Abdominal pain is a frequent reason for referral of children to paediatric and surgical specialist health care. Acute appendicitis, constipation and gastroesophageal reflux are among the most common diagnoses. Children often have diffuse symptoms, and although “common things are common,” it is important to be aware of symptoms that suggest serious underlying pathology. Close collaboration between general practitioners, paediatricians, paediatric surgeons and radiologists can be important for achieving a successful outcome.
A girl in her early teens, who had suffered from a ‘sluggish bowel’ since early childhood, had over the last five years been experiencing brief episodes of nausea and abdominal pain relieved by vomiting, often in the evening and at night. Her first contact with the specialist health service was a referral by a private specialist for assessment in Acute Admissions for suspected subileus/acute abdomen. Over the past few weeks, the episodes of abdominal pain and vomiting had become more frequent, and she was reluctant to eat because food intake triggered or exacerbated the pain. She had lost approximately 4 kg over the course of 1–2 months. There was no haematemesis, diarrhoea or melaena. That same day, abdominal ultrasound at a private radiology clinic had shown normal findings, while an abdominal x-ray was described as showing constipation with no signs of ileus.
Her pain had decreased from a score of 10 on the visual analogue scale to a score of 2–3 by the time she arrived in Acute Admissions. The paediatrician and surgeon decided that acute hospitalisation was not required, but an appointment was scheduled for examination by a paediatrician in 14 days’ time. The patient had two close relatives with migraine, and abdominal migraine was therefore considered a differential diagnosis. Gastroesophageal reflux was considered unlikely because of the episodic nature of the symptoms. Constipation and secondary abdominal pain were also relevant differential diagnoses, but while signs of constipation had been described on the abdominal x-ray, these findings were not consistent with clinical findings. She now had daily soft stools after having been started on macrogol (Movicol) by her general practitioner (GP) a few weeks earlier. Blood samples were taken to screen for coeliac disease, hypothyroidism, inflammatory bowel disease, iron deficiency anaemia and malabsorption prior to the scheduled outpatient appointment.
Constipation with no known organic cause (functional constipation) is a common cause of abdominal pain, with a reported prevalence of 0.7–12 % in Europe (1). Hard, lumpy stools less than twice a week in children over four years of age, simultaneous constipation and diarrhoea, and encopresis may indicate constipation (1, 2). In our department, ultrasound measurement of rectal diameter is performed in children aged 4–12 years, for whom reference ranges for rectal diameter are available. A transverse rectal diameter of more than 3 cm may indicate constipation (2). This test is performed only at the request of a paediatrician on the basis of clinical suspicion, and not as part of a standard abdominal ultrasound. Abdominal x-ray cannot be used to confirm or rule out constipation owing to a lack of association between constipation and the amount of stool visible on x-ray, poor inter-observer reproducibility, as well as the risk of overlooking other causes of abdominal pain such as appendicitis, volvulus and intussusception (1). Pronounced nausea and vomiting are not included in the Rome IV diagnostic criteria for constipation (1), and one should therefore look for other causes of persistent nausea and vomiting.
At the outpatient appointment two weeks after first contact, the patient had gained a little weight and had less abdominal pain. Clinical examination showed normal findings. Blood tests were normal, including negative transglutaminase and deamidated gliadin, normal levels of thyroid stimulating hormone (TSH)/thyroxine (T4), a negative genetic test for lactose intolerance, normal levels of calprotectin, vitamin B12, ferritin and folate, and a negative antigen test for Helicobacter pylori.
Gastroesophageal reflux (possibly secondary to constipation), constipation, and abdominal migraine were still considered relevant differential diagnoses. The patient continued on macrogol for suspected constipation, and it was decided to try esomeprazole (Nexium) 40 mg daily in addition. It was agreed that the mother would report back by telephone after four weeks, and an outpatient appointment was scheduled for four months’ time.
Gastroesophageal reflux, possibly secondary to constipation, is another frequent cause of abdominal pain in children. In a study of 10 394 French children (0–17 years), it was estimated that 6.2 % had gastroesophageal reflux (3, 4). A thorough patient history and clinical examination is considered adequate diagnostic testing for young children in whom no complications are suspected, and most children stop showing symptoms by 2–3 years of age (5). One standard diagnostic test that should be performed before any drug treatment is initiated, is 24-hour pH testing of the lower oesophagus; gastroscopy with biopsy can also be performed to detect oesophagitis. X-ray of the oesophagus, stomach and duodenum (an upper gastrointestinal series) is not well-suited to detecting reflux or oesophagitis, but can be used to detect anatomical anomalies such as a hiatus hernia, stricture or gastric outlet obstruction, e.g. due to malrotation (5). Our patient had not yet undergone any of these tests.
