A woman with acute abdominal pain was admitted to hospital with suspected cholecystitis. In addition to abdominal pain, she had vomiting, loss of appetite, diarrhoea and symptoms of pyrexia. She had no symptoms from the respiratory tract, but was later found to have COVID-19. A number of patients have presented with similar symptoms at our hospital. This has led to temporary changes in our procedures for handling and investigating patients with acute abdominal pain.
In the early stages of the corona epidemic a woman in her late forties was referred to the acute admission unit at a regional hospital due to acute abdominal pain and suspected cholecystitis. The woman had pre-existing hypertension for which she was taking medication. She was obese with a body mass index (BMI) of 34 kg/m2. Many years earlier, she had been treated for miliary tuberculosis involving the lungs and peritoneum. A previous CT scan had shown gallstones, but she had never experienced any gallbladder attack.
The woman reported that she had had constant abdominal pain for eight days prior to admission. Earlier in the week, she had been in contact with her GP, who had prescribed esomeprazole (Nexium) 40 mg daily for suspected dyspepsia. She located the pain to the epigastrium and upper right quadrant, with pain exacerbation after eating. The patient also reported a feeling of fluctuating temperature. In addition, she had also experienced loss of appetite, nausea, several episodes of vomiting and one episode of diarrhoea.
On clinical examination, the patient was lethargic and there was a decline in her general condition.
Her body temperature was 37.1 °C after taking paracetamol. The patient had an increased respiratory rate of 28 breaths per minute, and her oxygen saturation measured by pulse oximetry was 95 % on room air. She was tachycardic, with a pulse of 100 beats per minute. On auscultation of the lungs, there were normal findings. On abdominal examination, she had tenderness on palpation under the right costal margin and in the epigastrium. She also had pain during inspiration and palpation under the right costal margin (positive Murphy’s sign).
Blood tests showed elevated CRP 107 mg/l (0–4) but a normal leukocyte count. Her liver function tests were normal, but she had elevated lactate dehydrogenase 375 U/L (115–255). The receiving doctor considered cholecystitis to be the most likely cause of the symptoms. The patient met one of the three criteria in the qSOFA scoring system (increased respiratory rate) and her SIRS criteria score was two out of four (increased respiratory rate and tachycardia). The doctor suspected an ongoing infection and initiated intravenous antibiotic therapy in the form of piperacillin/tazobactam 4 g three times daily.
An ultrasound examination of the liver and biliary tract was requested. However, as the patient was overweight, and several radiologists were in quarantine due to the ongoing corona epidemic, it was decided to do a CT scan with intravenous contrast instead. The CT images of the abdomen showed no relevant findings in the abdomen, except gallstones that were previously known. There were no radiological signs of cholecystitis. However, cross-sectional images of the lower thorax showed peripherally diffuse opacities in both lungs as well as some areas with a more consolidated appearance. There were no signs of pleural effusion. The radiologist suspected viral or atypical pneumonia (Figure 1).
