Dizziness and unsteadiness are non-specific symptoms that are often caused by vestibular system disorders. When patients have neurological findings as well, however, the possibility of disease elsewhere in the nervous system should be considered. These symptoms may be signs of a serious systemic disease, as illustrated by this case report.
A man in his late twenties contacted his GP after feeling increasingly dizzy and unsteady for some days. His GP suspected benign paroxysmal positional vertigo, but the patient’s symptoms persisted even after Epley’s manoeuvre had been used in an attempt to treat him. Two months after his initial contact with his GP, he additionally developed right-side facial palsy, double vision, headache and tinnitus, with gradual onset. He was therefore referred acutely to the Ear, Nose and Throat Department for assessment. A clinical examination found peripheral facial palsy, but no other definite pathological findings. On suspicion of Bell’s palsy he commenced an outpatient course of prednisolone 60 mg x 1 for five days, before tapering by 10 mg daily until discontinuation. Borreliosis serology was also performed. The patient felt unsteady and had headache and was therefore referred for an outpatient head MRI. When his blood tests revealed positive serology for IgM borrelia antibody after a few days, it was decided to add doxycycline 100 mg two tablets daily for 14 days to treat possible neuroborreliosis. However, the tests were negative for IgG borrelia antibodies, so there was only a slight suspicion of neuroborreliosis.
The most common cause of an increase in IgM borrelia antibodies in isolation is non-specific reactivity. In borreliosis cases, tests for IgG and IgM borrelia antibodies may be negative at an early stage of the disease. Repeat serology after 6–8 weeks is usually recommended.
On the phone to the Ear, Nose and Throat Department, the patient reported a swift improvement in his symptoms. The double vision and headache vanished, and the facial palsy regressed to some extent. However, the symptoms recurred a week after the discontinuation of systemic steroids, and he was admitted acutely to the Department of Neurology with suspected neuroborreliosis. He had not yet had a head MRI. The patient was in relatively good general condition on admission, and able to give a good account of his history of illness. His parents were originally from Southeast Asia, but he himself was born and grew up in Norway. The patient did not know of any neurological diseases among close relatives.
A neurological examination found atactic pursuit eye movements, horizontal and vertical nystagmus, right-side abducens palsy and peripheral facial palsy. His gait was unsteady and ataxic, with a tendency to fall to the right, consistent with cerebellar affection. Sensibility, motor skills and reflexes were otherwise normal. All vital parameters were normal, and examination of the heart, lungs and abdomen yielded no findings. Exploratory blood tests were normal, including leukocytes, CRP and sedimentation rate. Borrelia serology was repeated and was unchanged, testing positive for IgM antibodies and negative for IgG antibodies.
As a result of the gradual onset of symptoms with a sub-acute course and improvement of symptoms during steroid treatment, possible differential diagnoses in the first assessment were primarily inflammatory, infectious or expansive conditions. Neuroborreliosis was regarded as less probable in light of the serology and lack of effect from doxycycline. Cerebral computed tomography (CT) is a rapid, readily available examination for detecting pathology requiring immediate action, such as a tumour with pronounced swelling.
A CT scan of the head without contrast was taken immediately after admission and showed low-attenuation changes in frontal white matter in the right cerebral hemisphere (Fig. 1) and in the right cerebellar hemisphere. Supplementary magnetic resonance tomography of the brain and medulla the following day revealed multiple lesions in the brain stem, cerebellum and both cerebral hemispheres (Fig. 2). The neuroradiologist regarded the findings as consistent with multiple metastases, cerebral tuberculosis, a parasitic disease or septic emboli with secondary abscess formation. Cerebrospinal fluid analysis revealed a leukocyte level of 9 · 109/l, but otherwise normal values for erythrocytes, glucose and protein. The same evening, CT scans of the thorax, abdomen and pelvis were carried out to look for signs of extracerebral disease, including cancer, bacterial infection focus, tuberculosis in or outside the lungs, or signs of a parasitic disease. They revealed multiple micronodules in the lungs, most in the apical parts of both upper lobes, one slightly larger nodule in the apical lateral segment of in the left upper lobe and a small high-attenuation lesion to the right of the entry of the right main bronchus, consistent with a calcified lymph node (Fig. 3). There were multiple low-attenuation lesions in the abdomen and pelvis, most of them in the upper part of the liver, and in addition lesions in the kidneys and prostate. The radiologist described the findings as most consistent with miliary tuberculosis.

Figure 1 CT head without contrast medium showing low-attenuation changes in frontal white matter in the right cerebral hemisphere (star).