Shortly before her scheduled outpatient appointment four months later, the girl was acutely hospitalised with abdominal pain and vomiting. She had vomited almost every day for 17 days, with a single major episode of vomiting every afternoon/evening which provided immediate symptomatic relief. There were no definite observations of blood or bile in the vomit. Her weight had decreased by 5.5 kg in the course of six months, but was still within the normal range for her age. Over the last two weeks the patient and her parents had been in contact with Accident and Emergency (A&E) and their GP twice, and the GP had consulted the Paediatric Department by telephone. Nexium had been discontinued in A&E, but reinstated by the GP. The patient had been taking macrogol for several months and still had normal/soft stools every 1–2 days. Blood tests performed by the GP a few days prior to hospitalisation had revealed no signs of severe dehydration, but the girl’s symptoms persisted and her mother felt that she was very weak with poor general condition.
On the day of hospitalisation, haemoglobin (Hb) was 17.2 (10.9–14.6) measured by the GP, and she was considered moderately dehydrated. Blood tests on arrival showed several abnormal results: Hb 16.5 g/dl (10.9–14.6), haematocrit 0.48 (0.33–0.43), erythrocytes 5.7 · 1012/l (3.9–4.9), monocytes 0.99 · 109/l (0.3–0.7), sodium 136 mmol/l (138–145), potassium 2.6 mmol/l (3.6–4.7), chloride 82 mmol/l (97–107), ionised calcium 1.08 mmol/l (1.14–1.32), and creatinine 80 μmol/l (37–73). Venous blood gas showed pH 7.45 (7.35–7.45), base excess (BE) 15.2 mmol/l (-3.0–+3.0), pCO2 7.8 kPa (4.7–5.9), pO2 5.0 kPa (11.0–14.4), and HCO3 40.2 mmol/l (22.0–26.0), i.e. a compensated hypochloremic metabolic alkalosis, which would be consistent with prolonged vomiting. The patient reported pain upon deep palpation of the epigastrium, but little pain otherwise. Other clinical examinations showed normal findings. Stools were soft without visible blood or mucus, and she had not vomited since arriving at the hospital.
Such a pronounced and acute exacerbation was not consistent with previously considered diagnoses such as abdominal migraine, gastroesophageal reflux and constipation; gastric retention and superior mesenteric artery syndrome were therefore considered as alternative differential diagnoses. Upon admission, treatment was started with erythromycin (Ery-Max) suspension 3 mg/kg to stimulate gastric emptying, intravenous NaCl and glucose solution with added sodium and potassium, and potassium suspension 10 ml x 3 orally. Abdominal ultrasound was performed on Friday evening by a specialty registrar in radiology, who described a whirl sign in the epigastrium involving the superior mesenteric artery and vein (Figure 1). The doctor suspected intestinal malrotation and recommended, in the first instance, a confirmatory ultrasound by an experienced paediatric radiologist in daytime hours. An acute angle was also noted between the aorta and the proximal portion of the superior mesenteric artery, consistent with possible superior mesenteric artery syndrome. Abdominal x-ray showed normal findings.

Figure 1 Ultrasound. Whirl sign involving vessels and the small intestine in the epigastrium.
The girl was kept under observation throughout the weekend. Her general condition had improved, and she had little abdominal pain and no episodes of vomiting. Her electrolyte levels quickly normalised following initiation of fluid therapy. On Monday morning, an ultrasound examination was performed by an experienced paediatric radiologist who confirmed the whirl sign (Figures 1 and 2) and who suspected concomitant volvulus (where a loop of intestine twists about its own axis). The diagnosis was confirmed by an upper gastrointestinal series, which showed passage of contrast to the proximal small intestine, but no further (Figure 3). The transition between the duodenum and small intestine was just to the left of the midline, caudal to the level of the duodenal bulb, which suggested malrotation with volvulus. The explanation for the patient’s long-term symptoms had finally been found (Figure 4).

Figure 2 Ultrasound. Whirl sign involving mesenteric vessels and loops of small intestine. The superior mesenteric artery (red Doppler signal) is to the right of the superior mesenteric vein (blue Doppler signal).

Figure 3 Upper gastrointestinal series (x-ray of oesophagus, stomach and duodenum). Contrast can be seen in the stomach and scattered throughout the duodenum, which has a typical ‘corkscrew’ appearance, with absence of contrast filling in the jejunum. The duodenum also has atypical positioning; normally the duodenum is further up and to the left of the midline than seen here.
