Maternity care in Norway has been a topic of discussion for decades. Internationally, the trend has been towards centralisation of childbirth services, for both financial and medical reasons. It has been maintained that centralisation ensures better utilisation of financial and staff resources and that the outcomes for mother and child are better, particularly in the case of high-risk deliveries (1, 2). The risk that failings in the maternity care provision may lead to the injury or death of mother or child has been found to be greater in small maternity units (1, 3).
Norway has a scattered population, and the Norwegian parliament, the Storting, has decided that we should provide a differentiated and decentralised system of maternity care. Differentiated delivery of maternity services means that different options must be available, to ensure that low-risk women have an opportunity to give birth in high-tech institutions, midwife-led birth units or at home. In Norway, there has been a three-tier system of maternity care, with institutions categorised on the basis of delivery rates, staffing requirements and risk status (4–6): midwife-led birth units (a minimum of 40 deliveries per year, on-call midwifery staff), hospital maternity wards (a minimum of 400–500 deliveries per year, on-call obstetrician and anaesthetist, midwifery and theatre staff as required) and maternity clinics (a minimum of 1 500 deliveries per year, obstetrician and anaesthetist present, on-call paediatrician, midwifery and theatre staff as required, paediatric ward with an intensive care unit). So-called modified midwife-led birth units (with facilities for performing emergency caesarean sections if transport is considered unsafe) have also been set up in some places (6).
The Medical Birth Registry routinely receives data about all childbirths from the actual place of delivery, not from the mother’s intended place of delivery at the time she went into labour. Consequently, we have only limited knowledge of the incidence of, reasons for, and outcomes of intrapartum and postpartum transfers from midwife-led birth units to hospital.
The study’s objective was to clarify whether births in midwife-led birth units were intended to take place there, and how often women who started giving birth in a midwife-led birth unit had to be transferred to a hospital. We also wanted to survey the reasons for hospital transfers, ascertain at what point in the birthing process transfers took place, the means of transport used and the outcomes for these deliveries (sphincter injury, blood loss, Apgar score and survival for children up to five years of age). This information is important to facilitate an assessment of the quality of the selection process for midwife-led birth units and the birthing process there.
Material and method
