Persistent symptoms of dizziness may be due to inappropriate compensatory strategies following an episode of acute dizziness. Common symptoms are dizziness in an upright position that is aggravated by visual stimuli and passive movement. In the World Health Organization’s new disease classification, ICD-11, the condition has been named persistent postural-perceptual dizziness. It is important to recognise this condition in order to avoid unnecessary investigation and to initiate the correct treatment.
Persistent symptoms of dizziness may be due to inappropriate compensatory strategies following an episode of acute dizziness. Common symptoms are dizziness in an upright position that is aggravated by visual stimuli and passive movement. In the World Health Organization’s new disease classification, ICD-11, the condition has been named persistent postural-perceptual dizziness. It is important to recognise this condition to avoid unnecessary investigation and to initiate the correct treatment.
Persistent functional dizziness has been known for many years under various names, including phobic postural vertigo, visual vertigo and chronic subjective dizziness. In response to an initiative by the Bárány Society, these terms have recently been grouped together under the umbrella term ‘persistent postural-perceptual dizziness’ and have been given their own diagnostic criteria (1). The condition is characterised by dizziness that is exacerbated by an upright posture and by complex visual stimuli, together with a sensation of falling without demonstrable unsteadiness or other abnormal neurological findings. The onset of symptoms often follows an episode of acute dizziness with different aetiology, such as vestibular neuritis, and are probably due to inappropriate compensatory strategies (2). Most patients benefit from information and rehabilitation exercises (3), and it is important to be aware of the condition to spare the patient prolonged suffering and unnecessary radiological assessment.
Here we provide a brief introduction to the pathophysiology, diagnosis and treatment of this condition, based on a literature review and our own experience.
A typical case history
A woman in her forties developed, over the course of a few hours, dizziness with accompanying head pressure and difficulty understanding what was being said to her. She was hospitalised and received a diagnosis of vestibular neuritis. After a brief improvement, she deteriorated and developed impaired balance and vision, nausea, fatigue and cognitive difficulties. She became nauseated whenever she looked at things while she or they were in motion. She was examined by an otorhinolaryngologist and a neurologist, neither of whom found anything abnormal.
After about six months of sick leave, she was examined by another neurologist. She described feeling as though someone had put a vacuum cleaner under her feet and sucked out all of her strength. She felt she had received little information or understanding from her doctor during her sick leave, and she wondered whether her symptoms were typical of inflammation of the vestibular nerve. The neurologist diagnosed chronic subjective dizziness and initiated vestibular rehabilitation.
After a month, she felt much better and moved more steadily and quickly, but she was still on partial sick leave and struggled with ‘brain fog’, fatigue, mental blanks and forgetfulness. After spending time at work, she would need to return home to sleep. Due to her own concern over her cognitive function she was referred to a neuropsychologist, who found no impairment. After a few more months, she was able to begin working full-time.
Pathophysiology
The human balance system consists of sensory input from the eyes, proprioceptive system and vestibular system that is interpreted and coordinated by the central nervous system, in particular the brainstem and cerebellum. Whenever we walk, move our head and/or look at something that is in motion, vestibulo-ocular and spinal reflexes work together to help us keep our balance. Damage or disruption of this complex interplay usually results only in transient problems with balance. This is because compensatory mechanisms, along with changes in the weighting of the various sensory inputs, serve to reduce any functional impairment (4). In the event of unilateral vestibular failure, for example, visual and proprioceptive inputs are assigned greater weight. Key structures in the vestibular nuclei and cerebellum also become more sensitive to input from the healthy contralateral vestibular apparatus (5).
The normal reaction to acute dizziness is to activate motion control strategies by leaning on something for support or by using the eyes to focus on fixed points.
The pathophysiological processes underlying persistent postural-perceptual dizziness are not fully understood, but the condition may be attributable to increased attention to postural and visual control after the acute symptoms have subsided. If the patient continues to lean on objects for support or to use their eyes to focus on fixed points while in motion, this may prevent recalibration of the balance system and trigger a vicious cycle with cautious and stiff gait, myalgia, anxiety and avoidance behaviours. Somatosensory information on body position may be reinforced and distorted, leading to dizziness. Many also become tired and have difficulty concentrating because they are expending energy on what was previously automatic (Figure 1) (2, 6).
