A young man was hospitalised with sudden onset paresis of the lower extremities, and spinal cord ischaemia was detected. Fibrocartilaginous embolism is most likely an underdiagnosed cause of spinal cord infarction: could this be the aetiology in our patient?
A foreign man in his twenties, who was visiting friends in Norway, woke up one night with intense pain between the shoulder blades. At the same time he noticed pins and needles in his upper and lower extremities. The pain eased off, and he went back to sleep. When he woke up some hours later, his arms and legs were weak and he was unable to stand. His friends drove him to hospital and carried him into the Emergency Department.
The man was previously healthy and used no regular medications. There were no hereditary diseases in his family. His medical history revealed no trauma prior to his hospitalisation. His respiratory rate was 16 per minute, blood pressure 120/76 mm Hg, pulse regular at 85 beats per minute and he did not have a fever. Routine admission blood tests were normal. Neurological examination revealed asymmetric weakening, paresis, in all four extremities. His left lower extremity was paralysed, i.e. loss of voluntary movement. There was some movement of the right hip, but not against resistance, graded as 3/5. The grade further distally was 4/5 in the knee and ankle joints. In the upper extremities, the paresis was more pronounced further distally. Strength in the wrists was graded 3/5 for flexion and 4/5 for extension bilaterally. The patient could hold his arms out in front of him for three seconds, but the left arm drifted more than the right. From level Th3 there was also reduced sensibility to pin-prick. His sense of position, or proprioceptive sense, was preserved. His reflexes were brisk in the upper extremities and absent in the lower extremities. Plantar responses were indifferent. The patient felt no urge to urinate, but catheterisation nevertheless revealed 750 ml urine. Sphincter tone was diminished. The symptoms gave rise to suspicion of pathology in the anterior cervical medulla. MRI of the spinal cord was therefore performed five hours after onset.
