Kikuchi’s disease is characterised by swollen lymph glands in the neck plus fever. Here we describe the first case to be reported in Norway.
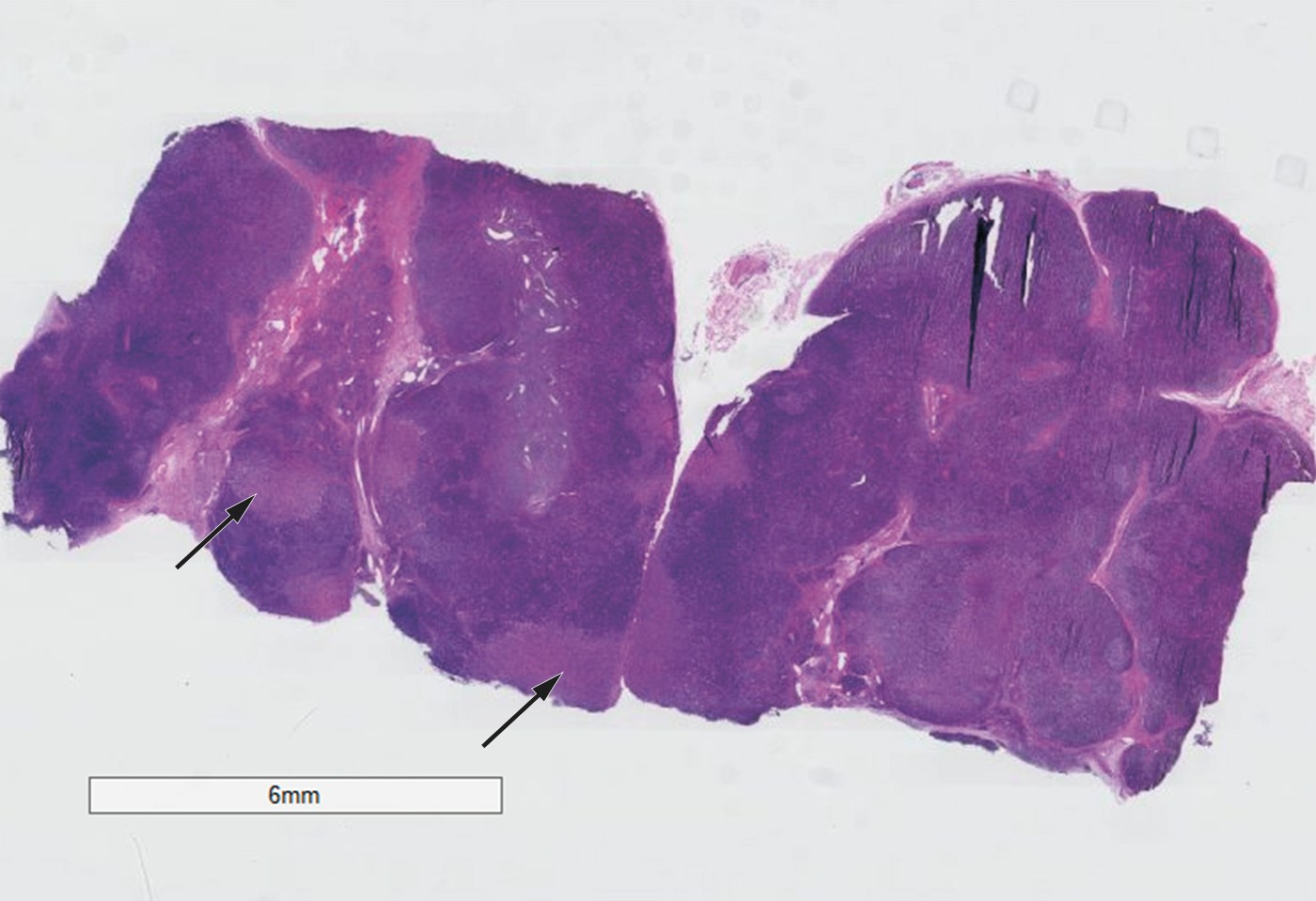
Figure 1 Haematoxylin and eosin-stained section. The arrows point to necrotic areas of the lymph node.
A 30-year-old patient had multiple swollen lymph glands on the left side of her neck. She also reported night sweats and a reduced general condition. The symptoms had persisted for a month on presentation. Clinical examination detected multiple hard, rounded and enlarged lymph nodes on the left side of her neck all the way from the skull base to the clavicle, but no other pathology. Extensive examination for infectious agents yielded negative findings. Fine needle biopsy showed lymphoid material and normal flow cytometry counts. MRI revealed the clinically detected lymph nodes and suspected lymphoma. We then performed an open biopsy of a nuchal lymph node, since the patient was still unwell. Pathology results showed necrotising lymphadenitis with an increased number of histiocytic cells, giving rise to suspicion of Kikuchi’s lymphadenopathy. We hereby present the first reported case of Kikuchi’s lymphadenopathy in Norway.