The material consists of detailed data about births that took place in midwife-led birth units between 1 January 2008 and 31 December 2010. The material also includes data about births for which a midwife-led birth unit had been the intended place of delivery but where the woman was transferred, either intrapartum or postpartum, to a different maternity institution. Data were collected by means of a supplementary form drawn up by the Norwegian Directorate for Health and Social Affairs in partnership with the Norwegian Institute of Public Health in 2007 (fig 1). This was distributed to all maternity institutions in the country (midwife-led birth units, hospital maternity wards and maternity clinics). All district midwives and midwives involved with home births were also informed and the form was sent to them. The form was also to be completed when the outcome of a planned home birth was a hospital transfer and for deliveries in transit that were unrelated to births in midwife-led birth units. Data from the latter events were not included in this study.
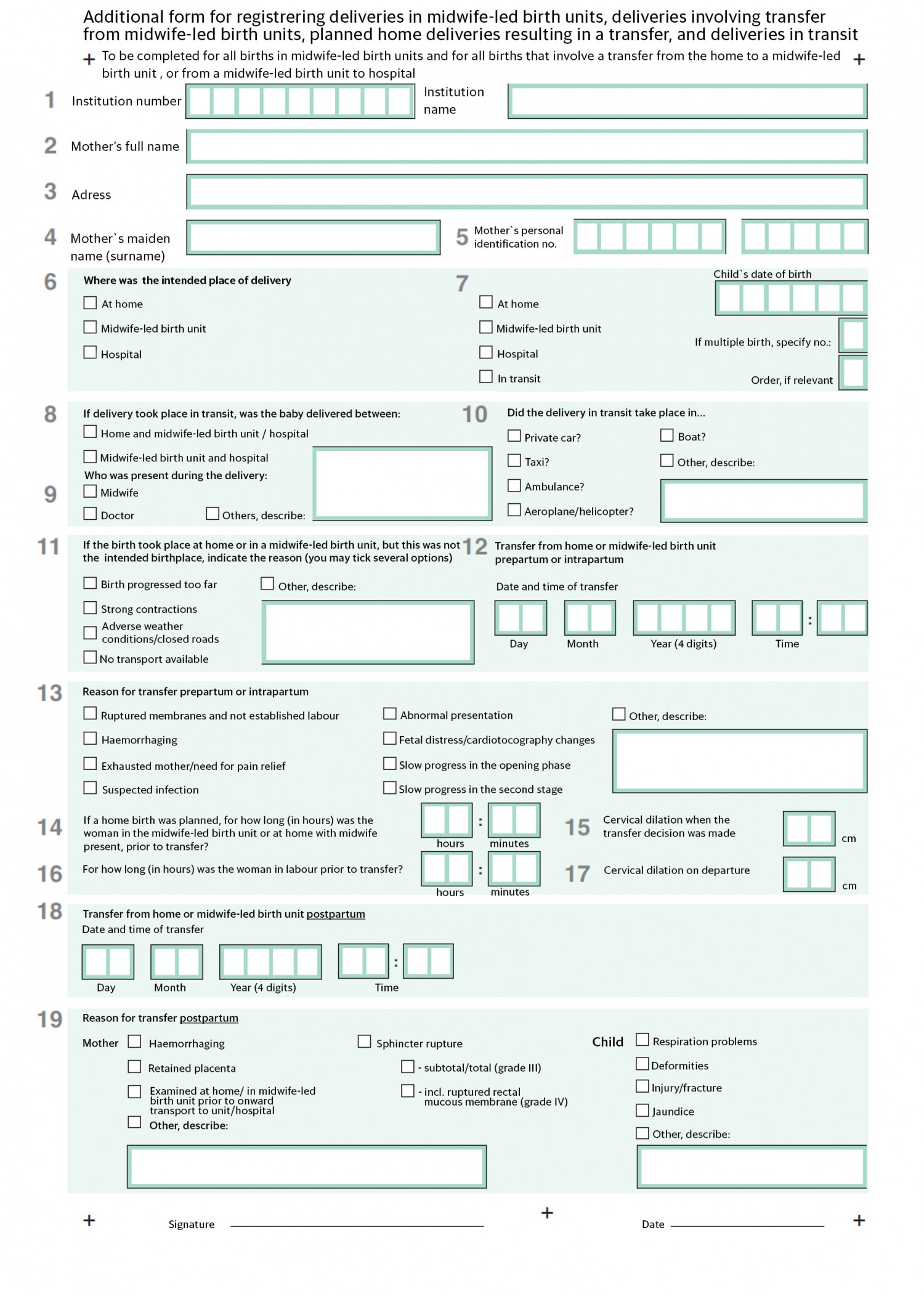
Figure 1 Supplementary form used throughout the project period
Data were collected pursuant to the Medical Birth Registry Regulations (7) and the information was managed in accordance with procedures drawn up by the Norwegian Institute of Public Health in its capacity as the registry’s data administrator. Data were quality assured and analysed by staff at the Norwegian Institute of Public Health. There is no need to obtain the consent of the registered individuals in order to use information submitted to the Medical Birth Registry, nor is approval by the regional ethics committee (REK) required for analysing this data if the analysis is integral to the administration of the registry.
When the study commenced, there were 14 midwife-led birth units in Norway: Føderiket (the former Rikshospitalet in Oslo), Hallingdal (Ål), Lykkeliten (Rjukan), Tynset and Valdres (Fagernes) administered by the Southern and Eastern Norway Regional Health Authority; Lærdal and Odda governed by the Western Norway Regional Health Authority; and Mosjøen, Brønnøysund, Lofoten, Steigen, Midt-Troms (Finnsnes), Sonjatun (Nordreisa) and Alta governed by the Northern Norway Regional Health Authority. The midwife-led birth units in Lærdal, Odda and Lofoten were modified units throughout the study period. One midwife-led birth unit (Lykkeliten) was closed down in the period.
The supplementary form was completed by the midwife in charge of the delivery at the midwife-led birth unit, even if the birthing woman was transferred to hospital and delivery took place while in transit to or in hospital. Completed forms were submitted to the Norwegian Institute of Public Health where they were scanned and checked. Based on information about the identity of the woman and the date of birth of the child, the data were linked with the relevant standard birth report submitted to the Medical Birth Registry. Missing forms were chased up with the appropriate midwife-led birth unit by telephone.
