
He had been working in a field on the day he was hospitalised, wearing whole-body rubber overalls to protect against stinging/prickly plants. It had been over 30 °C in the shade that day, but according to his employer he had had ready access to both water and breaks. He had been advised against working in the rubber overalls.
On the basis of the case history, clinical findings, and clinical and biochemical progression with multiple organ failure, the episode was interpreted as heat stroke. The patient developed complications as a consequence of hyperthermia in the form of respiratory failure, rhabdomyolysis, renal failure, liver failure and disseminated intravascular coagulation.
The patient was extubated after a week, but due to his multiple organ failure he remained in the intensive care unit until day 18, when he was transferred to the neurological department. While in intensive care, it was possible to communicate with him to some degree, and he was able to cooperate on simple matters and showed good understanding of what was said.
After two weeks, he became increasingly lethargic and seemed generally weak. He appeared apathetic and only occasionally made eye contact. Upon neurological examination, he was hypotonic but with spontaneous involuntary and uncoordinated movements of the arms and legs. As the days went by, he developed ataxia in both extremities and trunk, reduced facial expressions, dysphagia and repetitive, uncontrolled tongue movements including tongue protrusion. He did not speak and was slow to engage in motor and cognitive tasks.
The patient clearly had cerebral impairment, but an MRI scan of the brain showed no evidence of structural abnormalities, and blood tests and cerebrospinal fluid analysis provided no evidence of an infectious aetiology. The pronounced ataxia, involuntary movements and reduced facial expressions suggested involvement of the cerebellum and basal ganglia, presumably as a consequence of the heat stroke.
The patient showed decreased general condition after his prolonged stay in the intensive care unit, but over the next few weeks there was no suspicion of organ damage other than brain damage after the heat stroke. The patient’s blood test results normalised and his general condition improved.
A number of medications were tried out over the next few weeks in an attempt to improve the patient’s catatonic-like state. Benzodiazepines (lorazepam and diazepam) were tried for a week. The patient was alert, and gave the impression that he understood most of what was said to him, but he showed persistent stiffness of the extremities in various positions, very slow movements, rigidity, and absence of speech. The benzodiazepines initially helped with the sluggishness, and he began to speak a little, but the treatment was discontinued as its effectiveness was considered uncertain.
Levodopa was tried given the possibility of damage to the basal ganglia, but no effect was seen on either the sluggishness or the involuntary movements. Low dose olanzapine was tried upon suspicion of psychosis, but was soon discontinued when the patient seemed to be recovering spontaneously.
The patient had no symptoms of psychosis later in the disease course. He was also evaluated by psychiatrists owing to uncertainty over his mental state. It was concluded that he showed symptoms of depression, but that this was probably a normal reaction to a serious life event in the form of a physical illness with uncertain prognosis. A low dose of escitalopram was tried without any clear effect.
A gradual improvement occurred over the next few weeks. Upon leaving the hospital, after almost two months of treatment, the man was markedly better. He still had severe neurological deficits in the form of bradykinesia, dysarthria, gait ataxia, and general psychomotor slowing. He appeared cognitively unimpaired and showed insight into his illness, but cognitive testing was not performed.
He was otherwise in good physical health. The patient was discharged to a rehabilitation centre in his home country. The therapists there have been contacted by telephone and report persistent marked neurological deficits.
The man thus underwent an extended period of hospitalisation, including admission to a neurological department owing to signs of brain damage after heat stroke. No structural changes were ever detected in MRI of the brain, even upon discharge.
Nevertheless, a neurological examination upon departure from the hospital revealed clear neurological deficits consistent with damage to both the cerebellum and the basal ganglia.
Discussion
Hyperthermia is a potentially dangerous condition that can cause severe multiple organ failure, including brain damage (1). Hyperthermia should quickly be suspected in patients who collapse on hot days, especially if there are factors involved that would impede cooling (2). Our case report illustrates the vulnerability of the brain to high temperatures and shows that diagnosis can be difficult in the first hours and days (1, 3, 4).
