Malignant melanoma is a serious and growing health problem. What do we know about it, and what do we only think we know?
Since the Cancer Registry of Norway was established in 1953, the incidence of malignant melanoma has increased eleven-fold (1) and the mortality rate has increased five-fold (2) (Figures 1 and 2). The increase in incidence can be attributed partly to overdiagnosis, but we have no good explanation for the large increase in mortality. There is an apparent consensus that sunlight is the main cause of malignant melanoma (3). However, malignant melanoma is no more common on those areas of the body that are most exposed to the sun than on areas that are usually covered by clothing (4). Exceptions are the rare lentigo maligna melanomas, which have a good prognosis (5), and desmoplastic melanomas (6), which, in common with the relatively harmless keratinocyte carcinomas, are seen only on skin that has sustained high levels of sun exposure. We have no evidence that people are becoming more sunburned now than in the past.
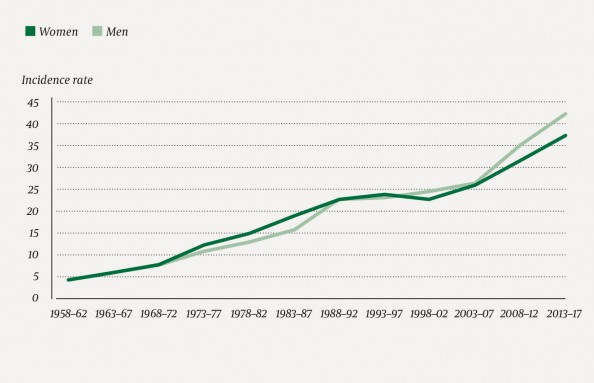
Figure 1 Age-standardised incidence rate for malignant melanoma per 100 000 persons.

Figure 2 Annual deaths caused by malignant melanoma in Norway in the period 1969–2012.
Multiple risk factors
There has been no increase in UV radiation in Norway (7), and it seems reasonable to assume that people have always sunbathed when given the opportunity, just as they do today. It has been suggested that sunburn in connection with sun-seeking holidays might have caused the increase in melanoma, but the majority of such trips are to Spain, which has few cases of malignant melanoma (8). Moreover, a Norwegian study of sun exposure habits in 2018 (9) showed that most of those who reported sunburn had become sunburned in Norway. Skin type, number of moles and genetic factors are established risk factors for malignant melanoma (10). Observational studies provide conflicting data on whether sun exposure causes malignant melanoma, as living at lower latitudes (e.g. Australia versus the British Isles, and the USA versus Canada) somewhat increases the risk of malignant melanoma, whereas having an outdoor occupation seems to reduce the risk (10). Sunburn may be an indicator that a person rarely sunbathes, but does so to excess whenever they do. Exposing your body to large amounts of sun for a few days seems to be more dangerous than daily exposure (3). A Norwegian-Swedish prospective study showed a slight increase in melanoma incidence after repeated cases of sunburn. The main risk factors in the study were red hair and a large number of asymmetrical moles larger than 5 mm (11).
Role of UV radiation
Sun exposure can cause a slight increase in the number of moles (12) and therefore possibly an increase in melanoma risk. But it is important to distinguish between an increase in incidence and in mortality. If the data show a slight increase in incidence with increased sun exposure, this may be balanced by the fact that mortality due to malignant melanoma is much lower with high levels of sun exposure than with low levels (13). Melanoma can arise in a number of ways, and has a multifactorial aetiology (14), but there is no linear relationship between sun exposure and malignant melanoma. This has already been discussed extensively in an article in the Journal of the Norwegian Medical Association (15), and the conclusion was that there is no evidence that changes in Norwegians’ sun exposure habits can explain the enormous increase in incidence and mortality of malignant melanoma. On the contrary, awareness of the potentially harmful effects of sunbathing and the use of sunscreen with ever higher sun protection factors (SPF) ought to have led to a reduction in the number of malignant melanomas. The weakness of the evidence base for concluding that UV radiation is a major cause of the increase in malignant melanoma is under-communicated, including in the Norwegian UV and Skin Cancer Strategy (16).
High sun protection factor?
