A young man was hospitalised with left-side respiration-dependent chest pain. He had a slightly reduced general condition and fever. It was to be a lengthy stay in hospital, with diagnosis of an unusual cause of pulmonary involvement.
A previously healthy man in his late teens was admitted to hospital via the Accident and Emergency Department after twenty-four hours of left-side, respiration-dependent pain.
On admission he had a temperature of 37.6oC, pulse 117 beats/minute, blood pressure 104/57 mm Hg, respiratory rate 24/minute and peripheral O2 saturation of 94 % without extra oxygen. The findings of the physical examination were normal. Blood tests revealed a normal leukocyte count without neutrophilia, and C-reactive protein (CRP) was 85 mg/l (< 5 mg/l). There was low-grade renal failure with creatinine of 106 umol/l (60–105) and a glomerular filtration rate (GFR) of 88 ml/min/1.73 m2 (92–146). Other blood tests were normal. Arterial blood gas was not taken on admission. Chest X-ray showed a consolidated opacity basomedially in the left lung, in addition to patchy opacities in the lower lobe. The right lung was normal, and sinuses were free. Because of suspected bacterial pneumonia, he was started on penicillin 1.2 g x 4 intravenously. In the hours following the first dose of penicillin, the patient developed a facial rash. A penicillin allergy was suspected, and he was switched to intravenous cefotaxime 2 g x 3. The day following admission there was growth of serogroup Y meningococci (Neisseria meningitidis) in two of four blood cultures and in nasopharyngeal secretion.
Could the rash developed by the patient after the first penicillin dose be a sign of a disseminated meningococcal disease rather than an allergic reaction? It was not petechial, looked like a drug-induced exanthem, and vanished when the antibiotic was changed. In three studies of a total of 862 patients with meningococcal infection, 37–49 % developed meningitis without shock, 10–18 % shock without meningitis, 7–12 % shock and meningitis and 18–33 % mild meningococcaemia with neither shock nor meningitis (1).
The patient was still clinically well, with no neck stiffness or mental deficit, but he had persistent pain in the left hemithorax, a rise in leukocytes to 9.4 109/l (3.5–8.8) and a rise in CRP to 320 mg/l. Antibiotic therapy in the form of intravenous cefotaxime was continued after resistance assessment. Members of the patient’s household and two persons he had kissed in the weeks prior to admission received eradication therapy in the form of a single dose of 500 mg ciprofloxacin by mouth.
In households with a case of meningococcal disease, the risk of invasive disease among family members is elevated by a factor of 400–800 (2). The risk of disease is greatest the first few days, and antibiotic prophylaxis should be administered as soon as a diagnosis is confirmed. The guidelines of the Norwegian Institute of Public Health recommend eradication therapy in the form of a single dose of 500 mg ciprofloxacin tablets to individuals in the patient’s household. This also included girlfriends/boyfriends and close friends (3). None of those close to the patient developed meningococcal disease.
A week later, his general condition was still good, but he became increasingly hypoxic with oxygen saturation down to 90 %. Despite seven days of intravenous cefotaxime treatment, his CRP was 199 mg/l. A chest CT scan revealed that almost the entire left thoracic cavity was filled with expansionary pleural fluid and findings were consistent with pneumonia in the adjacent atelectatic left lower lobe (Fig. 1).
