A woman in her sixties developed symptomatic soft-tissue swelling and fluid accumulation six months after a blunt trauma to her right hip. The swelling recurred despite repeated aspirations and surgical excision. MRI eventually provided the correct diagnosis.
A woman in her sixties was received by a hospital trauma team after being struck on her right side by a falling tree. An initial examination revealed displacement of the upper right arm and pain in the right side of the body. X-ray showed a compound fracture of the humerus. The fracture was stabilised with a plaster cast and the patient transferred to the orthopaedic department of a university hospital. There she underwent osteosynthesis with good results. Radiographic healing was confirmed after three months.
At six-month follow-up, the patient complained of pain and swelling in her right hip. Pelvic MRI showed a subcutaneous, well-defined, encapsulated, fluid-filled locule. This was deemed to be a possible earlier haematoma not requiring further intervention.
A month later, the patient was re-examined as an outpatient owing to persistent discomfort and swelling in her right hip. Palpation revealed a soft-tissue swelling over the greater trochanter, and 60 ml of bloody serous fluid was aspirated from the swelling under sterile conditions. Following recurrence, a further 30 ml was aspirated eight days later. One ml of corticosteroid was injected.
Eleven months after the trauma, the patient experienced another recurrence, and pelvic MRI revealed an unchanged subcutaneous locule. The radiologist suspected a Morel-Lavallée lesion (Figure 1). It was decided to perform an elective open excision of the locule, including the capsule, with primary suturing in the operating theatre. One week after the excision, the patient experienced another recurrence. A further aspiration was performed and compression attempted in the outpatient clinic, but without success.
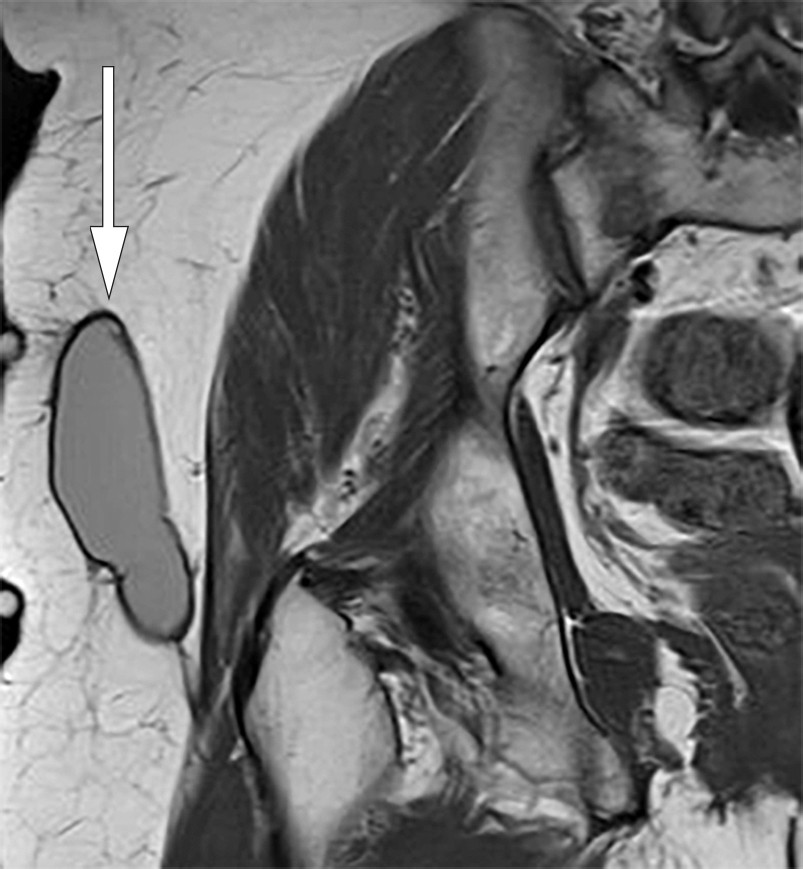
Figure 1 Coronal T1-weighted MRI of right hip. Well-defined, elongated, lenticular structure with homogeneous intermediate signal located over the deep fascia.
A chronic Morel-Lavallée lesion was diagnosed, and sclerotherapy with doxycycline (1) was decided upon. In the outpatient clinic, the old haematoma was evacuated under sterile conditions using two cannulae, and 25 ml doxycycline 20 mg/ml was instilled. The patient was rotated every ten minutes – three times in total – to distribute the antibiotic fluid, which was then aspirated. Temporary compression was applied with bandages until the patient acquired her own compression garments in the form of tight cycling shorts with extra padding over the lesion. These were used continuously for four weeks.