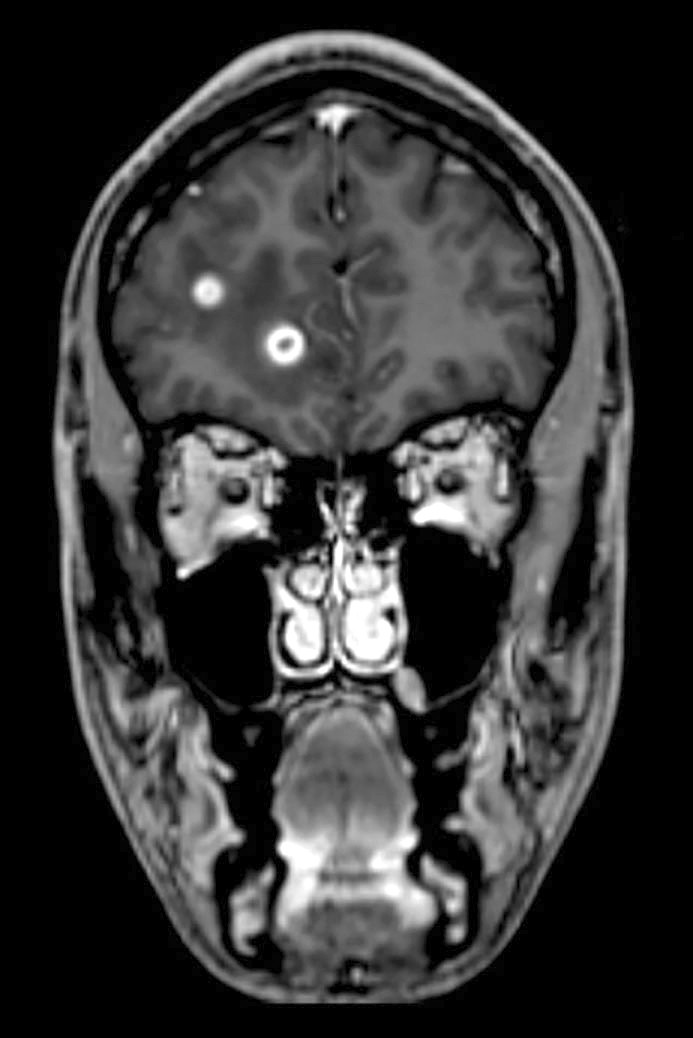
Figure 2 T1-weighted volumetric magnetic resonance tomography of brain and medulla, taken with contrast medium. The image shows multiple lesions in the cerebral hemisphere.
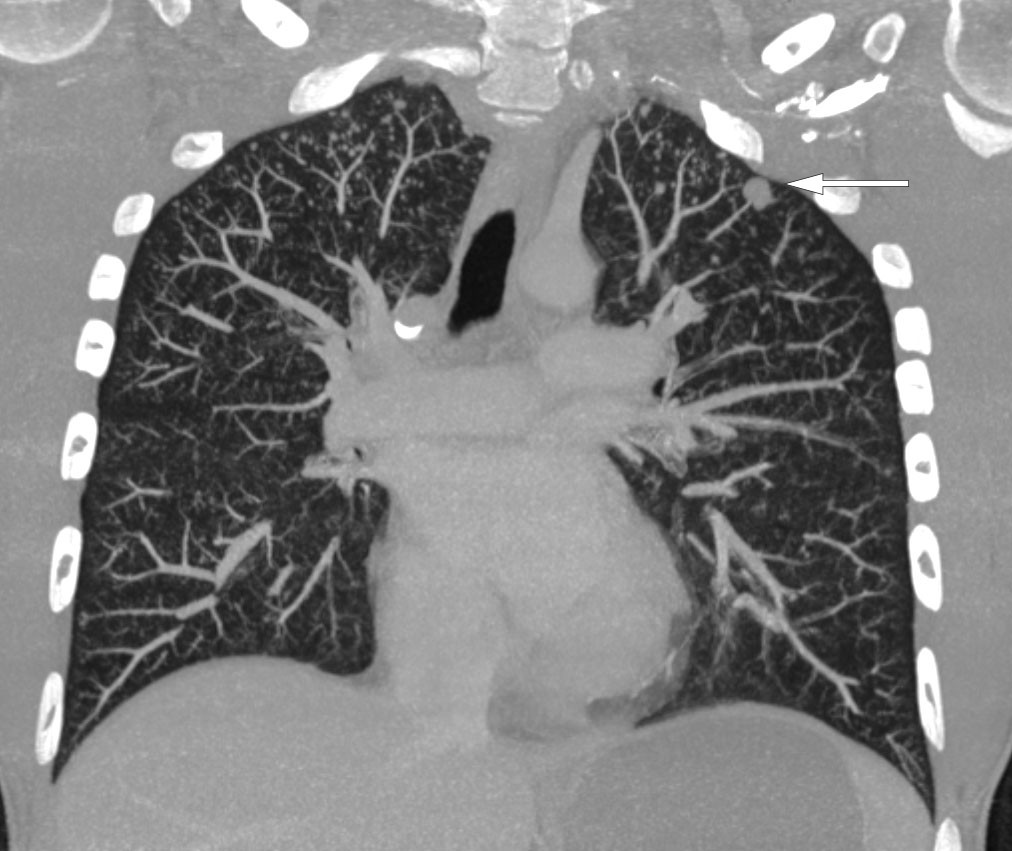
Figure 3 CT thorax taken after injection of intravenous contrast medium. The image shows multiple micronodules in the tops of both lungs and a 9 mm nodule apically and laterally in the left upper lobe (arrow).