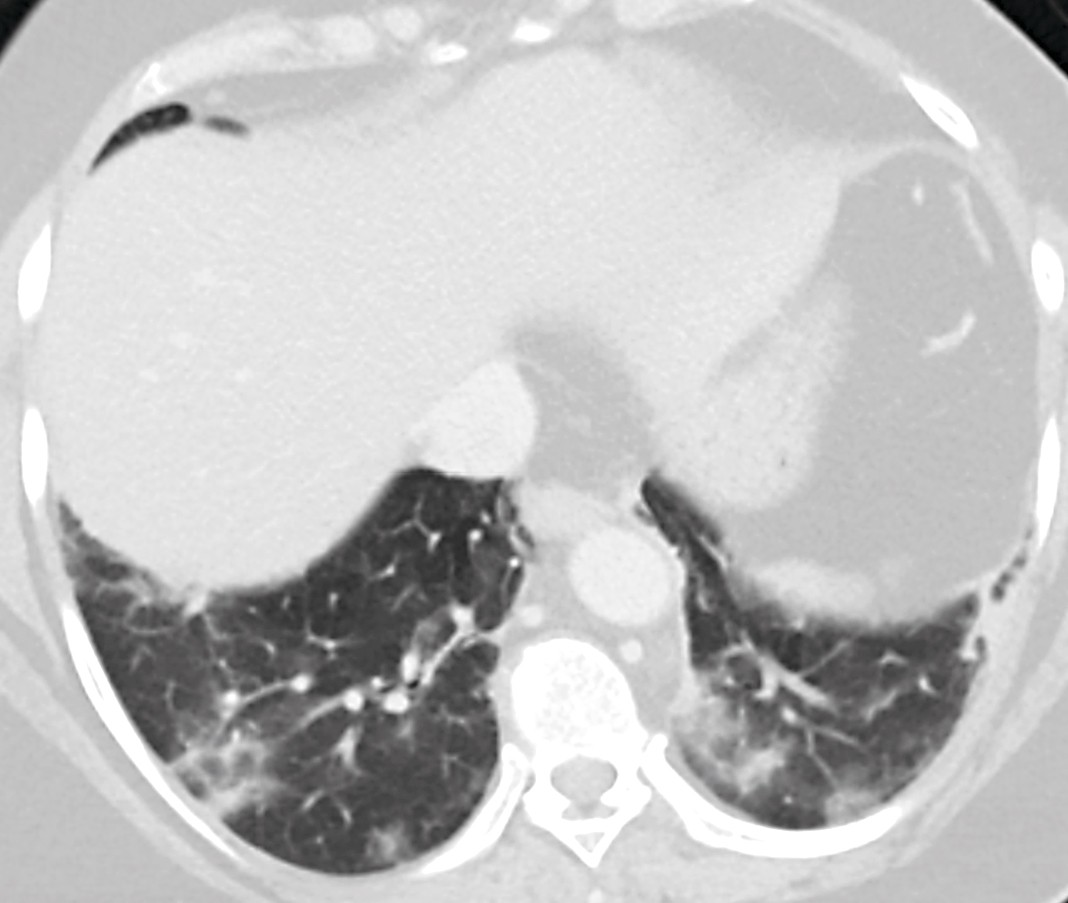
Figure 1 Cross-sectional image of the bases of the lungs as part of the CT examination of the abdomen. The image shows peripheral, patchy bilateral ground glass opacity with elements of consolidation.
Due to the ongoing corona epidemic, enhanced droplet precautions were immediately established. The woman was subsequently measured with a temperature of 38.0 °C and a respiratory rate of 20 breaths per minute. Oxygen saturation was 94 % on room air. Upon re-questioning, the patient reported that she did not have a cough, shortness of breath, sore throat or muscle pain. She said she had not travelled abroad during the past two weeks or been in close contact with anyone with COVID-19. Nevertheless, it was decided to take a swab from the nasopharynx and the throat for qualitative detection of SARS-CoV-2 RNA with real-time polymerase chain reaction (PCR).
A virologic test confirmed that the patient was positive for SARS-CoV-2. Hospital staff who had been in close contact with the patient before droplet precautions were established, were immediately notified of the need for a 14-day quarantine in line with the Norwegian Institute of Public Health’s guidelines (1). The patient was transferred to the infectious diseases department at her local hospital. She did not develop respiratory tract symptoms over the next two days, and as she was feeling better, she was discharged with a plan for home isolation.
Discussion
On 11 March 2020, the World Health Organization declared the spread of the novel coronavirus SARS-CoV-2, causing COVID-19, a global pandemic (2–4). Common symptoms of COVID-19 are a cough, fever, muscle pain and fatigue, with later onset of shortness of breath and eventual acute respiratory distress syndrome (ARDS) in some (5–7). The typical symptoms and radiological findings of ground glass opacity and reticular changes (crazy paving) have recently been described in a case study published in the Journal of the Norwegian Medical Association (8).
