An elderly man sustained a cervical spinal cord injury after a fall down the stairs. The rehabilitation process was delayed by repeated infections with few clinical signs. Spinal cord injury also disrupts the innervation of internal organs, which may lead to atypical manifestations of acute illnesses.
A man in his seventies with ankylosing spondylitis, type 2 diabetes and coronary artery disease was admitted to the surgical department of a local hospital after a fall on the stairs. Upon arrival in Acute Admissions, he was conscious and oriented but lacked motor responses in his upper and lower extremities. His airway was unobstructed, heart rate was regular and normal, and blood pressure was 80/60 mm Hg. CT of the head, neck, thorax, abdomen and pelvis in line with the trauma protocol showed a cervical fracture at level C4–C5. After the CT scan, the patient became unresponsive. Blood gas measurement showed respiratory acidosis, and hypoventilation was suspected. The patient was immediately intubated. Supplementary CT of the head with angiography showed no sign of traumatic bleeding, but rather cessation of circulation in both vertebral arteries with retrograde filling of the posterior cerebral artery, consistent with dislocation of the vertebral arteries as a consequence of the cervical fracture. The man was transferred to the neurosurgical department of the nearest regional hospital where he underwent emergency surgery with repositioning of the cervical fracture and osteosynthesis. Brain MRI after surgery showed restoration of circulation in the vertebral arteries without cerebral infarction. Spinal cord MRI showed spinal cord oedema at level C2–C5 consistent with a spinal cord injury (Figure 1).
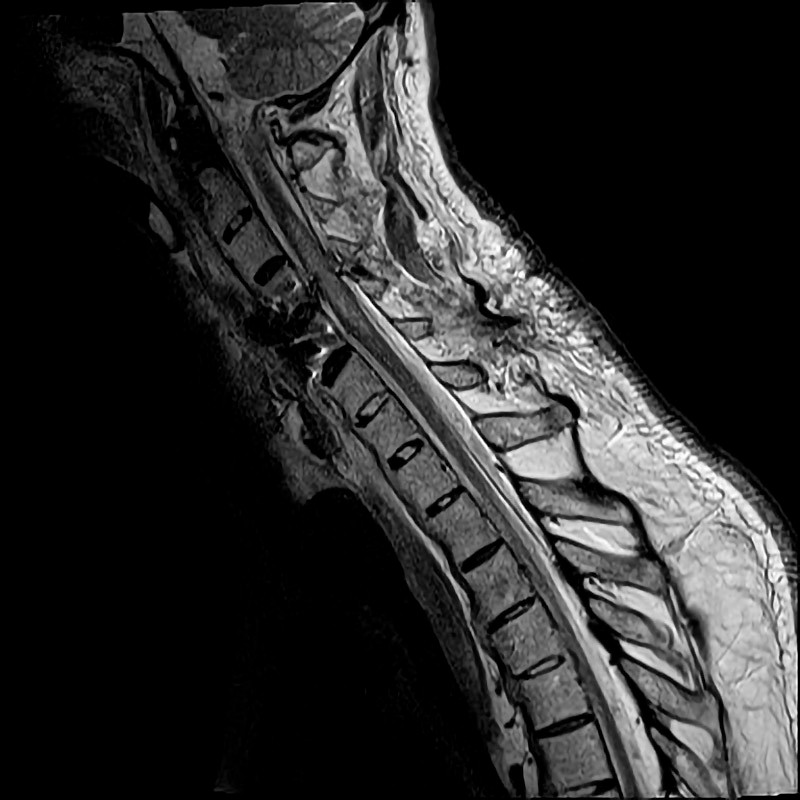
Figure 1 MRI of the cervical spine after surgical fixation at the C4–C5 level. Centromedullary injury can be seen at levels C3–C6.
In Norway, 50–100 people suffer a traumatic spinal cord injury each year (1). Falls among the elderly appear to be driving an increase in the number of traumatic spinal cord injuries (2). High (cervical) spinal cord injuries can be life-threatening. Damage to innervation of the diaphragm (C3–C5) and the intercostal muscles (Th1–Th11) will result in acute respiratory failure. Neurogenic shock with sudden loss of sympathetic stimulation from level Th1–L2 of the spinal cord can give rise to circulatory failure as a result of vasodilation and bradycardia. If the injury involves the sympathetic innervation of the heart, which originates from Th1–Th5, there is a risk of cardiac arrest and arrhythmias (3).