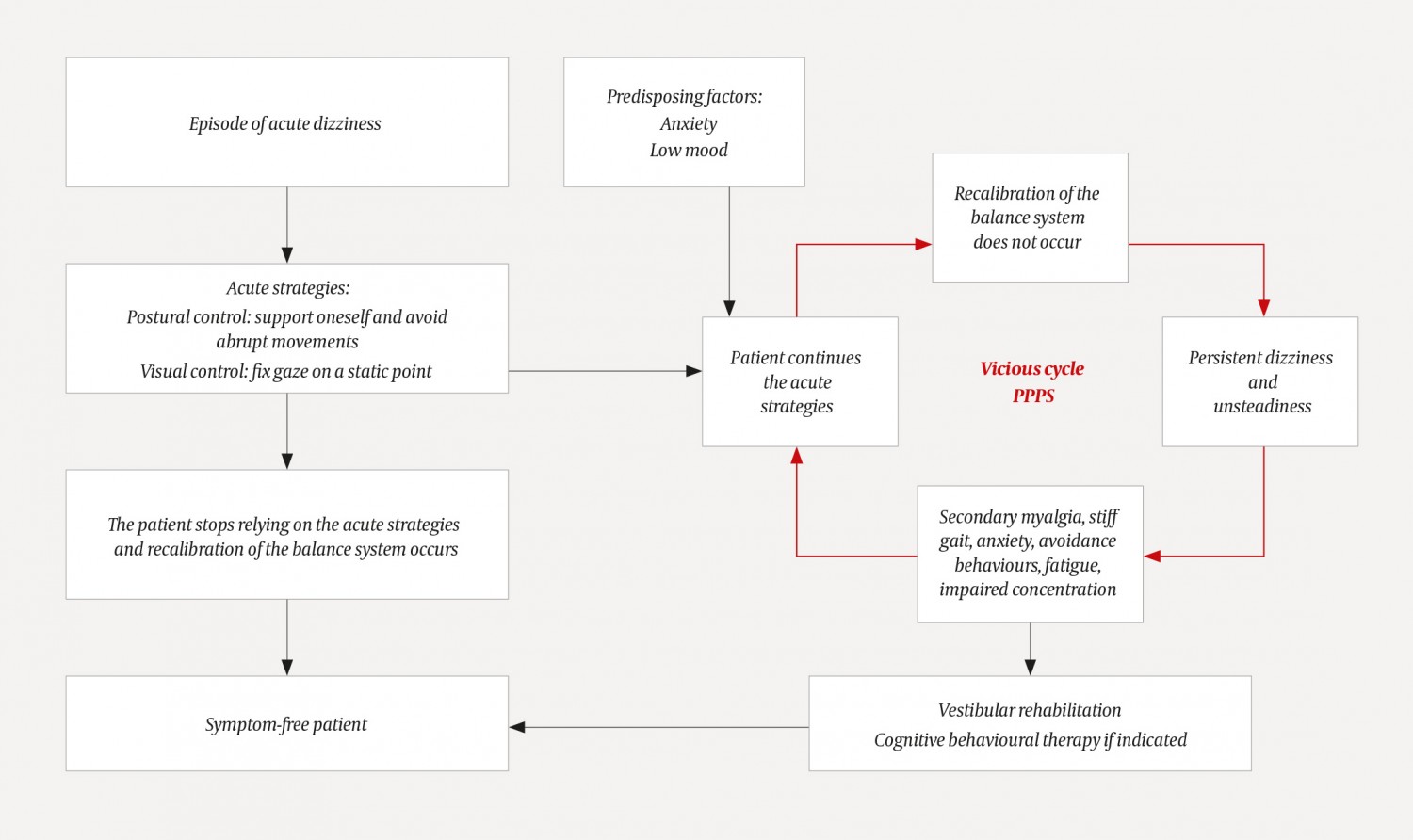
Figure 1 Putative mechanisms underlying normal and maladaptive physiological responses to acute dizziness, adapted from Popkirov et al. (6). PPPD = persistent postural-perceptual dizziness.
