In most cases, cataract surgery provides a permanent, good visual outcome. However, the artificial intraocular lens may become dislocated after some years. In the following case report, this complication led to sub-acute loss of vision several years after cataract surgery.
A man in his late seventies noticed one day that the vision in his left eye had suddenly become greyish and unclear. He had undergone a cataract operation on this eye seven years earlier, with standard implantation of an artificial intraocular lens in the existing lens capsule. The man had no other physical symptoms and was referred to an ophthalmologist.
The examination showed corrected Snellen visual acuity of 1.0 (right) and 0.2 (left). The left eye had an elevated intraocular pressure of 33 mg Hg. Red reflex was reduced and uneven, and a white opacity was observed in the pupil opening. Pupil dilation showed that the intraocular lens with surrounding capsule had dislocated downwards so that the upper lens haptic and an opaque portion of the capsule obstructed the visual axis. A number of zonular fibres that had ruptured from the suspensory ligament to the ciliary body could be observed in the upper part of the complex (Fig. 1). The diagnosis of late in-the-bag intraocular lens dislocation was made.

Figure 1 The intraocular lens with surrounding capsule dislocated downwards.
The patient was given pressure-lowering eye drops and indication for surgery was found. He was included in a research trial and randomised to having the intraocular lens with the surrounding capsule sutured to the sclera. The operation proceeded without complications (Fig. 2). His vision improved gradually to 1.25 after six weeks, and the intraocular pressure normalised so that the dosage of pressure-reducing medications could be reduced. Examination of the optic nerve revealed no definite glaucoma damage. The patient was followed up, and no complications occurred.
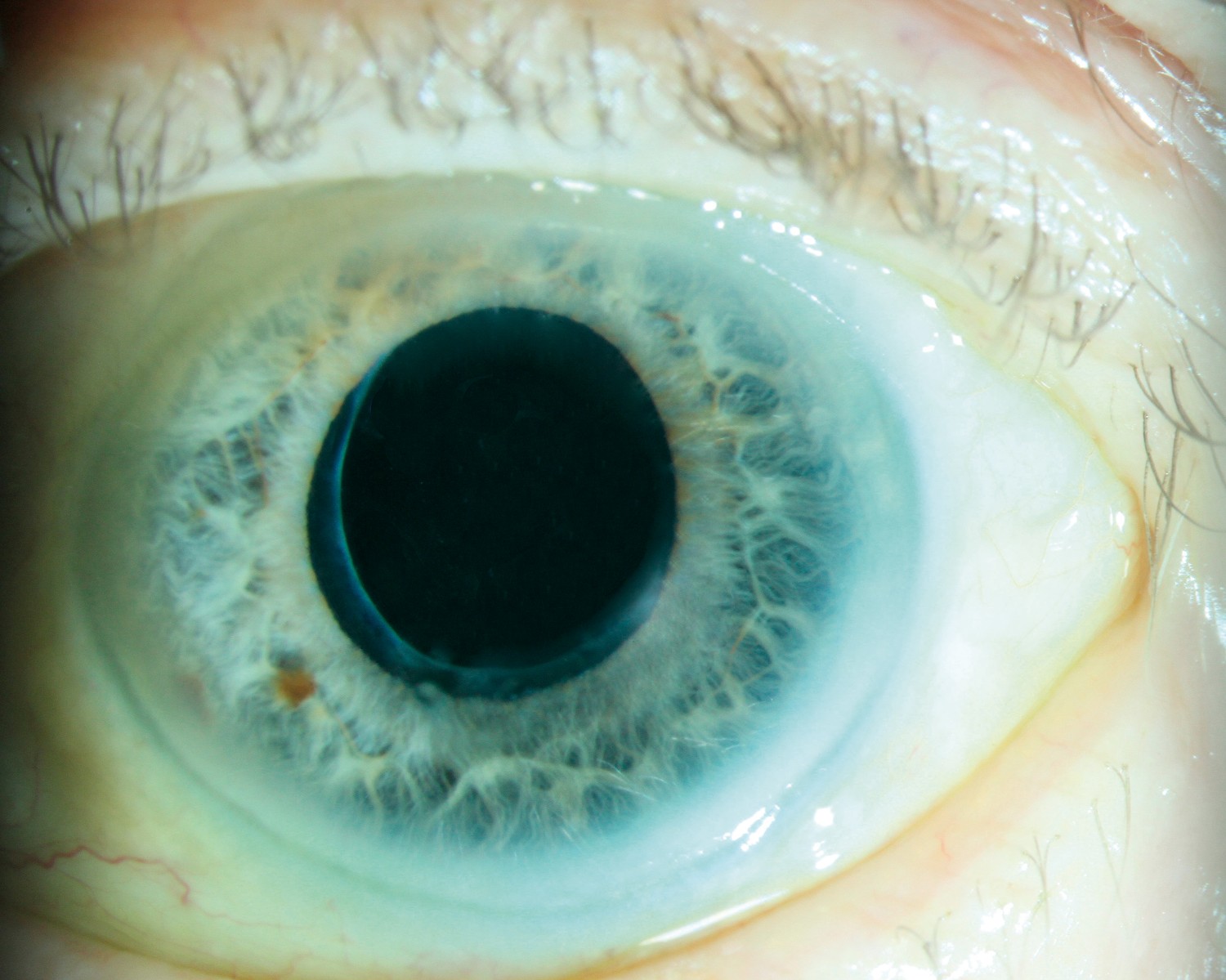
Figure 2 The eye with centred lens complex six weeks after the operation.
Discussion
This patient suffered dislocation of the intraocular lens seven years after cataract surgery. This type of dislocation, called late in-the-bag intraocular lens dislocation, was first described in 1993, and has been considered a rare complication (1). However, an increased frequency, with incidence of up to 0.5–1.0 % of all cataract patients, has been reported over the last few decades, and the dislocation occurs on average seven to ten years after the surgery (2, 3). Although this percentage is small, it represents a substantial number of patients. Over half the population is affected by cataract before the age of 75, and around 41 000 cataract operations are performed annually in Norway (4).