Upon awakening from anaesthesia, the patient showed intact cognition. He had undergone a tracheostomy, as it was thought that respiratory support would be required for an extended period, as well as treatment with a cough assist device. He was hypotensive and required a vasopressor (noradrenaline infusion 0.13 mg/kg/min) to maintain normal mean arterial pressure (MAP). His heart rate was normal with nocturnal bradycardia. Due to general weakness, he required parenteral nutrition even though his swallowing function was intact. He had urinary retention, was insensitive to bladder filling and required a permanent urinary catheter. Over the course of 14 days and after gradual tapering of the noradrenaline infusion, his mean arterial pressure stabilised above 60 mm Hg. However, due to ongoing pronounced orthostatism, he was placed on regular antihypotensive medication (etilefrine 10 mg × 3 peroral). He needed intermittent respiratory support via the tracheostomy. Nausea, vomiting and increasing abdominal distension were noted at this point, and CT abdomen was performed due to suspected paralytic ileus. The images showed no signs of ileus, but did reveal gallstones without cholecystitis, which was regarded as an incidental finding. Two weeks after the injury, the patient’s condition was considered stable and he was transferred to the neurological department.
Clinical examination of the spinal cord injury was performed using the American Spinal Injury Association (ASIA) Impairment Scale (4); the spinal cord injury was described as incomplete with quadriplegia, but partially intact sensation, and with neurological level of injury C2. Spinal cord injury also entails damage to the autonomic nervous system. Common sequelae are hypotension and orthostatism, bradycardia, respiratory failure, impaired intestinal motility with constipation, and urinary tract dysfunction (5). Autonomic dysfunction should be classified during rehabilitation, preferably using a standardised form. Spinal shock gives rise to transient areflexia that can last for hours, days or weeks following the injury, and which is gradually replaced by the hyperreflexia and spasticity expected after an injury to the central nervous system (5). Spinal cord oedema after trauma may result in the injury level appearing higher in the acute phase than is actually the case, and ASIA Impairment Scale classification should be repeated during the rehabilitation period.
Shortly after his transfer to the neurological department, he became febrile with reduced general condition and increased neuropathic pain. Clinical examination of the heart and lungs was normal, but his abdomen was still distended and meteoristic. Oxygen saturation fell spontaneously from 98–99 % to 87–92 % with unchanged respiratory support. CRP was 115 mg/l (reference range < 5 mg/l), and leukocytes were normal at 8.1 ∙ 109/l (4.0–11.0 ∙ 109/l). Dipstick testing of a sample from the permanent urinary catheter was 2+ for leukocytes; the sample was sent for culture. The skin showed no sign of infected pressure ulcers, and inspection of the surgical wound revealed no sign of infection. When CRP increased to over 200 mg/l, it was decided to initiate broad spectrum antibiotics (piperacillin/tazobactam 4 g/0.5 g × 3 intravenous) against suspected aspiration pneumonia. Chest x-ray confirmed an infiltrate suggestive of pneumonia and effusion over the right hemi-diaphragm. Antibiotic treatment for 10 days produced clinical improvement and normalised the patient’s body temperature, oxygen saturation and CRP. Microbiological culture of the urine sample was negative.
Infections after a spinal cord injury have historically given rise to serious complications, and sepsis as a result of respiratory, urinary tract or pressure ulcer infections still contributes to increased mortality in the chronic phase of spinal cord injury (6). Inefficient cough means that respiratory tract infections may have few symptoms, while secretion stagnation increases the risk of infection. Patients are predisposed to urinary tract dysfunction with difficulty in emptying the bladder, probable reflux to the upper urinary tract and the need for a urinary catheter. Immobilisation and impaired sensation increase the risk of pressure ulcers.