The intervention that has attracted most media attention is the recommendation to use sunscreen with a high SPF. However, studies that are not randomised and double-blind have a risk of selection bias. There has been only one randomised clinical interventional trial on whether sunscreen can protect against skin cancer (the Nambour Skin Cancer Prevention Trial). This was an open study in which half the participants were given free SPF 16 sunscreen along with instructions to apply it to the head, neck, arms and hands every day, while the other half received no specific intervention and presumably continued as before. Half of the participants were also independently randomised to take beta-carotene or placebo. The study tested the effect on keratinocyte carcinomas only, and the results showed that neither sunscreen nor beta-carotene had any effect on these cancers (17). However, a follow-up study was subsequently conducted that also included malignant melanoma, and this study found an almost significant (p = 0.051) reduction of malignant melanoma in the sunscreen group (11 of 812 versus 22 of 809) (18). A new endpoint was thus added after the study had been completed, which is not good practice. No change in melanoma-related mortality was detected, but the follow-up time was too short to see any long-term effects.
Sunscreen may lead to more time in the sun
A Norwegian cohort study (19) of women over the age of 40 used Cox regression to investigate the association between use of sunscreen and risk of malignant melanoma. In a model that included hair colour, freckles, UV radiation in region of residence, and the results of follow-up questionnaires, there was no significant difference between those who used high SPF sunscreen and those who used no sunscreen at all. The authors’ explanation was that the latter group comprised participants who were less exposed to UV radiation.
We simply do not know whether sunscreen can increase or decrease the incidence and mortality of malignant melanoma
Some previous analyses have found a positive association between malignant melanoma and the use of sun-protection creams, i.e. that the use of sunscreen increases the risk of malignant melanoma, but recent meta-analyses find no such association (20, 21). We simply do not know whether sunscreen can increase or decrease the incidence and mortality of malignant melanoma. It is hard to imagine that sunscreen per se can cause malignant melanoma, but if people use sunscreen to enable them to stay in the sun longer rather than to reduce their UV exposure, that could explain the previous findings. In a French randomised double-blind placebo-controlled trial, one group of participants was given SPF 30 and another SPF 10. There proved to be no difference between the two groups in the number of cases of sunburn, but those who received SPF 30 sunbathed far longer than those who received SPF 10 (22).
Questions have been raised about whether sunscreen may be harmful. In the Norwegian Consumer Council’s sunscreen test in 2017, 37 of the 45 sunscreens tested were found to be either environmentally damaging, allergenic or to cause hormone imbalances (23).
Vitamin D and sun
The optimal level of 25-hydroxyvitamin D3 (calcidiol) in the blood is unknown. A recent Norwegian study showed that mortality due to lymphomas and cancers of the breast, colon and lungs was markedly lower in patients with high serum concentrations of vitamin D (24). It is well known that the sun’s rays are an important source of vitamin D, and sunscreen may possibly increase the risk of vitamin D deficiency. A meta-analysis showed that under experimental conditions, the use of sunscreen significantly reduces vitamin D levels, but in field studies no significant effect has been found (25–27). Field studies will be affected by compliance, and it is possible that people spend more time in the sun if they use sunscreen. The field studies in question were carried out using low SPF sunscreen; no such studies have been performed with the high SPF sunscreens now recommended by the authorities. A Swedish study found that all-cause mortality was twice as high in individuals who avoided sun exposure compared to those who sunbathed the most (28). This cohort study thus suggests that avoiding sunbathing may be about as dangerous as smoking tobacco. But we do not know whether avoiding sunbathing is equivalent to using high SPF sunscreen.
There may be reason to be a little less afraid of exposure to the sun
The scientific literature does not substantiate the claim that sunlight and sunbathing are chiefly responsible for the large increase in malignant melanoma, and it seems more accurate to say that the causes of this increase are unknown. The authorities’ warnings against sunbathing, and their promotion of the use of sunscreen, have a weak scientific basis. There may be reason to be a little less afraid of exposure to the sun. We should recapture the joy of becoming tanned in the summer, and of seeing happy, suntanned children.
What constitutes sensible advice?
The scientific literature provides evidence that severe sunburn can increase the risk of malignant melanoma, and we should avoid becoming severely sunburned. The duration of sunbathing should be limited during the first few days of a holiday; the dose can then gradually be increased as a tan develops. Those with the most photosensitive skin (skin types 1 and 2) should protect their skin from sunlight by wearing a hat and other protective clothing or by staying in the shade as much as possible if there is a risk of becoming severely sunburned, and should only expose their bodies to direct sunlight for short periods. Public and private outdoor areas (for example, gardens) should allow people the option of staying in the shade. If you are exposed to strong sun and it is not possible to protect yourself from sunlight in a natural way, you should use sunscreen. Even those whose skin tans after sunbathing can be exposed to too much sun over the course of an entire day spent on the beach, skiing in the mountains, on a boat or in an open safari vehicle. But these are the exceptions. It is not advisable to lie in the sun all day, even when using high SPF sunscreen. Sunscreen has an uncertain place among measures for preventing malignant melanoma.