Radiofrequency turbinoplasty is a well-established technique for treating nasal obstruction caused by inferior turbinate hyperplasia. It should preferably be used after medical treatment has been attempted. We describe two patients who developed osteomyelitis after radiofrequency turbinoplasty.
Patient 1
A woman in her forties underwent combined septoplasty and radiofrequency turbinoplasty under general anaesthesia. Local anaesthesia was administered using tetracaine with adrenaline on tampons, plus infiltration of the nasal mucosa with lidocaine 1 % (Xylocaine) with adrenaline. Two insertion channels were made in the right inferior turbinate and three in the left, and septal splints were used for a week after surgery.
At the one-week follow-up, abundant crusting was noted in the nasal cavity. The septal plates were removed along with the crusting, and the patient was given guidance on increased saline irrigation of the nasal cavity.
Nineteen days after the operation, she contacted the otorhinolaryngology department and complained of an unpleasant smell in her nose. Nasal endoscopy revealed extensive crusting, and the inferior turbinate showed necrosis and bone loss. Chronic osteomyelitis was suspected with local spread of bacteria from a post-surgical infection (1, 2).
Bone biopsies were taken from the inferior turbinate for pathological examination and bacterial culture. The patient was hospitalised and treatment was initiated with cloxacillin 2 g × 4 intravenously (3). Bilateral resection of the posterior two-thirds of the inferior turbinate was performed under general anaesthesia.
The pathologist described the condition as ‘chronic inflammation and necrosis consistent with osteomyelitis’ (Figure 1). Bacteriological culture showed growth of Streptococcus pneumoniae, Moraxella catarrhalis and mixed anaerobic flora. The bacteria were sensitive to erythromycin and metronidazole, and cloxacillin was therefore replaced with a ten-day course of peroral erythromycin and metronidazole.
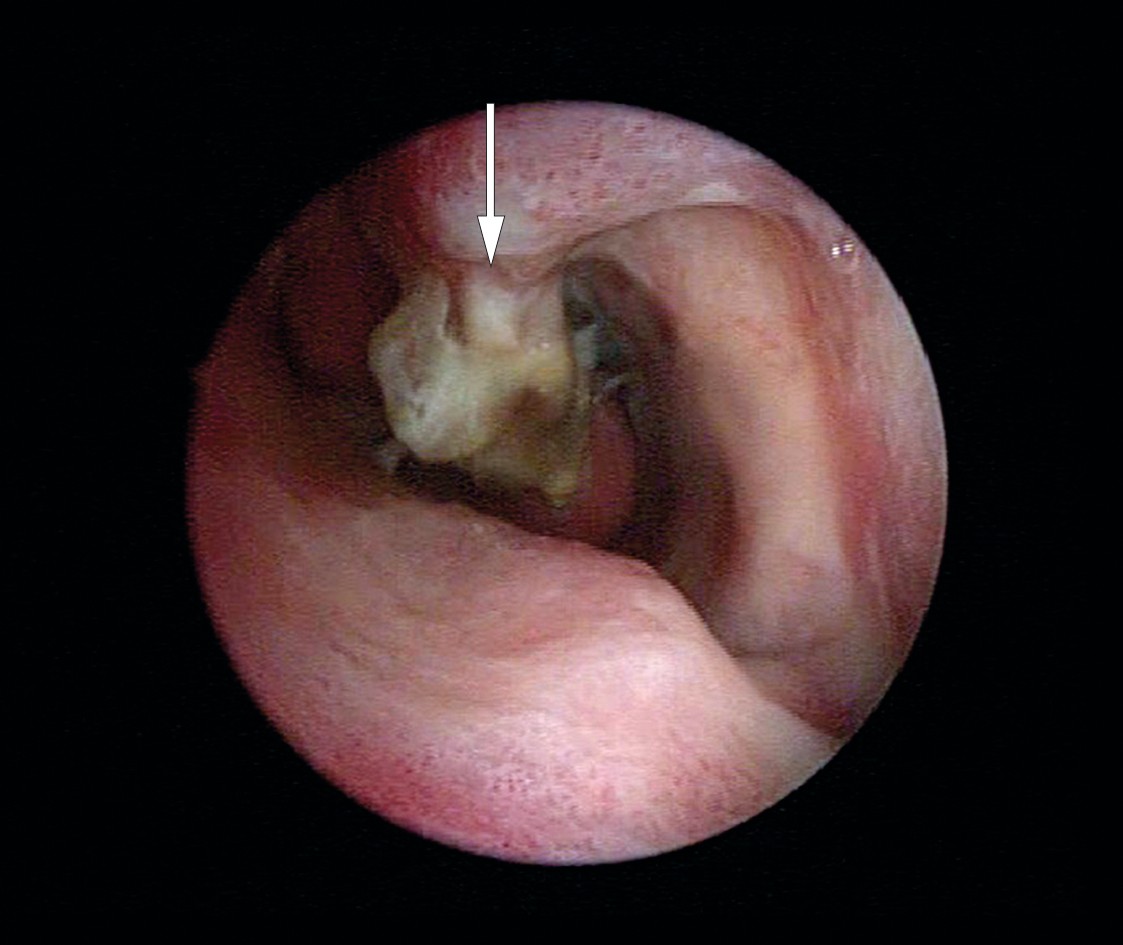
Figure 1 Patient 1 at the time of diagnosis of osteomyelitis. The image shows a pus-covered and necrotic inferior turbinate (marked with an arrow). The nasal septum can be seen lower left.