Four weeks after the injury, the patient became febrile again with reduced general condition. The physiotherapist noted a marked increase in spasticity in all extremities. Earlier that day, a temporary percutaneous endoscopic gastrostomy (PEG) tube had been inserted to supplement nutritional intake given the patient’s weakness. Clinical examination of the heart, lungs and abdomen revealed no change, and the skin around the PEG insertion site was unremarkable. Preliminary blood tests showed CRP 109 mg/l and leukocytes within the reference range. It was thought that the CRP increase could potentially be attributable to the surgery. However, blood tests 24 hours later showed that CRP had increased to 173 mg/l, with leukocytes 10.0 ∙ 109/l and neutrophilic granulocytes 8.3 ∙ 109/l (1.6–8.3 ∙ 109/l). Chest x-ray was normal. Dipstick testing of a sample from the urinary catheter was slightly positive for leukocytes and the sample was again sent for culture. An infectious disease specialist was consulted, who examined the patient and noted the distended abdomen with possible metallic bowel sounds and slight tenderness in the upper left quadrant. In the absence of other clinical signs – and in light of the recent surgical intervention – an abdominal infection focus was considered a possibility, such as an abscess, ileus or bowel perforation. CT abdomen was performed, which again showed no ileus or other pathology, only gallstones in the absence of cholecystitis. Further blood tests showed that CRP had increased to 215 mg/l and leukocytes to 11.4 ∙ 109/l; neutrophilic granulocytes, ALT, AST, GGT and creatinine were all within reference ranges. As it was difficult to identify a definite infection focus, it was decided to initiate broad spectrum antibiotic treatment (piperacillin/tazobactam at the same dose as for the previous infection). This led to rapid normalisation of body temperature and infection parameters. The treatment was continued for a total of 14 days. Microbiological cultures of blood and of urine from the permanent catheter were negative. The tracheal secretion was positive for Staphylococcus aureus, but this was considered to be without clinical significance.
The patient reported mild abdominal tenderness. In our experience, it is difficult to predict the degree of preserved visceral sensation in internal organs following a spinal cord injury. Up to 80 % of patients with spinal cord injuries have sequelae that include constipation and defecation difficulties (7), which can make it difficult to determine whether abdominal symptoms reflect a new-onset disease. Our patient noted increasing spasticity and neuropathic pain during the infection. Symptoms such as these, with spontaneous exacerbation of known sequelae, are not uncommon in cases of intercurrent disease.
Two months post-injury, the patient became febrile once again. Examination revealed that he was not oriented to time, but he had no neck stiffness and his respiratory and circulatory status were unchanged. Blood tests showed CRP 91 mg/l, leukocytes 10.3 ∙ 109/l and neutrophilic granulocytes 7.5 ∙ 109/l. Dipstick testing from the urinary catheter was positive for leukocytes, nitrite and blood, and peroral antibiotic treatment was started for a presumed urinary tract infection (trimethoprim-sulfamethoxazole 160 mg/800 mg × 2). Blood tests the following day showed rapidly increasing CRP of 219–261 mg/l. Examination of the heart, lungs, and abdomen again showed normal findings apart from distension and diffuse tenderness of the abdomen. However, there was no focal tenderness, guarding or costovertebral angle tenderness. Suspecting an upper urinary tract infection, it was decided to switch to intravenous antibiotic treatment (cefotaxime 2 g × 3). A chest x-ray was performed to rule out another case of pneumonia, and showed normal findings. The next day the patient became increasingly delirious with deteriorating general condition. Vital signs were unchanged. CRP increased to 328 mg/l, leukocytes to 13 ∙ 109/l and neutrophilic granulocytes to 10.4 ∙ 109/l. ALP, AST, GGT and creatinine were within reference ranges, whereas bilirubin was slightly elevated at 23 µmol/l (< 19 µmol/l). He complained of burning pain in all extremities. His bowel movements had been slower than usual, and he had visible abdominal distension, but examination of the abdomen showed no further changes. Following discussion with other specialists, we decided to request immediate examination by a surgeon owing to suspected acute abdomen. The surgeon on duty noted abdominal distension and slight tenderness under the right ribcage upon deep palpation, but no clinical signs of peritonitis. Clinical signs were thus fairly sparse, but the patient was referred for CT abdomen on suspicion of an abdominal infection focus, in particular in the bile ducts. CT showed gallstones and a thickened gallbladder wall consistent with cholecystitis (Figure 2). Treatment of the cholecystitis was initiated with intravenous piperacillin/tazobactam and percutaneous drainage via a biliary drainage catheter, which revealed yellow pus. The treatment produced rapid improvement in clinical symptoms and laboratory parameters.