To improve the prognosis after heat stroke, the most important treatment is rapid cooling, intravenous fluids and treatment of complications (2). Our patient did not undergo active cooling upon arrival, but he was admitted to hospital, where the temperature was markedly lower than outside, and quickly received adequate fluid therapy and intensive care.
Heat stroke was not considered as a diagnosis initially, as the patient’s high temperature and unconsciousness on arrival raised suspicion of sepsis and possible meningitis. Additional tests revealed no signs of infection, and by the time heat stroke became a pertinent diagnosis, the patient’s body temperature had already decreased spontaneously. The patient was unconscious on arrival and was promptly placed on respiratory support. The extent of his brain damage therefore remained unknown until he regained consciousness one week later.
Hyperthermia is defined as a core body temperature above 37.5 ºC, and arises due to inadequate thermoregulation (1, 4, 5). Symptoms of hyperthermia include varying degrees of tachycardia, hyperventilation, hypotension, feelings of loss of strength/weakness, nausea and dizziness.
A body temperature above 40 ºC is classified as severe hyperthermia, and is accompanied by an increase in both oxygen demand and metabolic rate. Blood is shunted from the internal organs to the skin and muscles. There is also a risk of gastrointestinal ischaemia. A core body temperature above 40 °C, together with symptoms of central nervous system dysfunction, is classified as heat stroke. The most common symptoms of heat stroke are altered mental status, slurred speech, agitation, inappropriate behaviour, impaired coordination, delirium, seizures and coma.
Common complications of severe hyperthermia are acute respiratory failure, disseminated intravascular coagulation, acute renal failure, rhabdomyolysis, acute liver failure, hypoglycaemia, arrhythmias, cardiac dysfunction, seizures and damage to brain tissue. The prognosis is very variable. The mortality rate is 21–63%, depending on the degree to which body temperature is elevated, the time before cooling and the number of organ systems affected. Recommended treatment is removal of clothing, application of a cooling blanket, and provision of cool drinks or cool intravenous fluids (4).