A total of 27 supplementary forms that were completed in the course of the study period could not be linked to any routine data submitted to the Medical Birth Registry, mainly due to insufficient information about the identity of women with foreign names. Furthermore, there was not always a perfect match between the option ticked on the supplementary form and the registered birthplace category recorded in the Medical Birth Registry. For the purpose of analysis, we have used the information provided in the supplementary form as the gold standard.
Information from standard and modified midwife-led birth units is provided in three categories:
-
births in midwife-led birth units that were intended to take place there
-
births in midwife-led birth units that were intended to take place elsewhere
-
births that were planned for midwife-led birth units but that took place elsewhere
Furthermore, we show the results for a comparison group consisting of low-risk deliveries in hospitals run by the regional health authorities of Southern and Eastern Norway, Western Norway and Northern Norway during the study period. We have defined low-risk births as all deliveries of infants born after 36 weeks gestation, except deliveries by women with chronic diseases such as hypertension, kidney disease, rheumatoid arthritis or heart disease, or who had suffered pregnancy complications such as gestational diabetes and hypertensive complaints. Also excluded were planned caesarean deliveries and deliveries that were induced.
The analyses were conducted using the software SPSS version 22.0 (IBM Corp., Armonk, NY, US) and R version 3.2.4 (8). In order to investigate whether group differences were statistically significant, a non-parametric significance test (chi-squared test) was used. P < 0.05 was considered statistically significant.
Results
A total of 3 546 supplementary forms were received, of which 2 734 referred to childbirth in midwife-led birth units and were thus included in the study (fig 2). Among them, 2 514 forms referred to deliveries that took place in a midwife-led birth unit while 220 forms referred to births for which a midwife-led birth unit had been the intended place of delivery, but which in fact took place elsewhere. Based on the standard reports submitted routinely to the Medical Birth Registry, a total of 2 556 births were reported to have taken place in a midwife-led birth unit, which amounted to 1.4 % of all births recorded in the Medical Birth Registry (9). The coverage of the supplementary forms for deliveries in midwife-led birth units was therefore 98.4 %