Diagnostics
Persistent postural-perceptual dizziness is diagnosed on the basis of a typical medical history (Box 1) (1). The dizziness, which the patient may describe in various ways, is exacerbated by an upright posture, by active or passive motion of the body, and in surroundings with complex or moving visual stimuli, such as shopping centres. The patient often reports a precipitating acute episode of dizziness. In 25 % of patients, this is due to vestibular neuritis, benign paroxysmal positional vertigo (BPPV) or vestibular migraine (1). The symptoms may also arise after mild head trauma or anxiety attacks (2). The patient feels unsteady, but a clinical neurological examination is usually normal. Some have vestibular findings due to the precipitating disorder or a comorbid condition, such as a pathological head impulse test, unilateral spontaneous nystagmus, positional nystagmus, a pathological caloric test, saccades upon ophthalmological examination, and veering or falling towards the impaired side while standing or marching with the eyes closed (Unterberger’s/Fukada’s test) (7).
Box 1 Diagnostic criteria for persistent postural-perceptual dizziness. All criteria must be fulfilled (1).
One or more symptoms of dizziness, unsteadiness, or non‐spinning vertigo are present on most days for 3 months or more.
Symptoms are persistent, but wax and wane.
Symptoms may not be active throughout the entire day.
Symptoms are present without specific provocation, but are exacerbated by:
Upright posture,
Active or passive motion without regard to direction or position, and
Exposure to moving visual stimuli or complex visual patterns.
The condition usually begins shortly after an event that causes dizziness, unsteadiness or problems with balance. Precipitating events include acute, episodic or chronic vestibular syndromes, other neurological or medical illnesses and psychological distress.
When triggered by an acute or episodic precipitant, symptoms typically settle into the pattern of criterion A.
When triggered by a chronic precipitant, symptoms may develop slowly and worsen gradually.
Symptoms cause significant distress or functional impairment.
Symptoms are not better attributed to another disease or disorder.
Differential diagnoses and comorbidity
Relevant differential diagnoses include other vestibular syndromes (bilateral vestibulopathy, mal de debarquement syndrome, benign paroxysmal positional vertigo, Ménière’s disease), neurological disorders (migraine, cerebellar degeneration, parkinsonism, cerebral small vessel disease, orthostatic tremor), adverse effects of medications, orthostatic hypotension, vestibular schwannoma, coronary heart disease, deficiency diseases (including vitamin B12 or iron deficiency) and anxiety disorder (8).
Treatment
In our experience the following points are key:
Respect. It is important to acknowledge that the patient’s symptoms and functional impairments are genuine.
Reflection. Talk to the patient about his or her symptoms and their effects on everyday life, as well as his or her thoughts on the underlying cause and on the future
Reattribution and rehabilitation. Name the condition and explain to the patient that it is well-known, common and potentially treatable. Explain the background (Figure 1) and emphasise that persistent postural-perceptual dizziness is not a diagnosis of exclusion, but rather has its own diagnostic criteria. The condition must not be confused with social anxiety, but may be exacerbated by psychological mechanisms (9).
Vestibular rehabilitation
There is substantial evidence that vestibular rehabilitation is effective in cases of vestibular injury or dysfunction (3, 10), but responses may vary depending on the aetiology (11).
Vestibular rehabilitation is an exercise-based treatment consisting of eye, head and body movements designed to stimulate and optimise vestibular compensation. The goal is to reduce the experience of dizziness and imbalance by re-establishing effective and automatic eye-head coordination, reducing anxiety and self-monitoring, increasing fitness, boosting confidence and learning to live with dizziness. The treatment is suitable for anyone who can perform a daily low-intensity exercise programme for 6–12 weeks. Many patients can do this independently. Others require follow-up by a physiotherapist.
The exercises used to promote recovery begin cautiously and slowly increase in intensity. The exercises consist of head movements (bending backwards and forwards, tilting from shoulder to shoulder and turning to the sides, with eyes open and closed, at rest and while moving the body), eye movements (keeping the eyes fixed in different directions while moving the body), rolling the body from side to side in a lying position, bending the head towards the floor in a sitting position, standing up from a lying position, standing with the legs together, standing on one leg, standing heel-to-toe, and walking in a circle on an uneven surface, combined with head and eye fixation exercises (12).
Some patients may benefit from cognitive behavioural therapy in addition to vestibular rehabilitation (3).
Antiemetic drugs, betahistine and drugs for travel sickness have no place in vestibular rehabilitation, but may instead delay recovery. Such medications should only be used for a brief period in the acute phase of vestibular neuritis to relieve symptoms and increase physical activity (13).