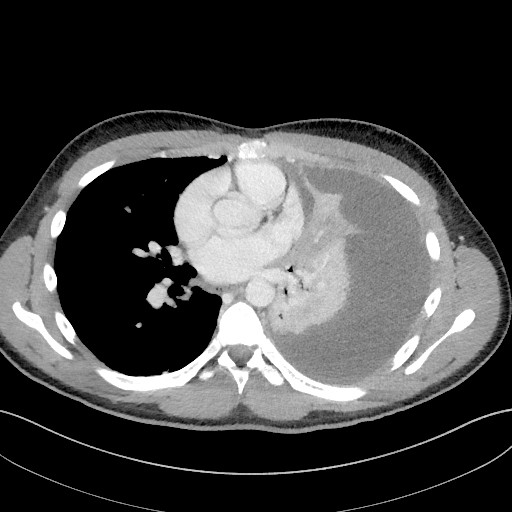
Figure 1 Axial CT images of the chest obtained one week after hospitalisation revealed that almost the entire left thoracic cavity was filled with expansionary pleural fluid which the radiologist interpreted as due to infection
Following ultrasound-guided drainage of the pleural cavity, 1750 ml of clear pleural fluid was aspirated in the course of 48 hours. Analysis of the pleural fluid revealed a low pH of 7.18 (≥ 7.35), low glucose level of 2.8 mmol/l (≥ 3.3 mmol/l), high lactate dehydrogenase (LDH) of 952 U/l (< 200 U/l) and high total protein of 42 g/l (< 30 g/l), consistent with exudate. A chest X-ray taken after aspiration still showed considerable amounts of residual fluid and veiling of half the basal lung field on the left. Pleural ultrasonography revealed multiple loculations and septations.
A single dose of alteplase and rhDNase was applied intrapleurally to break up interpreted fluid loculations, and by the twelfth day a total of 4 620 ml had been drained via the tube. That same day the patient developed a high fever and his general condition deteriorated, with a tripling of the CRP value from 96 mg/l the previous day to 314 mg/l. A repeat chest CT scanshowed a substantial reduction in left-side pleural fluid with residual non-expansionary pleural fluid basally. The following day a further pleural drain was inserted. During the procedure, viscous, purulent material was aspirated from the pleural cavity.
The permeability of the lung capillaries increases during pneumonia, allowing fluid to effuse into the pleural cavity. Pleural exudate forms when the leakage volume exceeds the resorption capacity of the lymphatic system in the pleural cavity. Neutrophil granulocytes and bacteria move over into the fluid. They metabolise glucose anaerobically, which results in a low pH value and low glucose level in the exudate. Persistent inflammation may result in fibrin deposits and hence multiple fluid loculations (4) as revealed by ultrasonography in our patient.
A parapneumonic effusion is defined as complicated when an invasive procedure is necessary to resolve the problem. Empyema means that there is an accumulation of pus in the pleural cavity (4, 5). Because viscous purulent material was aspirated by thoracocentesis, it was concluded that empyema had developed. It was assumed that the empyema was due to a meningococcal infection, because of the growth of meningococci in blood cultures. Direct microscopy and culture of the exudate yielded negative results.
Because there was limited production from both drains, the patient was again put on alteplase and rhDNase intrapleurally, this time twice daily for three successive days. This resulted in tapping of a further 1040 ml fluid. When fluid production from the two drains stagnated, and there was still radiological evidence of residual effusion, the last drain inserted was replaced by one with a larger diameter (from 10 to 16 french). This caused the patient severe pain, but resulted in no further production via the drain. Both drains were therefore removed the following day.
According to the British Thoracic Society guidelines of 2010, drainage of the pleural cavity is indicated if there is clinical evidence of infection and at the same time pleural exudate that is macroscopically purulent, culture-positive, gram-staining positive or has a pH level < 7.2 (6). There is no consensus on the size of the optimal chest tube diameter (6).
In a prospective, non-randomised study, where the inclusion criterion was consistent with the aforementioned indication for drainage of pleural effusion, a comparison was made of draining pleural cavities with tube sizes of < 10F, 10–14F, 15–20F and > 20F. No difference was found between the groups (7). Similarly, inserting a larger drain was not effective with our patient, and in fact it caused more pain than gain.
The patient’s condition improved, and pleural drains were removed after 16 days in hospital. After a mild, clostridium difficile-associated colitis treated with metronidazole, and 19 days in hospital, he was able to go home, afebrile and feeling better. Cefotaxime was replaced by ciprofloxacin tablets 500 mg x 2 so that the total treatment period was four weeks. At a check-up at the infectious diseases clinic three weeks after discharge he was clinically well with normal infection test results and almost normalised chest X-ray.
Discussion
It is not clear why a young, previously healthy man developed disseminated meningococcal infection with atypical manifestation in the form of empyema. He had normal immunoglobulins and there was no other obvious reason for his developing such a disease.