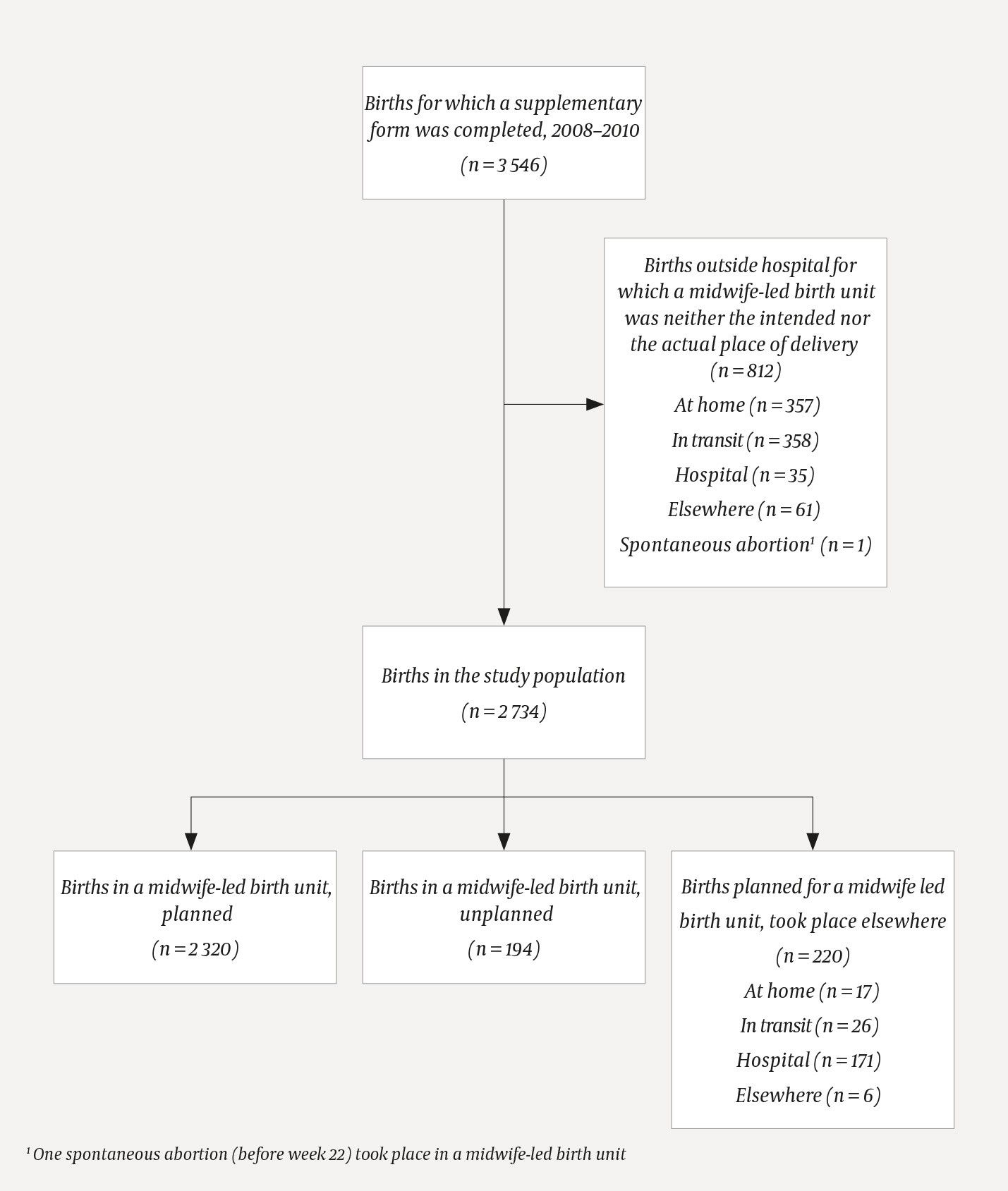
Figure 2 Categories of collected data and deliveries included
Table 1 provides an overview of the deliveries included in the study by regional health authority and midwife-led birth unit, as well as the intended and actual place of delivery. The midwife-led birth unit had been the intended place of delivery for 2 320 of the 2 514 deliveries that took place there (92.3 %), while 194 (7.7 %) had been planned for elsewhere.
Table 1
Births by actual and intended place of delivery, 2008–10.
|
Midwife-led birth unit,
Regional Health Authority
|
Intended place of delivery: Number (%)
|
Total1
|
|
Midwife-led birth unit
|
Hospital
|
|
Føderiket (Oslo), Southern and Eastern
|
344 (100)
|
0 (0)
|
344
|
|
Hallingdal (Ål), Southern and Eastern
|
1 (33.3)
|
2 (66.7)
|
3
|
|
Lykkeliten (Rjukan), Southern and Eastern
|
21 (77.8)
|
6 (22.2)
|
27
|
|
Tynset, Southern and Eastern
|
230 (93.9)
|
14 (5.7)
|
245
|
|
Valdres, Southern and Eastern
|
96 (88.1)
|
13 (11.9)
|
109
|
|
Lærdal, Western
|
218 (90.1)
|
22 (9.1)
|
242
|
|
Odda, Western
|
183 (98.4)
|
3 (1.6)
|
186
|
|
Alta, Northern Norway
|
249 (87.4)
|
36 (12.6)
|
285
|
|
Brønnøysund, Northern Norway
|
114 (96.6)
|
4 (3.4)
|
118
|
|
Lofoten, Northern Norway
|
346 (93.8)
|
18 (4.9)
|
369
|
|
Midt-Troms (Finnsnes), Northern Norway
|
308 (91.7)
|
27 (8.0)
|
336
|
|
Mosjøen, Northern Norway
|
140 (84.3)
|
26 (15.7)
|
166
|
|
Sonjatun (Nordreisa), Northern Norway
|
59 (81.9)
|
13 (18.1)
|
72
|
|
Steigen, Northern Norway
|
11 (91.7)
|
1 (8.3)
|
12
|
|
Deliveries in midwife-led birth units
|
2 320 (92.3)
|
185 (7.4)
|
2 514
|
|
Deliveries elsewhere
|
220 (100)
|
0 (0.0)
|
220
|
|
Deliveries included in the study
|
2 540 (92.9)
|
185 (6.8)
|
2 734
|
Among the 2 540 women who had planned to give birth in a midwife-led birth unit, a total of 174 (6.9 %) were transferred to hospital intrapartum. Among the 2 514 women who gave birth in a midwife-led birth unit, 95 (3.8 %) were transferred to hospital postpartum. Among nulliparous women 19.5 % were transferred intrapartum and 3.8 % postpartum, while among multiparous women the intrapartum transfer rate was 3.4 % and the postpartum transfer rate 3.7 % (data not shown).