The MRI revealed increased DWI signal and reduced ADC values in the ventral part of the spinal cord from level C5 through Th1, extending almost 7 cm (Fig. 1). The spinal cord was not swollen, and no contrast enhancement was detected. An axial image (Fig. 2) at the same levels showed increased T2 signal in the anterior horn bilaterally, so-called snake-eye appearance, consistent with one of the known patterns of ischaemia in the area supplied by the anterior spinal artery. Findings of restricted diffusion with “vascular distribution” aroused suspicion of cytotoxic oedema due to acute ischemia. At this point there was no evidence of infection, as the patient was afebrile and had normal blood test results. Inflammation was still a possible differential diagnosis. There were no signal alterations and no evidence of infarction or other pathology in the cervical vertebral bodies, but somewhat dehydrated discs. Later the same day a CT angiogram of the aorta was performed, which did not reveal dissection, aneurisms or any other source of embolism.
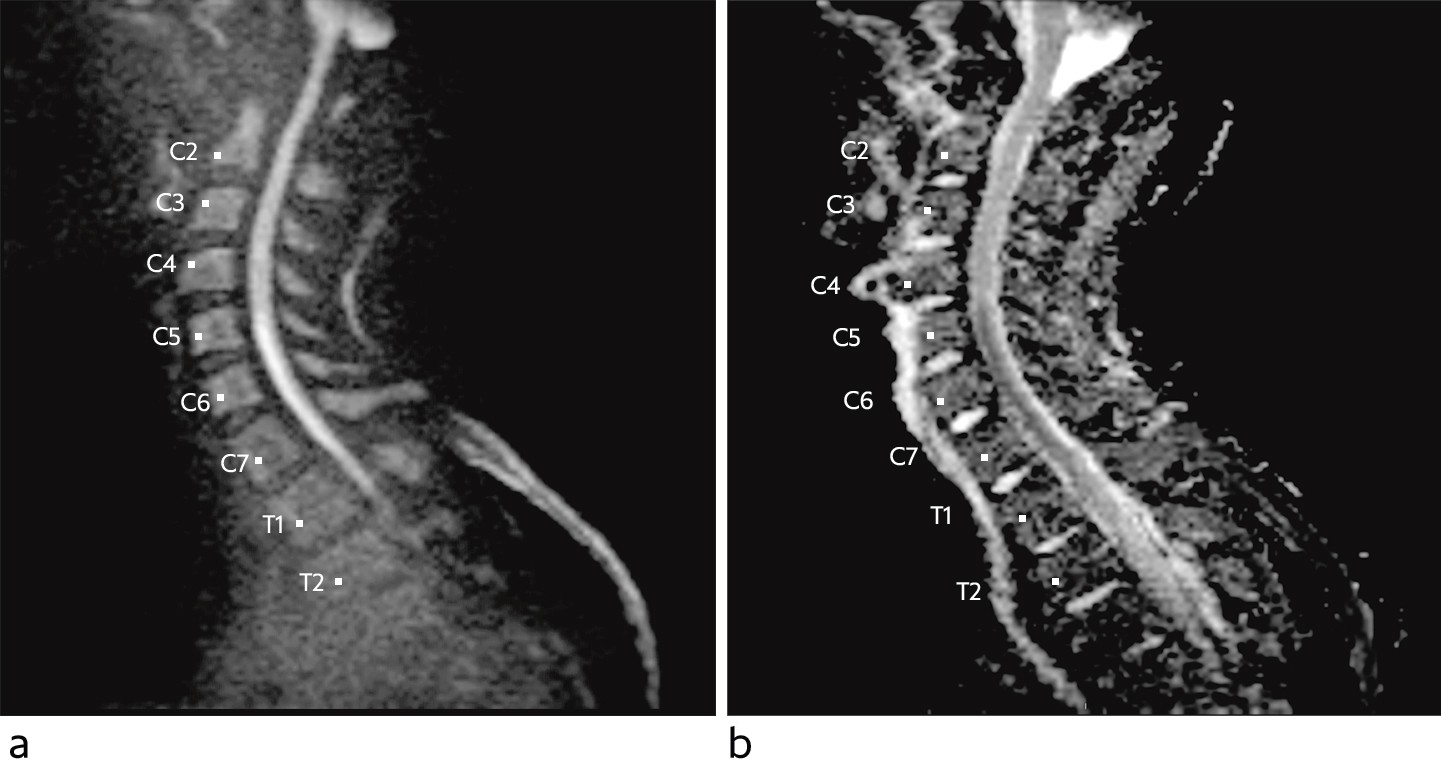
Figure 1 Sagittal diffusion-weighted MRI sequence with b-1 000 image (a) and apparent diffusion coefficient (ADC) map (b) shows diffusion restrictions in the ventral part of the spinal cord from the level of C5 to Th1, consistent with cytotoxic oedema.
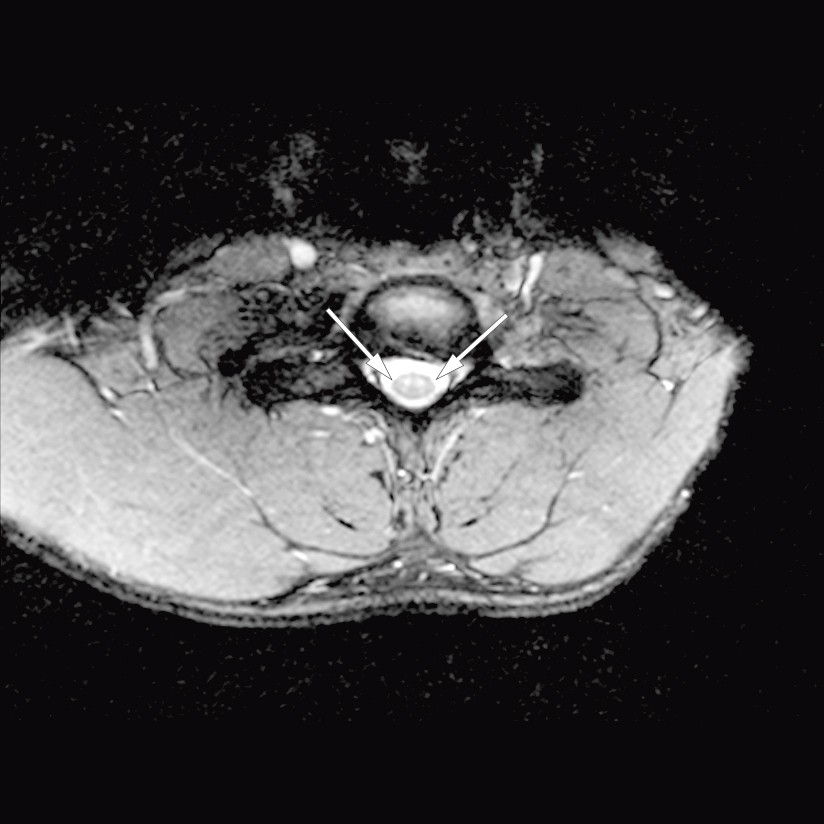
Figure 2 Axial T2 image at level C6. Increased signal corresponding to the anterior horn bilaterally, but normal signal in surrounding medulla. The pattern is termed ‘snake eyes’, and is consistent with the area supplied by the anterior spinal artery.