Hepatocytes, vascular endothelial cells and neurons, particularly in the cerebellum (3), are highly sensitive to hyperthermia. In severe cases, such as in the current case report, multiple organ failure, disseminated intravascular coagulation and cerebral/cerebellar long-term effects may occur.
Body temperature is normally maintained within a tightly controlled range (Fig. 1), and the body’s total heat load is due to a combination of metabolic processes and absorption of heat from the environment. Upon an increase in core body temperature, the preoptic nucleus of the anterior hypothalamus will stimulate efferent fibres in the autonomic nervous system to trigger both sweating and cutaneous vasodilation. Individuals will also typically change their behaviour by minimising skeletal muscle use, withdrawing to a cooler environment and removing items of clothing.
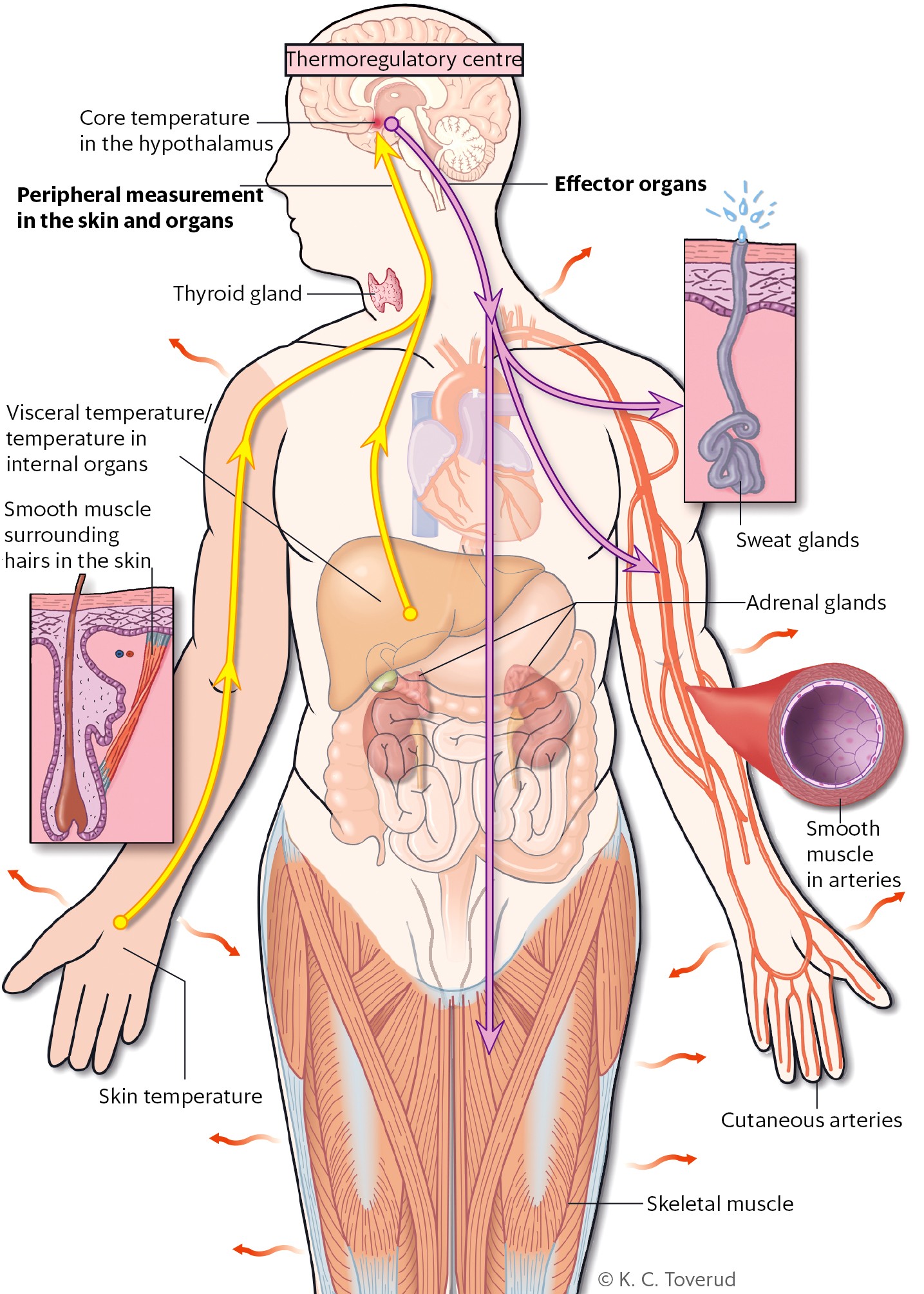
Figure 1 The hypothalamus sends signals to arterial smooth muscle, the sweat glands, smooth muscle surrounding hairs in the skin, skeletal muscles, the adrenal glands, and the thyroid gland to raise or lower the body temperature
Evaporation through the skin is the most effective way of regulating body temperature in warm environments (1, 2, 4). Our patient engaged in physical labour while wearing whole-body rubber overalls on a very hot day, which generated both internal and external heat as well as preventing evaporation through the skin.
The patient had a very high core body temperature, fully at the limit of what the body can tolerate, and quickly developed severe symptoms due to hyperthermia. At a body temperature of 42 ºC, oxidative phosphorylation is reduced and enzyme function decreases. Denaturation of proteins may occur, and a cytokine-mediated systemic inflammatory response is initiated. The production of heat shock proteins also increases (1, 4, 6–9).
Heat shock proteins are neuroprotective proteins that are produced under stress, for example, during large temperature changes, exposure to ultraviolet light, or wounding. The highest concentration of heat shock proteins is found in the brain, in particular in the cerebellum. An increase in the production of heat shock proteins (as in cases of hyperthermia) leads to increased cytokine release and a sepsis-like reaction, which in turn leads to increased blood-brain barrier permeability, increased cerebral oedema and the risk of cell death in the long term (3).