Patient 2
A man in his thirties underwent radiofrequency turbinoplasty as described in patient 1, but with three insertion channels bilaterally.
The man had normal postoperative status after one week, and saline irrigation and nasal use of sesame oil were recommended. He also resumed regular use of budesonide (Rhinocort).
The patient contacted his general practitioner 15 days after surgery owing to a bad smell and pus in his nose. The general practitioner prescribed a 7-day course of doxycycline tablets (the patient had a penicillin allergy). Due to lack of improvement, the patient was referred back to the otorhinolaryngology department 45 days after surgery.
Nasal endoscopy revealed similar findings to those in patient 1, and biopsies were taken of the inferior turbinate. Bilateral excision of the posterior two-thirds of the inferior turbinate was performed under general anaesthesia. Due to the penicillin allergy, treatment was started with erythromycin and metronidazole rather than cloxacillin. The pathologist described this patient’s condition too as ‘chronic inflammation and necrosis consistent with osteomyelitis’. Bacterial culture showed growth of Pseudomonas aeruginosa, Corynebacterium diphtheroides, anaerobes, Staphylococcus aureus and alpha-haemolytic streptococci. The bacteria were sensitive to ciprofloxacin and metronidazole, and the treatment was changed to a two-week course of these drugs in tablet form.
Both patients had values for leukocytes, sedimentation rate and CRP within reference ranges throughout the disease course. They were in good general condition without fever or signs of systemic infection. In addition to the above treatment, the patients were instructed to apply ointment containing hydrocortisone and oxytetracycline (Terra-Cortril) to the inferior turbinates twice a week and to irrigate the nose with saline daily. They were followed up with frequent outpatient appointments.
Both patients have made a good recovery. Patient 1 has an open nose with functioning mucosa-lined residual tissue in the bilateral inferior turbinate.
Patient 2 has developed ‘empty nose syndrome’ (4) on the right side, with subjective nasal congestion but an objectively clear nasal passage. His left side is functioning well.
Discussion
To the best of our knowledge, there are no previously published descriptions of osteomyelitis in the inferior turbinate after radiofrequency turbinoplasty. There are, however, articles describing infections after the procedure, which may of course include osteomyelitis (5).
Any surgical procedure carries an infection risk, and one should be alert to increased crusting, altered smell, and to pain and fever. Patient 1 experienced only an unpleasant smell in her nose. In retrospect, she should have had a follow-up appointment shortly after the first postoperative check. This may have made it possible to detect the infection earlier and possibly prevent the development of osteomyelitis. Patient 2 should ideally have been referred to the otorhinolaryngology department when he contacted his general practitioner.
Radiofrequency turbinoplasty has been described as preferable to cryosurgery (6). However, a Cochrane review found that existing studies were of insufficient quality to allow a preferred modality to be recommended (7). The review notes that severe complications are rare after turbinoplasty, with bleeding and dry nose the most common problems. The distributor of the surgical equipment used on our patients recommends only a single insertion channel, but this often poses anatomical challenges and we usually use two insertion channels. This increase in the number of insertion channels may have been responsible for the osteomyelitis, as it results in increased trauma and thus an increased risk of tissue necrosis. The distributor further recommends tetracaine as surface anaesthesia and infiltration with lidocaine 1 %. We used tetracaine with adrenaline as surface anaesthesia and infiltration with lidocaine 1 % with adrenaline, as this reduces bleeding during the procedure. It is possible that the adrenaline, as a result of its vasoconstrictive properties (8), may have contributed to the development of osteomyelitis.
Osteomyelitis is defined as infection and inflammation of the bone. It can occur as a result of haematogenous spread or contiguous spread of a soft tissue infection to the bone, or by direct inoculation of the bone in connection with trauma or surgery. Haematogenous osteomyelitis is usually monobacterial, whereas osteomyelitis in cases of bacterial inoculation or spread from adjacent tissues is usually polybacterial. Correct diagnosis and treatment requires bone biopsies and microbiological culture (9).
Our patients probably had osteomyelitis resulting from contiguous spread of infection. Their infections were chronic and polymicrobial and required surgical debridement in addition to antibiotics. We followed Norwegian guidelines for antibiotic use before adjusting the treatment in response to microbiological test results.