He had Neisseria meningitidis in blood cultures and nasopharyngeal secretions. N. meningitidis is a gram-negative aerobic diplococcus found in the normal flora of the throat in about 10 % of healthy individuals (8).
Point prevalence is age-dependent, and asymptomatic carriage is more common in young people. In a study of nasopharyngeal swabs from approximately 14 000 British teenagers aged 15–19, an increased risk of being a carrier of meningococci was associated with frequenting pubs/clubs, intimate kissing and cigarette smoking Around 33 % of the teenagers with all three risk factors were found to be carriers, compared with 8 % of those without risk factors (9).
According to the Norwegian Institute of Public Health, the combination of close contact with others, partying with high alcohol consumption and little sleep makes young people more vulnerable to developing invasive meningococcal disease during their end-of school celebration period (3). Our patient was a non-smoker, had been to a number of parties in connection with the planned celebrations, and he had had increased exposure to infection, having kissed two girls in the weeks before he was hospitalised.
Meningococcal vaccine is available, but not included in the general vaccination programme. The Institute of Public Health recommends that youngsters aged 16–19 consider conjugate vaccine A+C+W+Y against meningococcal disease, but makes no specific recommendations as to who should be vaccinated (10). Our patient had not been vaccinated against meningococcal disease.
According to population-based retrospective studies of data from monitoring meningococcal disease, where N. meningitidis has been isolated from blood and/or cerebrospinal fluid (CSF), 6–15 % of patients with invasive meningococcal disease develop pneumonia (11, 12).
A low incidence of meningococcal pneumonia and high prevalence of asymptomatic carriage in the general population complicates the diagnostics, and it is possible that the bacterium is actually more frequently a cause of pneumonia than commonly believed.
In the present case, the meningococci belonged to serogroup Y. Several studies have found this serogroup to be most frequently associated with pneumonia (12, 13). Patients infected with serogroup Y are often older and have comorbid conditions (11, 12), in contrast to our patient, who was a young and previously healthy man.
Approximately 1 % of all patients who are hospitalised with community-acquired pneumonia develop empyema, but the figures vary (4, 5). Earlier studies show that meningococci are a very rare cause of empyema, also in patients with meningococcal pneumonia (14). In a Spanish study of 4 751 patients who were hospitalised with community-acquired pneumonia, 6 % developed complicated parapneumonic effusion or empyema. The microbe was known in 72 % of the patients. None of them were infected with N. meningitidis (15).
As there was growth of meningococci in two of four culture bottles from our patient, the microbe was interpreted as being the cause of pneumonia with subsequent formation of empyema. Co-infection with a different type of bacteria in the lung is a differential diagnostic possibility, since direct microscopy and cultivation of pleural effusion were negative.
We find no clear updated international or Norwegian guidelines on the use of intrapleural fibrinolysis of the pleural cavity, and have the impression that the treatment is controversial both in Norway and abroad.
In a major trial in which intrapleural fibrinolysis was compared with a placebo, no reduction was found in the number of patients who were referred for surgery after three months (16). However, in 2011 treatment with alteplase and rhDNase intrapleurally was compared with a placebo. This study found a significant improvement in terms of lung opacity reduction as measured by chest X-ray. After three months, a reduction was also found in the number of patients who needed surgical intervention – 2/48 (4 %) compared with 8/51 patients (16 %) (17).
Because of this study, we tend at our hospital to choose intrapleural treatment with alteplase and rhDNase if conventional drainage of the pleural cavity fails. Nonetheless, there is a need for guidelines and large, randomised trials of this treatment.
Conclusion
In the event of slow clinical response, persistent high inflammation markers, fever and/or hypoxia in a patient who is being treated for pneumonia, the possibility of pleural effusion and empyema development should be considered.
It is possible that meningococcal pneumonia without sepsis and meningitis occurs more frequently than commonly believed, because it is a difficult diagnosis on account of the low incidence of invasive disease and high prevalence of asymptomatic carriage.