The patient had a lumbar puncture performed the same day, which was normal. Analysis of isoelectric focusing was completed a week later and revealed no non-serum-like bands, such as seen in demyelinating diseases, for example. He was transferred to the Intensive Care Unit (ICU) for respiratory monitoring and to maintain an adequate mean arterial pressure (MAP) in the acute phase of the infarction. By keeping his mean arterial pressure above 90 mm Hg, we aimed to prevent an increase in the size of the infarction by ensuring perfusion in a possible watershed area of the spinal cord. A vasopressor was administered to maintain the mean arterial pressure. This was discontinued after three days, when the oedema in the infarction area was thought to be established and had passed its peak. The patient was not at any time in need of respiratory support. He had significantly reduced cough strength initially, with a peak expiratory flow (PEF) of 170 l/min., and there was risk of bronchial infection.
In the ICU the patient’s cardiac rhythm was monitored for three days without atrial fibrillation or other heart rhythm disorders being detected. Transthoracic and transoesophageal echocardiography did not reveal any potential sources of embolism in the heart or aorta. Additional blood tests with the aim of detecting hypercoagulopathies revealed no pathology. 300 mg of acetylsalicylic acid and 300 mg of clopidogrel were administered orally the first day, and thereafter the dosage was 75 mg daily of both. There was progression of pareses during the first 48 hours, before a slow improvement was seen. The patient remained in the ICU for a total of nine days, and his PEF reached 250 l/min.
The patient was well under way with mobilisation when he was moved to the neurological ward. Dual antiplatelet therapy with acetylsalicylic acid and clopidogrel was discontinued after four weeks, and he was prescribed single life-long antiplatelet therapy in the form of clopidogrel. After two weeks of hospitalisation in Norway, the patient returned to his home country and underwent further rehabilitation there. Five months after the onset of symptoms, the patient still has considerable paresis in all four extremities and is in need of a walking aid. His strength is reduced, particularly in the left leg, the wrists and the fingers. The patient claims to be in good spirits despite spasticity, leg pain and urinary retention.
Discussion
Spinal cord infarction is rare and accounts for 0.3–1 % of all infarctions of the central nervous system (1). Studies with long term follow up of patients with spinal cord infarction reveal that the patient group has a better chance of returning to work and to be in a better emotional and mental state than patients with cerebral infarction (1). This is probably because patients with spinal cord infarctions do not have cognitive sequelae.
The cause of our patient’s spinal cord infarction was not uncovered. MRI images revealed Schmorl´s nodes and some degenerative changes in thoracic vertebral bodies. The most common cause of spinal cord infarction is aortic pathology, or iatrogenic origin following aortic surgery, but fibrocartilaginous embolism is described in the literature as being a likely underdiagnosed cause of spinal cord infarction (2, 3). Theories suggest that fibrocartilaginous material from the nucleus pulposus in degenerated discs can undergo retrograde migration by way of adjacent vascular structures to the arterial blood supply (2, 4). The most common is an embolism to the spinal cord, but fibrocartilaginous embolisms of the lungs, brain, vertebral bodies and ribs have also been described (2). Fibrocartilaginous embolism is well known in veterinary medicine, particularly in dogs (5). In humans, it is probably often misdiagnosed as transverse myelitis. The diagnosis is difficult to make, and can only be confirmed by autopsy with histopathology. This diagnosis should be suspected when typical clinical findings such as back and neck pain are followed by acute onset and progressive paresis, possibly preceded by a minor trauma, the absence of vascular risk factors, MRI findings consistent with ischaemia and normal findings in cerebrospinal fluid, coupled with the exclusion of other possible causes. The preceding trauma may be something as minor as lifting shopping bags or straining when on the toilet (6). In contrast to inflammatory conditions, there is rapid progression of symptoms in spinal cord infarctions, typically over the course of a few hours. With infarctions in the territory of the anterior spinal artery, proprioception and pallesthesia (vibratory sensation), are not affected, as in the case of our patient.