No recurrence was seen at four-week follow-up. The patient felt only mild discomfort in the area and was able to discontinue compression. At 12-week follow-up, MRI of the right hip showed almost full regression of the lesion (Figure 2). At one-year follow up, the patient showed no clinical or radiographic evidence of disease, but with sequelae in the form of mild skin contraction.
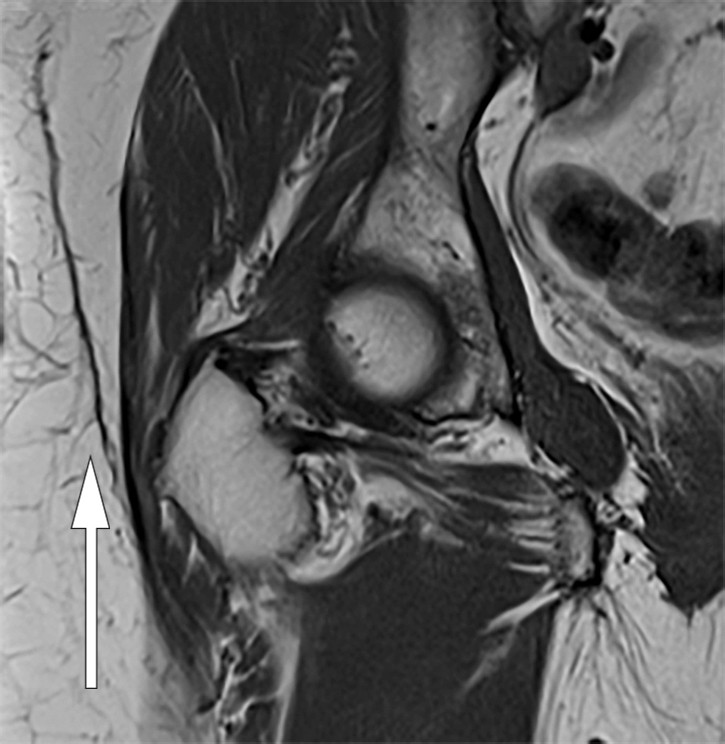
Figure 2 Coronal T1-weighted MRI of right hip. Minor residual changes after previous fluid-filled locule.
Discussion
The Morel-Lavallée lesion was first described by French surgeon François Morel-Lavallée in 1863 (2). The lesion is often seen in trauma patients and is usually caused by a blunt injury in which large tangential forces displace subcutaneous adipose tissue and the superficial fascia from the underlying deep fascia. This causes damage to the perforating arteries, veins and lymph vessels, which in turn leads to accumulation of bloody fluid in the interfascial plane (3). The damage is often overlooked upon initial contact with trauma units owing to larger and more obvious injuries. The peritrochanteric region is the most common site of Morel-Lavallée lesions because of its prominence and large surface area, skin mobility and the rich capillary network in the soft tissue (4). Diagnosis is made on the basis of medical history, clinical examination and MRI.
MRI is the gold standard for description and diagnosis of a Morel-Lavallée lesion, and the condition is classified into six types on the basis of appearance on MRI (5). Ultrasound can be used in the acute phase and where MRI is not available. Non-specific fluid accumulations with heterogeneous echogenicity are seen in the acute phase. The lesion is usually compressible and without flow on Doppler imaging. Chronic lesions tend to be more homogeneous with capsule formation (3, 6, 7).
Morel-Lavallée lesions are often overlooked initially, which can lead to a complicated course. Had our patient received the correct diagnosis after her first MRI, she might have been spared four aspirations and a surgical excision. It is therefore important to consider this type of injury during tertiary review of trauma patients.
The following treatment algorithms have been proposed for Morel-Lavallée lesions (8): First, a distinction must be made between acute and chronic lesions, and between conditions with and without infection and/or fracture. Acute lesions can be treated using compression. If this proves unsuccessful, percutaneous drainage is recommended with or without sclerotherapy, combined with compression. In cases of infection or fracture, open debridement, vacuum-assisted wound closure (9) and secondary suturing are advised. Chronic lesions should be treated initially with percutaneous drainage, sclerotherapy and compression. Tetracyclines should be considered first-line agents for sclerotherapy owing to a number of advantages: they are cheap and easy to obtain, have few adverse effects, and have an antibacterial effect that may prevent infection (10). If no improvement is seen, debridement, primary suturing and compression are recommended, plus repeated sclerotherapy if appropriate. In the event of continued treatment failure, open debridement, vacuum-assisted wound closure and secondary suturing should be performed.
The importance of compression for achieving a good result must be emphasised. This is illustrated by our patient, in whom lack of compression in association with the initial treatment is thought to have contributed to rapid recurrence.