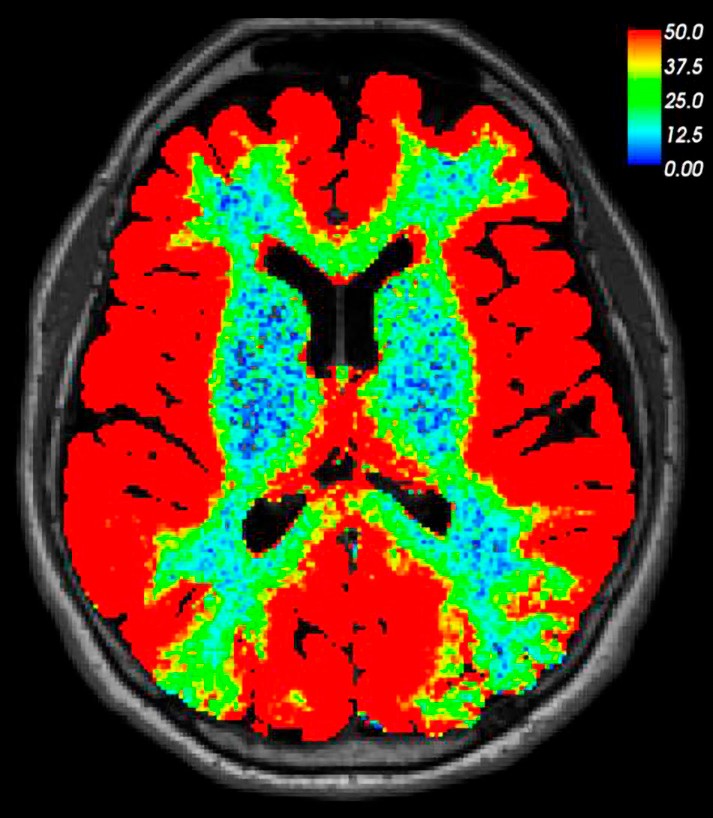
This brain MRI was taken 24 hours after lumbar puncture and intrathecal injection of an MRI contrast agent (0.5 ml gadobutrol). The patient was undergoing tests in the neurosurgical department owing to a suspected cranial cerebrospinal fluid leak. However, no leak could be detected in either the image taken after 24 hours or those that had been taken previously. In this image, which is based on T1-weighted MRI, we have used a colour scale to visualise the percentage increase in signal intensity in brain tissue as a result of contrast enhancement. The image shows that a small and water-soluble molecule like gadobutrol can produce contrast enhancement throughout the entire brain when administered via the cerebrospinal fluid. It had previously been unclear to what extent intrathecally injected drugs could enhance human brain tissue. Given that the contrast agent cannot leak into the bloodstream through an intact blood-brain barrier, we can state with certainty that the enhancement of brain tissue takes place entirely outside the blood vessels.
Since most drugs administered orally or intravenously are unable to pass through the walls of cerebral blood vessels, characterising the route into the brain from the spinal fluid could open up new possibilities for the diagnosis and treatment of brain disorders. It could also shed light on how meningeal lymphatic vessels can influence the brain via the cerebrospinal fluid (1).
Much evidence suggests that the MRI contrast agent enhances brain tissue via the so-called glial lymphatic or ‘glymphatic’ system, which was first described in 2012 (2). Cerebrospinal fluid acts as a transport medium for excretion of waste products such as amyloid-β and tau protein from the brain via the perivascular spaces (a form of ‘brainwashing’). There is reason to believe that gadobutrol is washed out of the brain along the same route as these waste products. Glymphatic MRI has shown this excretion to be reduced in patients with a particular form of dementia (normal pressure hydrocephalus) (3).