Figure 2 CT abdomen showing distended gallbladder with marked thickening of the wall, a focal response in surrounding adipose tissue as well as concrements in the gallbladder and bile duct.
Abdominal ultrasound would normally be the primary choice for targeted investigation of gallstones and cholecystitis. The fact that CT abdomen was chosen instead as the primary examination method suggests an unclear clinical picture and the need to simultaneously rule out multiple conditions with rapid diagnostic imaging.
The patient experienced two recurrences of cholecystitis, both times shortly after discontinuation of antibiotics and drainage. At no point did he experience spontaneous abdominal pain. It was noted that he had complained of pain in his right shoulder during the cholecystitis. This was interpreted at the time as musculoskeletal pain, neuropathic pain or spasticity, but in retrospect may have been referred pain from the gallbladder.
The patient underwent cholecystectomy after the third recurrence, despite the risks associated with surgery given his general condition. The operation was successful. The patient remained free of infection long-term and could engage fully with planned rehabilitation. He was using a sip-and-puff wheelchair when he was discharged to his own home a few months later.
Discussion
This case illustrates the challenges associated with diagnosing acute disease in a patient with a spinal cord injury. Our patient had multiple infections with sparse clinical signs and symptoms. When he developed cholecystitis, his symptoms were atypical and differed little from those of his previous infections.
Retrospective studies show that symptoms of acute abdomen in patients with spinal cord injuries vary from classical (pain in the upper right quadrant) to atypical (8–10). Examples of atypical symptoms in cases of acute abdomen include reduced general condition, general malaise, increased spasticity and neuropathic pain (8–10). Referred pain, such as back and shoulder pain in cases of cholecystitis, has also been described in patients with spinal cord injuries (8). Autonomic dysreflexia is a phenomenon associated with high spinal cord injuries, in which sensory stimulation below the level of the injury leads to intense sympathetic activation with hypertension, intense headache, paradoxical sweating and agitation (3). The commonest cause of autonomic dysreflexia is urinary retention, but it has also been reported as an early symptom of acute abdomen (9). Acalculous cholecystitis, a rare and serious form of cholecystitis in the absence of gallstones that most often affects patients in intensive care, has also been described in a case study of seven patients with spinal cord injuries, none of whom had typical symptoms (10).
The prevalence of gallstones appears to be increased in patients with spinal cord injury. Studies show a prevalence of 17–31 %, which is higher than in able-bodied persons (11, 12). Risk factors for gallstone formation in the acute phase of spinal cord injury include long-term parenteral nutrition, immobilisation and rapid weight loss with muscle atrophy. In the chronic phase of spinal cord injury, there is an increased incidence of diabetes (probably due to muscle atrophy with increased body fat percentage (13)), which is a known risk factor for gallstones. In common with other abdominal organs, the gallbladder receives complex autonomic innervation. Ultrasound and scintigraphy studies in patients with spinal cord injury show normal emptying of the gallbladder (mainly under parasympathetic control by the vagus nerve), but changes to the relaxation phase (mainly under sympathetic control) (14–16); it is thus conceivable that altered gallbladder storage leads to increased risk of gallstone formation. A recent study showed an increased incidence of cholecystitis following spinal cord injury independent of previously diagnosed gallstones (17). This suggests that other factors may also contribute to acute cholecystitis in patients with spinal cord injuries, although the evidence is currently sparse. Gallstones were detected in our patient as an incidental finding only two weeks after his spinal cord injury, and he also had known risk factors in the form of advanced age and diabetes. We consider it likely that our patient had gallstones prior to his spinal cord injury. With an increased incidence of gallstone disease in this patient group, and the challenges associated with diagnosing acute disease, there is much to be learned from this patient’s medical history.
Complications after spinal cord injuries have historically resulted in high morbidity and mortality. Doctors in many disciplines will encounter the spinal cord injured patient.
In our opinion, doctors should be vigilant and adopt a low threshold for extensive blood testing and diagnostic imaging if a serious illness is suspected. It is important to take into account autonomic dysfunction and reduced visceral sensation. Any changes noted by the patient should be viewed as significant.