Tuberculosis bacteria spread by means of airborne infection. If the body’s immune system does not fight the infection, a granuloma or tubercle will form in the lungs through an inflammatory process. This is called a primary focus. A primary focus with associated tuberculosis-infected hilar glands forms a primary complex. From here, the bacteria can be transmitted by way of the blood. In most cases, the immune system will prevent further spreading, but the bacteria can also survive for a long time. The condition is then called latent tuberculosis, which by definition does not cause symptoms. In patients with otherwise sound immune systems, 90–95 % of those who become infected will only have latent tuberculosis, while 5–10 % will develop active disease. Among those with active disease, most will develop pulmonary tuberculosis, while about a quarter to a third will develop extrapulmonary tuberculosis. In cases of disseminated or miliary tuberculosis, the infection may spread through the blood to all parts of the body. Our patient had lesions in the central nervous system, lungs, liver, kidneys and prostate, which could be consistent with haematogenous spread of tuberculosis.
Owing to suspicion of potentially infectious tuberculosis, the patient was moved to airborne infection isolation in the Infection Control Section. A closer examination of the patient’s clinical history revealed some weight loss and night sweats recently, but no cough, laboured breathing or sense of fever. The patient stated that he had spent 2–3 months in his parents’ home country in Southeast Asia six months prior to the onset of symptoms. He had been given BCG vaccine as a child. As a further stage of the tuberculosis diagnostics, repeated tests were conducted on saline-induced expectorate and bronchial lavage water from bronchoscopy and urine and stool were cultured for mycobacteria. Although there was still no definite evidence of tuberculosis, antitubercular treatment was started after the bronchoscopy, with intravenous rifampicin and isoniazid, pyrazinamide and ethambutol orally at doses as recommended in the tuberculosis guidelines (1). We initially chose to add high-dose moxifloxacin 800 mg x 1, with a view to improving penetration to the central nervous system. In addition to the antitubercular treatment, he was started on dexamethasone 12 mg x 1 to suppress the brain swelling.
Ordinary tubercular treatment is divided into an intensive phase with rifampicin, isoniazid, pyrazinamide and ethambutol for two months and then a continuation phase with rifampicin and isoniazid for four months (1). For tuberculosis of the central nervous system, particularly for tubercular meningitis, the continuation phase is usually extended, so that the total treatment time is 12 months. Isoniazid penetrates freely to the cerebrospinal fluid and has a strong bactericidal effect throughout the course of the treatment (2). Rifampicin has poor penetration to the cerebrospinal fluid, but has a potent antitubercular effect, and is regarded as a cornerstone in the treatment of all tuberculosis, also of the central nervous system (3). Pyrazinamide readily penetrates the blood-brain barrier, while ethambutol’s penetration of this barrier is poor.
Direct microscopy did not detect acid-fast bacilli in cerebrospinal fluid, induced sputum or bronchial lavage water. Polymerase chain reaction testing (PCR) for the tuberculosis complex was negative in the same samples. However, tuberculosis was strongly suspected, and tissue biopsies were indicated to directly detect mycobacteria. A lung or prostate biopsy was regarded as safer than a kidney and especially a brain biopsy. Direct microscopy of a transurethral biopsy from the prostate and a CT-guided transthoracic lung biopsy yielded negative findings. Four days after sampling, PCR of prostate tissue revealed DNA from mycobacteria belonging to the tuberculosis complex. The sample additionally tested positive for mutation of the rpoB gene.
The tuberculosis diagnosis was confirmed by the PCR finding in the prostate tissue. Mutations of the rpoB gene are a marker of rifampicin resistance. When rifampicin resistance is detected, there is an over 90 % probability of isoniazid co-resistance. If the bacterium is resistant to both these primary agents, multi-resistant tuberculosis is present by definition. Multi-resistant tuberculosis is associated with a poorer prognosis and higher mortality. The condition requires long-term treatment with drugs, with a higher risk of serious side effects, and treatment is centralised at regional hospital level.