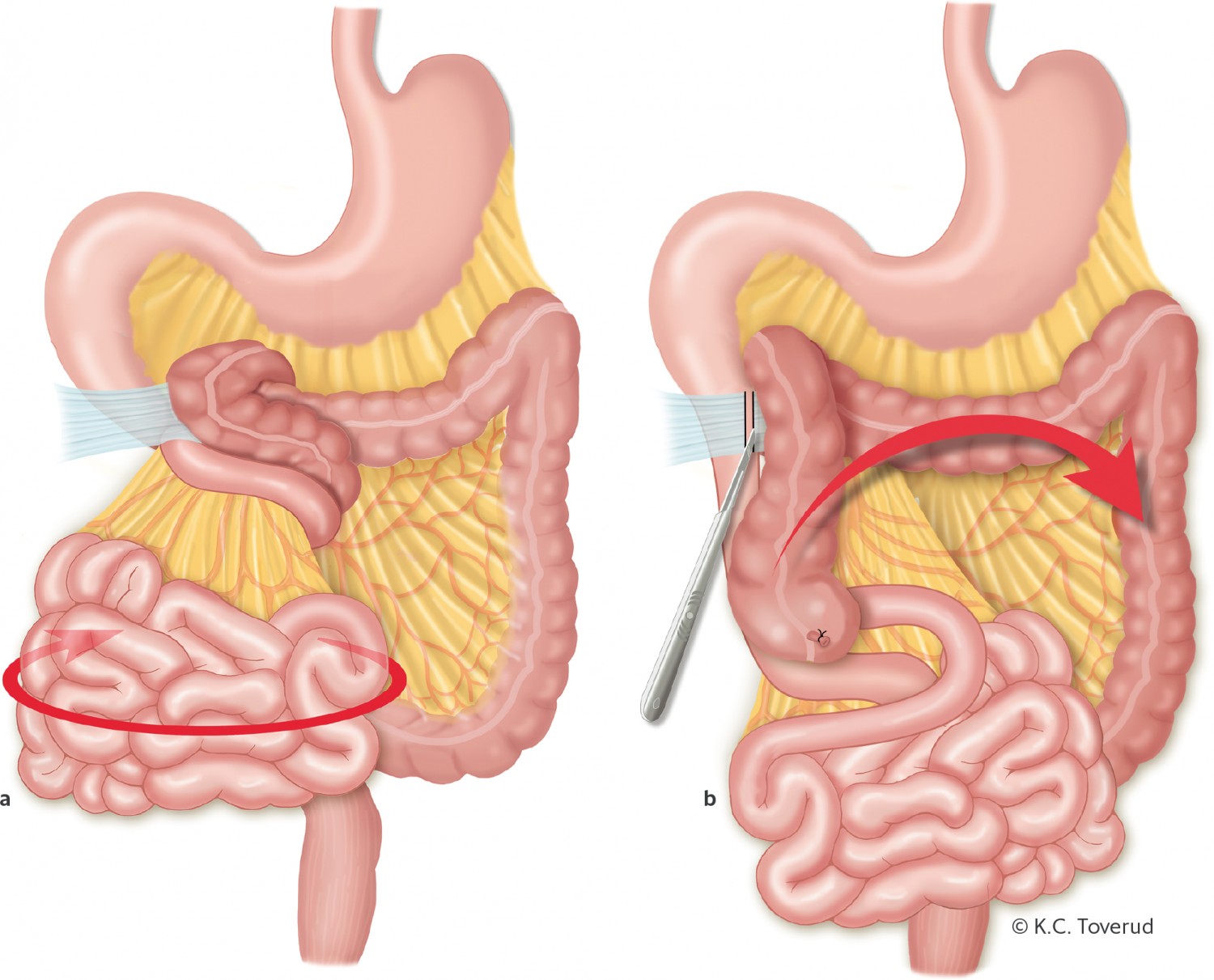
Figure 4 a) Midgut volvulus due to congenital malrotation and duodenal obstruction due to congenital Ladd’s bands. Volvulus can be corrected by rotating the midgut counter-clockwise (‘turn back the time’). b) Ladd’s procedure entails dividing Ladd’s bands between the posterior abdominal wall, duodenum and colon. The mesentery is then widened by dividing the bands between the duodenum and the colon using blunt and sharp dissection. The appendix is removed to prevent misdiagnosis in the event of future appendicitis, as the caecal pole will be on the left side of the abdominal cavity following the procedure. After the procedure, the large intestine is on the left side of the abdominal cavity, and the duodenum and small intestine are on the right side (non-rotated positioning).