Figure 2 shows the actual place of delivery for the 220 births that had been planned for a midwife-led birth unit but which took place elsewhere. There were 26 deliveries in transit, of which 16 took place between the home and the midwife-led birth unit; four in a private car and the rest in an ambulance (road vehicle/plane/helicopter). A midwife was present at 18 of the deliveries in transit, while the ambulance personnel assisted in eight such cases and the father of the child in three such cases. No doctor was reported to be present at any of the deliveries in transit.
Among the reasons listed for unplanned births at home or in a midwife-led birth unit (n = 203) the most common was that the birth had progressed too far for transport to be considered practical (139 cases, 68.5 %), and/or frequent and heavy maternal contractions (71 cases, 35.0 %). In four cases adverse weather conditions /closed roads were cited as the reason and in seven cases there was no suitable means of transport available (data not shown).
Table 2 provides an overview of the most important reasons why women are transferred to hospital before or during a birth that was planned to take place in a midwife-led birth unit. Slow progress in the opening phase was listed as a contributing or sole reason in 67 of 174 such cases (38.5 %).
Table 2
Reasons for prepartum and intrapartum transfers in cases of planned midwife-led birth unit deliveries, 2008–10
|
Reasons for prepartum and intrapartum transfers, n = 174
|
Number1
|
|
Ruptured membranes without established birth (>24 h)
|
26
|
|
Haemorrhage
|
0
|
|
Exhausted mother /need for pain relief
|
35
|
|
Suspected infection
|
4
|
|
Abnormal position / presentation
|
16
|
|
Fetal distress/ cardiotocography changes
|
41
|
|
Slow progress during the opening phase
|
67
|
|
Slow progress during the second stage
|
11
|
|
Other
|
16
|
The most important reasons for postpartum transfers included severe maternal perineal tears, haemorrhaging or retained placenta, whereas the most frequent cause in the case of the child was respiration problems (data not shown).
When intrapartum transport to hospital was necessary, it took an average of 10.1 hours (median 8.5 hours, range of variation 0–40 hours) from arrival at the midwife-led birth unit until a transfer decision was made, and the dilation of the cervix was 5 cm (average and median, range of variation 0–10 cm).
Table 3 shows the birthing women’s characteristics as well as results from standard and modified midwife-led birth units in the three categories of delivery covered by the study. Additionally, the same data is specified for a low-risk birthing population in hospital (maternity ward or clinic). There were 7 (0.4 %) operative vaginal deliveries at standard midwife-led birth units, 28 (3.5 %) at modified midwife-led birth units and 28 (12.7 %) among those who were transferred to hospital intrapartum. In the low-risk birthing population in hospital, vacuum or forceps was used in 10.4 % of deliveries, which is a considerably higher rate than in the midwife-led birth units (p < 0.001). The caesarean section rate for modified midwife-led birth units was 9.5 %, 11.8 % among those transferred from a midwife-led birth unit to a hospital, and 6.2 % in the comparison group. In the midwife-led birth unit population, 0.9 % of women haemorrhaged more than 1 500 ml, while the rate was 1.5 % in the comparison group (p = 0.02). Among the children born at a midwife-led birth unit, 0.6 % had an Apgar score of < 7 after five minutes, compared to 1.0 % of the children in the comparison group born in hospital (p = 0.04).
Table 3a
Characteristics, complications and outcomes for planned and unplanned births at midwife-led birth units, for births planned for midwife-led birth units that took place elsewhere and for low-risk births in hospital, 2008–10. Data obtained from supplementary forms linked with data from the Medical Birth Registry (MFR) a) Information on deliveries and b) Information on the condition of neonates.