A woman in her thirties attended the Otolaryngology Department because of swollen lymph glands in her neck, reduced general condition and night sweats, all of which had begun a month previously. The patient had had a tonsillectomy as a child, but had otherwise been in good health. She had not been exposed to tuberculosis, had not been abroad recently and was in a stable relationship. She had only drunk water from the mains supply and had had no recent contact with animals.
Clinical examination revealed multiple pathologically enlarged lymph nodes on the left side of the neck, extending from the skull base to the clavicle. The lymph nodes were rounded, hard and enlarged to approximately 1.5 cm in diameter. The patient had otherwise normal otolaryngology status, and a full-body clinical examination revealed no other pathology. Fine needle aspiration of a pathological lymph node was performed to obtain material for cytological and flow cytometric analysis.
Blood samples were taken to check for malignancy and for autoimmune conditions such as sarcoidosis and rheumatic disorders, for infection with HIV, hepatitis B and C, cytomegalovirus, herpes simplex virus, borreliosis, tuberculosis (QuantiFERON) and Epstein-Barr virus, and to check general organ status.
The results of cytological and flow cytometric analysis showed lymphoid tissue without abnormal cells and with a normal immune profile. CT from the skull base to the abdomen and cervical MRI both showed generally enlarged lymph nodes in the neck, and the findings were considered consistent with lymphoma.
As the patient still had symptoms when the results of the cytological analysis became available, it was decided to perform an open biopsy. Following uncomplicated removal of a nuchal lymph node, the tissue was sent for routine bacterial culture, plus testing for tularaemia, Bartonella bacteria, and tuberculous and non-tuberculous mycobacteria. Parts of the node were placed in saline and formalin for pathological assessment.
All bacteriological and virological tests were negative for current infection. Serum ferritin was 269 µg/l (reference range 18–240 µg/l), CRP 7 mg/l (<5 mg/l), AST 40 U/l (15–35 U/l), fibrinogen 4.1 g/l (2–4 g/l) and D-dimer 0.61 mg/l FEU (<0.5 mg/l FEU). Other blood tests were normal.
The pathologist described necrotising lymphadenitis in the biopsy. The lymph node was enlarged with necrosis in the cortical zone. An increase in blast cells was seen in the intrafollicular zone, with the following immune profile as revealed by staining: CD30-positive, CC15-negative and CD3-dominant positive. Some of the blast cells were also positive for CR20/PAX5. Flow cytometry and PCR both revealed a normal polyclonal phenotype for B cells. Staining for the immunomarker CD68 revealed a markedly increased number of macrophages, i.e., histiocytic cells. The pathologist therefore suspected Kikuchi’s disease, also known as histiocytic necrotising lymphadenitis.
Discussion
Kikuchi’s disease is a benign condition with unknown cause characterised by swollen lymph glands in the neck and fever. The most frequent symptoms are lymphadenopathy (100 %), fever (35 %), rash (10 %), arthritis (7 %), fatigue (7 %) and hepatosplenomegaly (3 %) (1). The disease mimics a number of serious conditions and is diagnosed on the basis of a characteristic histopathological profile in lymph node biopsy and by excluding other causes of lymphadenopathy, in particular lymphoma and systemic lupus erythematosus (2). Upon re-examining lymph node biopsies, one study found that 30 % of cases of Kikuchi’s disease had been misdiagnosed as lymphoma (3). Disease histology is dominated by abundant CD68-positive lymphocytes that typically express myeloperoxidase (4). Most patients recover from Kikuchi’s disease within six months without treatment. Individual cases with severe and persistent or recurrent symptoms have shown rapid remission following treatment with glucocorticoids (5).

Figure 2 CD68 immunostaining, showing a clear increase in the number of histiocytic cells.
Kikuchi’s disease is seen in patients of all ages, but most are under 40. The disease has been reported worldwide, with the highest prevalence in Asia. In a Korean study with 147 patients, Kikuchi’s disease was the most frequent cause of lymphadenitis (34.7 %) (6). However, a study in Saudi Arabia that examined 920 lymph node biopsies performed on the basis of enlarged lymph nodes reported a prevalence of only 0.5 % (7). The disease is associated with the development of systemic lupus erythematosus, and patients with Kikuchi’s disease should therefore be followed up for several years. A Korean study from 2001–2006 found that of 102 patients with Kikuchi’s disease, three developed systemic lupus erythematosus (8). This is notably higher than the incidence of systemic lupus erythematosus in the general population (1–25 cases per 100 000) (9). A study from 2016 found three patterns among patients with both Kikuchi’s disease and systemic lupus erythematosus: 30 % of patients had had Kikuchi’s disease before they developed systemic lupus erythematosus, 47 % had simultaneous onset and diagnosis of both conditions, and 23 % had systemic lupus erythematosus and subsequently developed Kikuchi’s disease (10).
We have found no other published cases of Kikuchi’s disease in Norway. Pathologists and clinicians should be aware of the condition to prevent misdiagnosis and to enable them to provide appropriate follow-up with respect to the risk of systemic lupus erythematosus. We encourage clinicians to perform a biopsy in all cases of lymphadenopathy of uncertain aetiology to help ensure correct diagnosis and treatment.