Lens dislocation is therefore a problem that general practitioners and A&E doctors may also encounter. The condition often arises spontaneously, but may be preceded by head trauma. There are several predisposing factors, and one of the most common is pseudoexfoliation syndrome, as in the case of our patient (3). This syndrome is seen mainly in elderly people and is particularly common in Scandinavia, with a reported prevalence of up to 20 % in the 60+ age group (5). The syndrome is characterised by fibrillary deposits in the anterior part of the eye, which may both weaken the zonular fibres’ attachment of the lens capsule and increase the risk of glaucoma (capsular glaucoma). Several studies have found a clear association between late intraocular lens dislocation and increased intraocular pressure, as with our patient. One hypothesis is that the dislocation itself affects the pressure (6), while another is that glaucoma arises concurrently, with pseudoexfoliation syndrome as a joint risk factor (7, 8). Experiences reported in the literature indicate that increased intraocular pressure in patients with dislocated intraocular lenses usually requires pressure-lowering treatment (7, 8).
The patient in this case report had very good vision after the operation. The visual prognosis in cases of surgery for late in-the-bag intraocular lens dislocation has been uncertain in the past, and some have regarded these procedures as risky. Furthermore, there has not been a clear consensus on the choice of operation method. Previous publications have indicated that the most widely used methods yield similar results, but these studies have been small and mainly retrospective. In a recently published randomised clinical trial, suturing of the dislocated complex was compared with exchanging it in favour of a new intraocular lens clipped to the iris. These methods yielded equally good visual results, and both were evaluated as safe (3, 9).
In cases of monocular, painless loss of vision in a previously cataract-operated eye, dislocation of an intraocular lens is an important condition to be aware of as a differential diagnosis for retinal detachment, vascular occlusion or vitreous haemorrhage. There are few contraindications to surgery, and research shows a good prognosis for postoperative vision. Acute surgery is not required, but it is an advantage to operate before the lens dislocates completely into the vitreous body. In our experience, patients should undergo surgery within a few weeks, depending on symptoms and findings. A substantial proportion have elevated intraocular pressure that must also be treated and monitored.