Malrotation occurs during gestational weeks 4–12. It affects the positioning of the duodenum from the opening of the common bile duct up to and including the first two-thirds of the transverse colon, and involves varying degrees of short mesentery and proximal, obstructive fibrous bands (Ladd’s bands) (6). Malrotation may have a range of symptoms or none at all. In the absence of volvulus, symptoms may include bilious vomiting, abdominal pain, or appendicitis with abnormal localisation. In cases of malrotation with concomitant volvulus and altered blood flow to the gut, there may additionally be bloody stools and peritonitis. With partial or intermittent volvulus, there may be protein-losing enteropathy, poor growth, malnutrition and occult gastrointestinal bleeding (6). The classic presentation of malrotation in neonates or infants is bilious vomiting, and children with bilious vomiting should be assumed to have malrotation until proven otherwise (6). Abdominal symptoms and radiological findings in a child with malrotation and volvulus may be subtle and non-specific, despite the highly serious and potentially life-threatening nature of the underlying condition. As the midgut becomes ischaemic, the patient may develop melaena, irritability, pain, abdominal distension or peritonitis; in the worst-case scenario, bowel necrosis may result in septic shock and death (6). Early diagnosis and treatment is essential to avoid ischaemia of the bowel with serious consequences for the child.
Upon ultrasound examination, the superior mesenteric vein can usually be seen to the right of the superior mesenteric artery. If the vein is to the left or in front of the artery, this should raise strong suspicion of malrotation. Sensitivity is reported to be 67–100 % and specificity 83–92 % (7). If abnormal positioning is detected with ultrasound, an upper gastrointestinal series should then be performed. In our patient, ultrasound revealed the ‘whirl sign’, which is considered 100 % specific for midgut volvulus (7): the duodenum, the proximal portion of the small intestine, and the superior mesenteric vein twist around the superior mesenteric artery. The underlying cause is malrotation and a short mesentery. Midgut volvulus gives rise to a duodenal – i.e. proximal – obstruction, and abdominal x-ray may thus be completely normal, despite the child having an acute condition in need of surgical intervention.
When volvulus is present, an upper gastrointestinal series will show an obstruction, often with a ‘corkscrew’ appearance of the duodenum and a lack of contrast filling beyond this point. Water-soluble contrast should be used for x-rays when volvulus is suspected, as bowel resection may be required with the associated risk of intraoperative contrast extravasation.
The patient was transferred from the local hospital to a university hospital, for acute surgery in the paediatric surgery department. A laparotomy revealed malrotation with volvulus, with a 720º rotation of the midgut. Detorsion of the midgut was performed, and no evidence of strangulation of the intestines was seen. Ladd’s procedure was then carried out. This entails widening the mesentery to prevent future volvulus, and arranging the intestines in a non-rotated position with the duodenum and small intestine on the right side of the abdominal cavity, and the ileocaecal junction in the upper left quadrant. The colon is positioned in the left half of the abdominal cavity. Appendectomy is usually performed, as in our patient, to avoid a future atypical appendicitis.
The postoperative course was uncomplicated and, according to the patient’s mother, the girl has been completely symptom-free in the first year since the surgery.
Discussion
This case report illustrates the challenges of diagnosing children with abdominal pain and vomiting. Most cases of symptomatic malrotation and concomitant volvulus are discovered in early childhood before the age of two years (6). It is much rarer for the condition to be seen at 12 years of age, as in this patient (6). The symptoms were intermittent and the abdominal pain varied greatly in intensity. This is typical for this age group, but made diagnosis challenging (6).
Doppler ultrasound, with can reveal the whirl sign, is a very useful diagnostic tool in trained hands (3) and is often the first imaging examination the child undergoes. An upper gastrointestinal series is the gold standard for diagnosing malrotation and should always be performed as an emergency procedure when malrotation is suspected – even if the ultrasound is negative (6, 7). Although radiology specialisation includes training in paediatric ultrasound, one cannot expect everyone to be able to recognise an unexpected volvulus on ultrasound. Few of those in non-paediatric specialties will ever see it. However, clinicians and radiologists alike should pay particular attention to babies/children with bilious vomiting, in whom malrotation and volvulus must always be suspected. There may initially be subtle abdominal symptoms, and it is usually only late in the disease course that the baby develops bloody stools and peritonitis (6). By then irreversible ischaemic damage to the midgut may already have occurred. Prompt, accurate diagnosis and subsequent surgery to correct malrotation can, however, result in a successful outcome for this potentially life-threatening condition.