|
a
|
|
Births in midwife-led birth units, planned
|
Births in midwife-led birth units, unplanned
|
Births planned for a midwife-led birth unit, took place elsewhere
|
Births in hospital, low risk1
|
|
Deliveries
|
2 298 of 2 320 linked with
MFR data
|
189 of 194 linked with MFR data
|
220 of 220 linked with MFR data
|
105 358 from MFR
|
|
Woman and pregnancy
|
Categories
|
Ordinary (n= 1 557)
|
Modified (n = 741)
|
Ordinary (n=141)
|
Modified (n=48)
|
Ordinary (n=178)
|
Modified (n=42)
|
|
|
|
N
|
%
|
N
|
%
|
N
|
%
|
N
|
%
|
N
|
%
|
N
|
%
|
N
|
%
|
|
Parity
|
0
|
225
|
14.5
|
216
|
29.1
|
46
|
32.6
|
13
|
27.1
|
90
|
50.6
|
24
|
57.1
|
45 700
|
43.4
|
|
|
1+
|
1 332
|
85.5
|
525
|
70.9
|
95
|
67.4
|
35
|
72.9
|
88
|
49.4
|
18
|
42.9
|
59 658
|
56.6
|
|
Gestation
|
Gestation< 36 weeks
|
2
|
0.1
|
10
|
1.3
|
5
|
3.5
|
4
|
8.3
|
1
|
0.6
|
0
|
0.0
|
0
|
0.0
|
|
|
≥ 36 weeks
|
1 552
|
99.7
|
728
|
98.2
|
136
|
96.5
|
44
|
91.7
|
174
|
97.8
|
41
|
97.6
|
104 396
|
99.1
|
|
|
Missing
|
3
|
0.2
|
3
|
0.4
|
0
|
0.0
|
0
|
0.0
|
3
|
1.7
|
1
|
2.4
|
962
|
0.9
|
|
Presentation
|
Normal, vertex
|
1 470
|
94.4
|
710
|
95.8
|
130
|
92.2
|
46
|
95.8
|
150
|
84.3
|
39
|
92.9
|
98 182
|
93.2
|
|
|
Breech
|
19
|
1.2
|
14
|
1.9
|
2
|
1.4
|
0
|
0.0
|
6
|
3.4
|
0
|
0.0
|
1 929
|
1.8
|
|
|
Other
|
67
|
4.3
|
17
|
2.3
|
8
|
5.7
|
2
|
4.2
|
22
|
12.4
|
3
|
7.1
|
5 229
|
5.0
|
|
|
Missing
|
1
|
0.1
|
0
|
0.0
|
1
|
0.7
|
0
|
0.0
|
0
|
0.0
|
0
|
0.0
|
18
|
0.0
|
|
Operative deliveries:
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Vacuum
|
Yes
|
7
|
0.4
|
24
|
3.2
|
0
|
0.0
|
2
|
4.2
|
25
|
14.0
|
0
|
0.0
|
9 218
|
8.7
|
|
Forceps
|
Yes
|
0
|
0.0
|
2
|
0.3
|
0
|
0.0
|
0
|
0.0
|
1
|
0.6
|
2
|
4.8
|
1 761
|
1.7
|
|
Caesarean sections:
|
Elective
|
0
|
0.0
|
44
|
5.9
|
0
|
0.0
|
0
|
0.0
|
0
|
0.0
|
0
|
0.0
|
0
|
0.0
|
|
|
Acute
|
1
|
0.1
|
27
|
3.6
|
0
|
0.0
|
3
|
6.3
|
21
|
11.8
|
5
|
11.9
|
6 564
|
6.2
|
|
|
Unspecified
|
1
|
0.1
|
1
|
0.1
|
0
|
0.0
|
0
|
0.0
|
0
|
0.0
|
0
|
0.0
|
8
|
0.0
|
|
Complications:
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Sphincter injury, grade ¾
|
Yes
|
13
|
0.8
|
18
|
2.4
|
2
|
1.4
|
0
|
0.0
|
2
|
1.1
|
0
|
0.0
|
2 410
|
2.3
|
|
Haemorrhage > 500 ml
|
500–1
500 ml
|
58
|
3.7
|
48
|
6.5
|
12
|
8.5
|
2
|
4.2
|
15
|
8.4
|
4
|
9.5
|
12 378
|
11.7
|
|
|
> 1 500 ml, transfusion
|
10
|
0.6
|
9
|
1.2
|
3
|
2.1
|
1
|
2.1
|
5
|
2.8
|
0
|
0.0
|
1 604
|
1.5
|
|
|
> 500 ml, no further details
|
15
|
1.0
|
0
|
0.0
|
0
|
0.0
|
0
|
0.0
|
5
|
2.8
|
0
|
0.0
|
264
|
0.3
|
Table 3b
Characteristics, complications and outcomes for planned and unplanned births at midwife-led birth units, for births planned for midwife-led birth units that took place elsewhere and for low-risk births in hospital, 2008–10. Data obtained from supplementary forms linked with data from the Medical Birth Registry (MFR) a) Information on deliveries and b) Information on the condition of neonates.