Our patient fell victim to heat stroke. Upon arrival at hospital, he had symptoms of heat stroke in the form of high body temperature and unconsciousness. He also developed multiple organ failure shortly after being hospitalised. He sustained significant brain damage as a result of the heat stroke, which is still evident long afterwards.
Heat stroke is a relatively rare condition in Norway, which has few days with very high temperatures. Since the condition is potentially fatal, it is nevertheless important to be aware of it. It is also important for hospital departments to have good procedures in place for rapid diagnosis and treatment of heat stroke, as well as for correct temperature measurement in the emergency department. Several studies have shown poor consistency between tympanic thermometer measurements and core temperature, and it has been concluded that correctly measured rectal temperature is the most accurate non-invasive temperature measurement (10).
It is possible that had the patient received another type of treatment, such as rapid cooling in the ambulance and in the emergency department, the outcome might have been different. Once in hospital the patient was relatively quickly rehydrated and cooled thanks to the cooler indoor climate. The initial assessment was made difficult by virtue of not knowing the patient’s name, previous medical history, the course of events on the day of admission, and whether he was using any medications or intoxicants.
Medications that may increase vulnerability to heat stroke include anticholinergic drugs, antihistamines, beta blockers, diuretics, calcium blockers, laxatives, neuroleptics and tricyclic antidepressants, as well as poisoning with central stimulants such as cocaine and amphetamine (11). When treating a patient who is unconscious, it is important to obtain as much anamnestic information as possible. Excluding infections will always be a top priority initially.
Kosgallana et al. show in their article that the cerebellum is particularly vulnerable to heat stroke, and that this is often overlooked during clinical examinations (3). Animal studies, and post-mortem examination of the brain after heat stroke, have shown changes in Purkinje cells as well as cell death, and that the extent of cell damage increases with prolonged hyperthermia.
In spite of major neurological deficits, MRI scans of the brain – including the cerebellum – were unremarkable in our patient. Patients with pronounced cerebellar deficits but initially normal brain MRI have been described in the literature. Atrophy of the cerebellum is often not detected by diagnostic imaging until months or years after the event (3). Unfortunately, it was not possible to obtain a post-discharge MRI of our patient as his care was continued in another country.
In addition to cerebral oedema and cell death, studies show that hyperthermia may alter the composition of neurotransmitters in the brain (9, 12). Animal studies demonstrate that if rats are exposed to an environment with a temperature above 38 °C over time, the composition of neurotransmitters in the brain changes. The concentration of GABA and glycine decreases, while that of glutamate and aspartate increases (8).
In addition to being an excitatory neurotransmitter, glutamate has key roles in cell survival and differentiation as well as in the formation and elimination of synapses in the brain. The presence of glutamate is therefore essential, but high concentrations of glutamate are neurotoxic. Cerebellar Purkinje cells produce GABA and are thus inhibitory. GABA also inhibits glutamate release.
The literature shows that other neurotransmitters are also involved in thermoregulation. Upon an increase in temperature, serotonin, prostaglandins and opioid peptides help to increase the permeability of the blood-brain barrier, with the result that serum proteins and other substances are drawn into the brain extracellular space, contributing to cerebral oedema and cell damage (8).
Lorazepam, a GABA agonist, had a beneficial effect on the patient’s symptoms for a period of time. It is possible that this medication reduced the release of neurotoxic glutamate, but as of yet there is no established treatment for central nervous system symptoms following heat stroke (4).
Conclusion
Our patient showed clear symptoms of heat stroke upon admission, but due to difficulty in obtaining anamnestic information and an unknown history of events, the case was initially interpreted as sepsis with unknown focus. This case report illustrates the challenge of examining patients with an incomplete medical history in the emergency department when information from others known to the patient is not available, as well as the importance of correct measurement of core temperature.
The cerebellum and basal ganglia are particularly vulnerable to high temperatures, and brain damage may not necessarily be visible on diagnostic imaging in the acute phase. Early cooling is currently the most important and optimal treatment for hyperthermia, and can prevent long-term effects and death.