However, some patients with COVID-19 present with other symptoms. Over the past two weeks, our acute admissions unit has seen an additional five patients with similar symptoms, where COVID-19 has been confirmed by real-time PCR. The main complaint of all of these patients was abdominal pain, with some also having lower abdominal pain. In addition, they reported loss of appetite, nausea and vomiting. Some also had diarrhoea, but none had new symptoms from the respiratory tract. All underwent a CT examination of their abdomen, as part of the assessment of their abdominal pain, where the images showed typical findings for COVID-19 in the lungs (Figure 2).
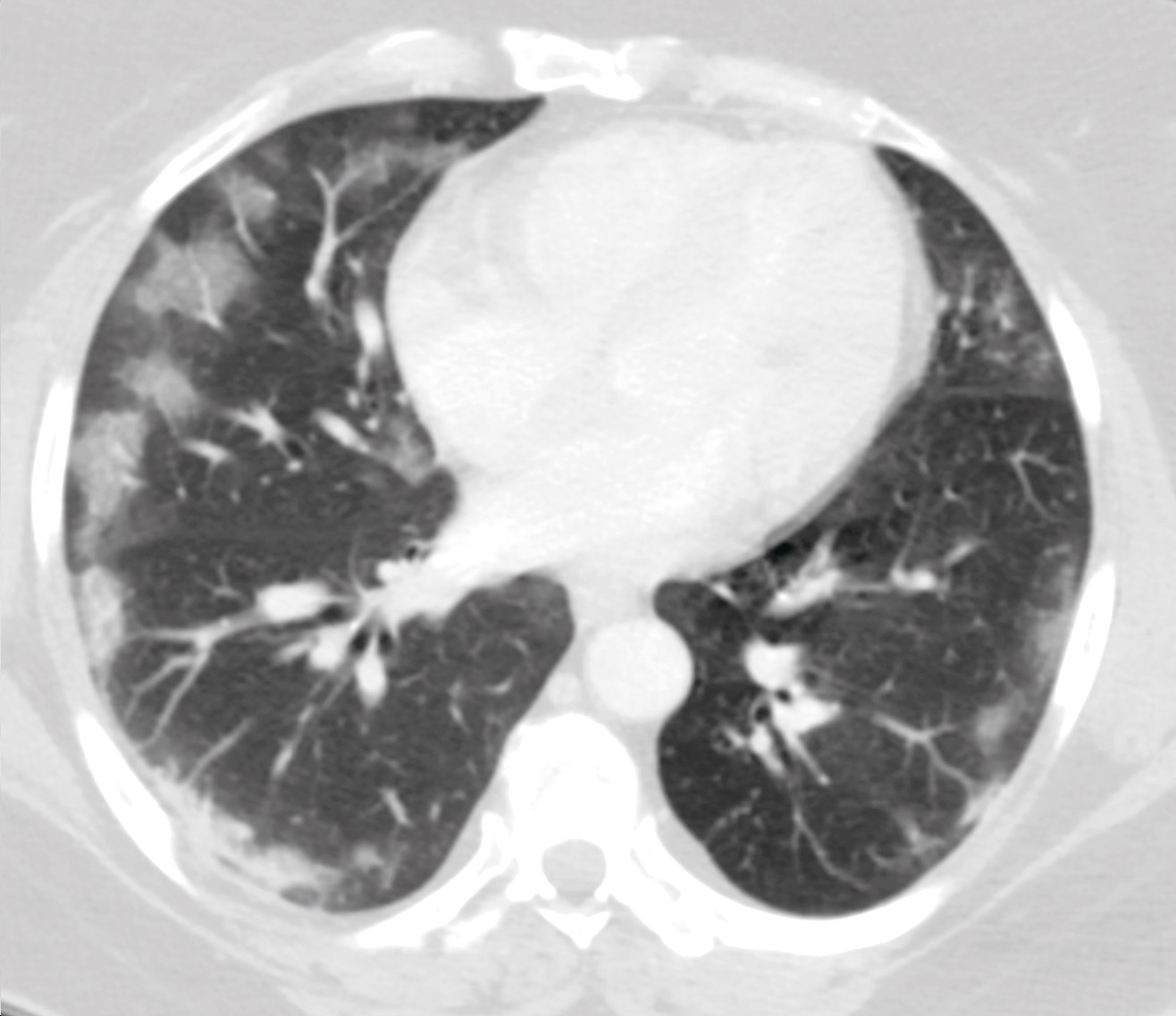
Figure 2 CT image of patient (not actual case study) with acute abdomen as an early symptom. The image shows the lower part of the thorax and shows patchy, bilateral characteristic ground glass opacity with peripheral distribution. The patient gave consent for the image to be published.