|
b
|
|
Births in midwife-led birth units, planned
|
Births in midwife-led birth units, unplanned
|
Births planned for a midwife-led birth unit, took place elsewhere
|
Births in hospital, low risk1
|
|
Newborn infants1
|
2 298 of 2 320 linked with
MFR data
|
190 of 195 linked with MFR data
|
220 of 220 linked with MFR data
|
105 358 from MFR
|
|
The child
|
Categories
|
Ordinary (n= 1 557)
|
Modified (n = 741)
|
Ordinary (n=142)
|
Modified (n=48)
|
Ordinary (n=178)
|
Modified (n=42)
|
|
|
|
N
|
%
|
N
|
%
|
N
|
%
|
N
|
%
|
N
|
%
|
N
|
%
|
N
|
%
|
|
Weight at birth
|
< 2 500 g
|
3
|
0.2
|
11
|
1.5
|
7
|
4.9
|
1
|
2.1
|
0
|
0.0
|
0
|
0.0
|
953
|
0.9
|
|
|
2 500–4 500 g
|
1 515
|
97.3
|
701
|
94.6
|
130
|
91.5
|
40
|
83.3
|
172
|
96.6
|
40
|
95.2
|
101 569
|
96.4
|
|
|
> 4 500 g
|
39
|
2.5
|
29
|
3.9
|
4
|
2.8
|
7
|
14.6
|
6
|
3.4
|
2
|
4.8
|
2 789
|
2.6
|
|
|
Missing
|
0
|
0.0
|
0
|
0.0
|
1
|
0.7
|
0
|
0.0
|
0
|
0.0
|
0
|
0.0
|
47
|
0.0
|
|
Apgar score after 5 min
|
< 7
|
1
|
0.1
|
10
|
1.3
|
1
|
0.7
|
2
|
4.2
|
2
|
1.1
|
1
|
2.4
|
1 029
|
1.0
|
|
|
≥ 7
|
1 552
|
99.7
|
730
|
98.5
|
139
|
97.9
|
45
|
93.8
|
174
|
97.8
|
41
|
97.6
|
104 289
|
99.0
|
|
|
Missing
|
4
|
0.3
|
1
|
0.1
|
2
|
1.4
|
1
|
2.1
|
2
|
1.1
|
0
|
0.0
|
40
|
0.0
|
Among the entire midwife-led birth unit population there were three still births, all of which were intrauterine deaths found on arrival. Five live infants died between 29 days and one year of their birth. None of these deaths could be related to complications at birth. None of the children in the midwife-led birth unit population were registered as dead between the ages of one and five.
Discussion
Our findings indicate that risk selection and outcomes for midwife-led birth units are satisfactory. A total of 6.9 % of the women who had planned to give birth in a midwife-led birth unit were transferred intrapartum and 3.8 % were transferred postpartum, due to circumstances relating to the mother or the child. Most transfers were uneventful, and the reasons most commonly cited were slow progress in the opening phase, the need for further pain relief, no delivery imminent more than 24 hours after ruptured membranes, discoloured amniotic fluid or changes to the fetal heart sound. Among nulliparous women who had planned to give birth in a midwife-led unit, 19.5 % were transferred intrapartum. This is a considerable proportion, and nulliparous women who wish to give birth in a midwife-led birth unit must be informed of this. However, the transfer rate in our study is clearly lower than the reported rate for midwife-led birth units in England, where observations indicate that 30–43 % of nulliparous women in midwife-led birth units are transferred to a hospital (10, 11).
The most common reasons for postpartum transfers were retained placenta, suspected tears that required repair by a doctor, or respiratory problems in the newborn infant. The use of vacuum/forceps, the incidence of sphincter injuries and the incidence of Apgar score < 7 after 5 minutes demonstrated satisfactory outcomes for deliveries in midwife-led birth units as well as for maternal transfers.
The reasons why 7.7 % of deliveries in midwife-led birth units were intended to take place elsewhere, may be that the women waited too long before setting off to hospital, or that the birth progressed so fast that they would be unable to get to hospital and that the only option available if an unplanned home birth or delivery in transit was to be avoided, was to travel to the midwife-led birth unit. Adverse weather conditions or non-availability of suitable means of transport were rare reasons for unintended deliveries in midwife-led birth units. It is also somewhat surprising that 1.4 % of births in midwife-led birth units are breech deliveries.