With reservations for the fact that the PCR method had not been validated for the sample material in question, we had to allow for the possibility of multi-resistant tuberculosis. As recommended in the tuberculosis guidelines, we switched to a frequently chosen empirical combination treatment for suspected multi-resistant tuberculosis: moxifloxacin, pyrazinamide, amikacin, cycloserine and protionamide. We also chose to retain isoniazid in the regimen until any resistance was confirmed. The patient had already been receiving treatment for just on a week and was feeling better. Nonetheless, there was a possibility that this could be ascribed to the effect of pyrazinamide and systemic steroids. After two weeks of treatment he was still unsteady, but had almost no abducens or facial palsy.
Resistance to tuberculosis drugs, particularly multi-resistant tuberculosis (4), but also monoresistance to isoniazid (2), is associated with increased mortality as a result of tubercular meningitis. The reserve medicines used against multi-resistant tuberculosis have many side effects. Our patient developed neuropsychiatric symptoms a week into his treatment, but recovered after cycloserine was discontinued.
Four weeks into the treatment for suspected multi-resistant tuberculosis, tuberculosis bacteria grew on a prostate tissue sample. Somewhat surprisingly, repeat PCR revealed no mutation of the rpoB gene. Resistance assays conducted by the Norwegian Institute of Public Health revealed phenotypic sensitivity to all primary agents. No mutation was found in rpoB and no markers for isoniazid resistance.
Once multi-resistant tuberculosis had been ruled out, first-line treatment was resumed. Because of the severity of the disease and extensive central nervous system spreading, we chose to retain moxifloxacin supplement through the intensive phase, even though there is no good documentation for making this choice in cases of tuberculosis sensitive to primary agents. The patient then received continuation therapy with rifampicin and isoniazid for a total of 12 months. After six weeks, the patient left the hospital to go home. There was total regression of cranial nerve deficits at the time of his departure, but his gait was still somewhat unsteady. Growth of mycobacteria was not found in other samples taken from the bronchi, and we regarded the patient as non-infection-bearing. Nor was there growth in the urine, stool or cerebrospinal fluid cultures. If multi-resistant tuberculosis had been detected, the patient would normally have been isolated until three culture samples were negative.
Discussion
This case report illustrates a rare, but life-threatening manifestation of tuberculosis. The combination of clinical examination, recording of the patient’s history of illness, radiological examinations and epidemiological thought process raised suspicion of tuberculosis of the central nervous system. The patient’s symptoms of headache, dizziness and double vision, and the clinical findings in the form of cranial nerve deficits and ataxia were due to tuberculomas in the brain stem and cerebellum. This condition is rare in Norway, but occurs more often in patients who have originated from or spent time in a high endemic country.
Since direct microscopy has low sensitivity and growth of mycobacteria can take up to six weeks, it is often necessary in serious cases to start treatment before the tuberculosis diagnosis is confirmed. PCR may be useful for detecting tuberculosis bacteria in the event of negative microscopy, and can also provide information about sensitivity to antibiotics through genotypic resistance assays. If a mutation indicating resistance to rifampicin is detected, a high probability of co-resistance to isoniazid must be assumed. The combination of resistance to both rifampicin and isoniazid defines multi-resistant tuberculosis, which requires very prolonged and potentially toxic treatment. The PCR method for detecting resistance has not been validated for use directly on sample material. In this case it led to the patient receiving unnecessary treatment with reserve medicines that cause side effects. We chose nonetheless to carry out this examination, because in cases of lesions in the central nervous system it is important to get answers as fast as possible, as the correct therapy is life-saving. Phenotypic resistance assays have higher sensitivity and specificity, and also yield resistance results for more drugs. Our patient was therefore able to revert to first-line drugs when the test ruled out multi-resistant tuberculosis.
When extra-pulmonary tuberculosis is suspected, it is important to secure sample material, and biopsies from several locations may be necessary to increase diagnostic accuracy. The diagnostics of brain biopsies are demanding and entail a risk of serious complications. As tuberculosis of the brain is an expression of lymphohaematogenous dissemination of mycobacteria, it is important to investigate whether there is extracranial disease. About three quarters of patients with tuberculosis of the central nervous system have extracranial lesions which may be more readily accessible for diagnostics (5). Our patient had lesions in the lungs, kidneys, liver and prostate, and sampling from these organs entailed less risk than a brain biopsy. After negative tests from both bronchial secretion, urine and stool as well as from a CT-guided biopsy of lung changes, it was a prostate biopsy that finally confirmed the diagnosis.
Clinical history and findings illustrate important points in the diagnostics of tuberculosis. There is every reason to be on the watch for this old, but still equally relevant disease.