Studies have increasingly reported symptoms from the gastrointestinal tract in COVID-19 patients (6, 7, 9). In a large study of 1099 patients with COVID-19, 5 % had nausea and 3.8 % vomiting. The study also found that 8.9 % never developed viral pneumonia (7). In a recently published study of 204 patients with confirmed COVID-19, it was reported that about half of the patients had symptoms of loss of appetite, diarrhoea, vomiting and abdominal pain. It was found that the period of time from onset of symptoms to hospitalisation was longer for patients with gastrointestinal symptoms than for patients with respiratory tract symptoms, and that those with gastrointestinal symptoms had a poorer prognosis (10).
In other infections caused by phylogenetically similar coronaviruses, such as Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS), it has been reported that 20–25 % of patients initially experienced symptoms from the gastrointestinal tract (11-13).
Basal pneumonia with pleural effusion may explain pain and discomfort in the upper abdomen. However, it is less likely that basal pneumonia will cause lower abdominal pain and symptoms such as nausea, vomiting and diarrhoea. Other mechanisms must therefore be suspected. Similar to SARS-CoV, SARS-CoV-2 has been shown to have proteins that readily bind to the cell receptor angiotensin-converting enzyme 2 (ACE2) (3). There are many ACE2 receptors on type 2 alveolar cells in the lungs, and the lungs are therefore particularly at risk. Cells in other organs have also been shown to have ACE2 receptors. The virus can therefore invade, multiply and cause infection in several organ systems. A high proportion of ACE2 receptors has been seen in the heart, ileum, oesophagus, kidneys and bladder. In one study, epithelial cells in the ileum were reported to have a very high proportion of ACE2 receptors (30 %, versus 1 % in the lungs) (14).
Our experiences with the COVID-19 pandemic to date have led us to change the procedures in the radiology and surgery departments. Droplet precautions are used for all patients with unexplained upper abdominal pain, as well as all patients with abdominal pain (irrespective of location) and concomitant fever, until test results of COVID-19 are available. Since the typical COVID-19 findings are not necessarily located on the bases of the lungs, a CT thorax is also performed at the same time as the abdominal CT. This does not entail extra time in the CT machine. We also believe that since many patients with acute abdomen often end up getting a CT scan as part of their investigative procedures, consideration should be given to primarily doing a CT scan of the thorax, abdomen and pelvis, instead of an ultrasound examination of the abdomen and a conventional thoracic x-ray, during the current epidemic.
Early suspicion of COVID-19 is crucial for early diagnosis and reducing the risk transmission. At the time our patient was admitted, procedures had already been established for early assessment of the risk of infection in all patients arriving at our acute admission unit (pre-triage). This assessment includes questions on travel history and close contact with people with confirmed COVID-19. Enhanced droplet and contact precautions are used for a large proportion of patients. Our patient was pre-triaged in accordance with the procedures at the time, but enhanced droplet precautions were not established.
Our experience indicates that unexplained abdominal pain should be considered as a criterion in the pre-triage procedure. This will potentially reduce the risk of transmission to other patients and hospital staff. However, the experiences with COVID-19 are at an early stage, and ongoing assessments must be made of the most appropriate patient management procedures.