The organisation of maternity services and the number of maternity institutions in Norway will depend on factors such as maternal accessibility, quality of service, economy and political decision-making. It has been decided that we should offer a differentiated and decentralised service provision in a three-tier system of maternity institutions (midwife-led birth units, hospital maternity wards, maternity clinics) (4–6). These categories were formerly based on delivery rates and staffing requirements, but they are now based on quality requirements (12).
It is important that all types of maternity institutions are familiar with their own results. Information reported to the Medical Birth Registry is recorded under the actual birthplace. Consequently, the data that are routinely submitted to the Medical Birth Registry do not always provide an adequate basis for assessing the quality of midwife-led birth units and small maternity wards that requisition maternal transfers to larger maternity institutions. Each institution’s results must be analysed according to the intention-to-treat principle, i.e. outcomes must be reported for all birthing women admitted, including those who are transferred intrapartum or postpartum. If a midwife-led birth unit can demonstrate good results for the deliveries that take place within the institution, but poor results for deliveries in transit, then the quality of the services provided by that institution is not necessarily good. This study sought to examine this particular issue.
The findings show satisfactory results for mother and child following deliveries in midwife-led birth units. Only 0.6 % of the children had an Apgar score of < 7 after 5 minutes, and we found no data to suggest that serious injuries or deaths in mother or child were related to the midwife-led birth unit delivery per se. The operative vaginal delivery rate was 0.4 % in standard midwife-led birth units. These results match earlier Norwegian and international studies (13– 20). The study demonstrated a conspicuously high incidence of caesarean deliveries among planned births in modified midwife-led birth units; contrary to the intention, these were not limited to emergency caesarean sections.
The study sheds light on the reasons for intrapartum and postpartum transfers to hospital, at what point in the birthing process transfers took place, and the means of transport. A good ambulance service is clearly important for the midwife-led birth units.
In 2008, at the start of the project period, there were 55 maternity institutions in Norway, of which 14 were midwife-led birth units. In the course of the study period 1.4 % of all childbirths took place in midwife-led birth units. There are currently 47 maternity institutions, of which six are midwife-led birth units. The following eight units have been closed down:
Lykkeliten (2008), Føderiket, Lærdal and Steigen (2011), Valdres and Odda (2013), as well as Hallingdal and Mosjøen (2016). In 2016 a total of 0.7 % of all childbirths took place in midwife-led birth units (9). Norwegian health authorities have now recommended the winding up of modified midwife-led birth units (12), and there is currently only one such modified unit in the country (Lofoten).
Some maternity services are provided by institutions similar to midwife-led birth units (low-risk units) at Oslo University Hospital (the ABC clinic, Ullevål hospital), Stavanger University Hospital (Fødeloftet) and Haukeland University Hospital (Storken). These units were not included in the study, but it will be important for them to be able to document results for birthing women who are transferred from these low-risk units to ordinary maternity wards.
In Denmark, Sweden and Finland, maternity care services are more centralised than in Norway. In these countries there are very few maternity wards with less than 1 000 deliveries per year, and Norway has more than twice as many maternity institutions relative to the birth rate. Geography and settlement patterns may well be different, but this can hardly explain the large differences in the number of maternity institutions.
It is a strength of our study that it is population-based, national in scope and prospective. We were able to supplement the collected material with data routinely submitted to the Medical Birth Registry. The supplementary forms provided details about virtually all deliveries in midwife-led birth units during the study period, including the reasons for transfers to hospital, at what point in the birthing process transfers took place, what means of transport was used, and information about deliveries in transit. Furthermore, the supplementary forms provided detailed information about births that had been planned for a midwife-led birth unit, but that took place elsewhere.
An important weakness of the study is that the number of deliveries included is low, and that all findings associated with rare events such as severe maternal haemorrhage, still births, very low Apgar scores and neonatal death, must be interpreted with care.
Conclusion
The study’s results suggest that the risk selection and outcomes for midwife-led birth units are satisfactory. While only few multiparous women who planned to give birth in a midwife-led birth unit had to be transferred intrapartum to hospital, nearly one in five nulliparous women were transferred. Most of these transfers were uneventful. The study provided knowledge about delivery outcomes that are required for the quality assessment of selection for and delivery in midwife-led birth units. All low-risk maternity units and small maternity wards should be in a position to document such knowledge.
