The current pandemic caused by the SARS-CoV-2 virus was predicted to reach Norway shortly after the outbreak in China (1). Following the government decision to virtually shut Norway down on 12 March (week 11), acute admissions departments have prepared for a large influx of infected patients. The Emergency Department at St Olav’s Hospital, Trondheim University Hospital is preparing for worst-case scenarios, but is now experiencing the calm before the storm. No Emergency Department health personnel are in quarantine, but as of 14 April 2020 a total of 15 members of the staff of St Olav’s Hospital have COVID-19 disease and 83 are in quarantine or at home with respiratory tract symptoms (2)
In recent years, the Emergency Department at St Olav’s Hospital has seen a gradual increase in patient visits (3). The patient population consists primarily of patients aged over 15 years. Acuity level is in all cases determined using the Rapid Emergency Triage and Treatment System (RETTS) (4) according to which patients are categorised as red, orange, yellow or green depending on assumed severity. Red patients must be seen immediately by a doctor, while green patients can wait if more urgent cases come at the same time. Children and adults presenting with problems in the fields of obstetrics and gynaecology, ophthalmology and ear, nose and throat are as a general rule received at separate receptions or clinics (3).
In this study we wanted to compare the inflow of patients in weeks 11 and 12, when St Olav’s Hospital stepped up its preparations for the pandemic, with the average for the previous weeks (weeks 2–10).
Material and method
Data from all patients who attended the Emergency Department at St Olav’s Hospital in the period 6 January 2020 to 22 March 2020 (weeks 2–10) were retrieved from the Emergency Department’s database (Akuttdatabasen, Helse-Vest ICT, version 1.5.5., Stavanger). We chose this period because we assume that it is representative of a stable flow of patients unaffected by public holidays. Logistical data such as patient numbers, medical issue, time spent in the Emergency Department, urgency, infection status and treatment level, were imported and processed using the Statistical Package for the Social Sciences (SPSS) version 25. Relevant data were then transferred to Microsoft Excel 2016 for graphical presentations. The study was approved by the data protection official (ESA no. 16/9114) and submitted to the Regional Committee for Medical and Health Research Ethics (REK 2016/1813).
Results
In Weeks 11 and 12, 426 and 331 patients, respectively, were referred to the Emergency Department, compared with the average of 541 patients in weeks 2–10. This is equivalent to a reduction of 115 patients (21 %) in week 11 and 210 patients (39 %) in week 12 (Fig. 1). The reduction was clear already in the middle of week 11 (Figure 2).
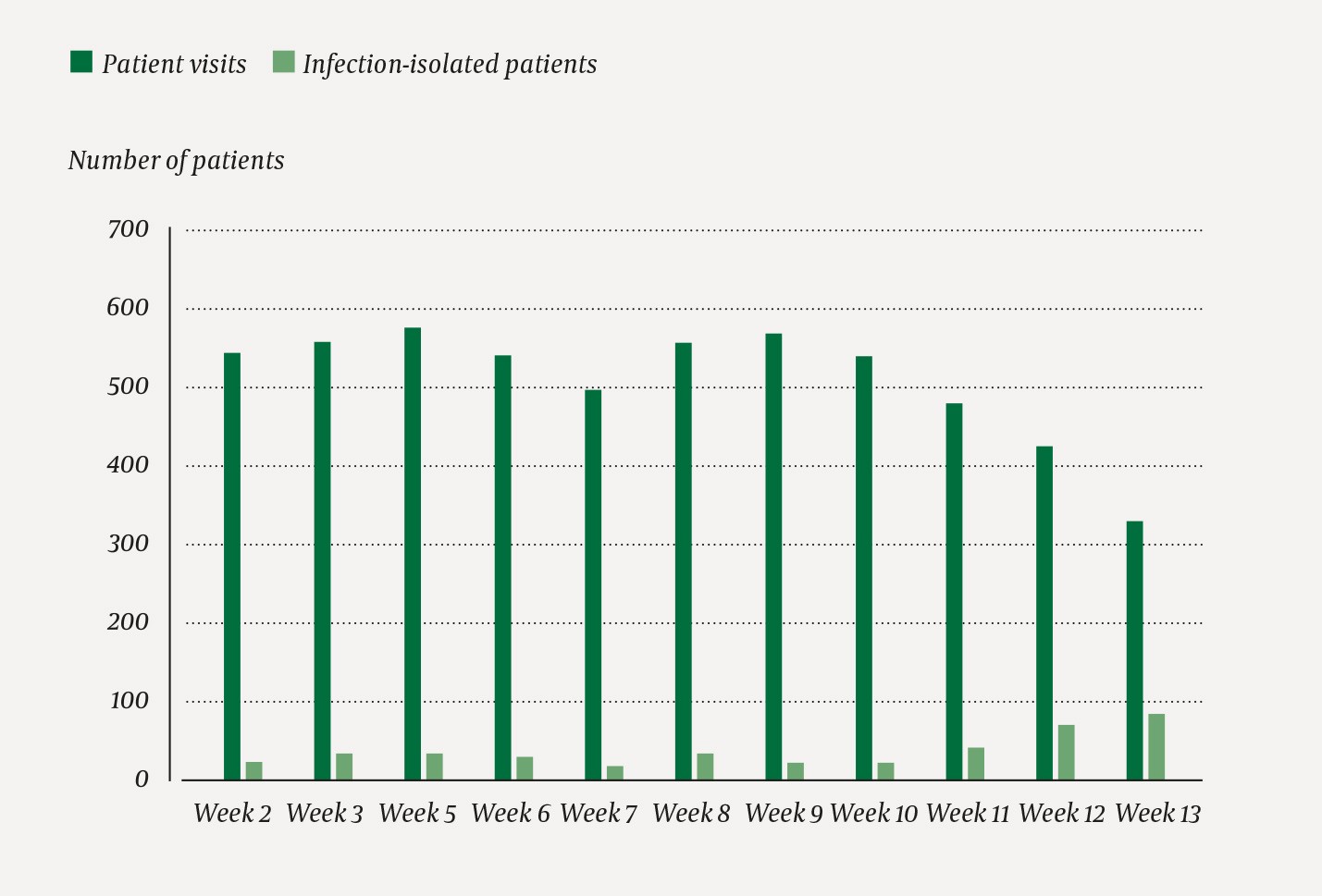
Figure 1 Overview of the total number of patients seen weekly in the Emergency Department at St Olav´s Hospital in the first quarter of 2020 and the weekly number of patients isolated in the Emergency Department in the same period because of suspected/potentially infectious disease.
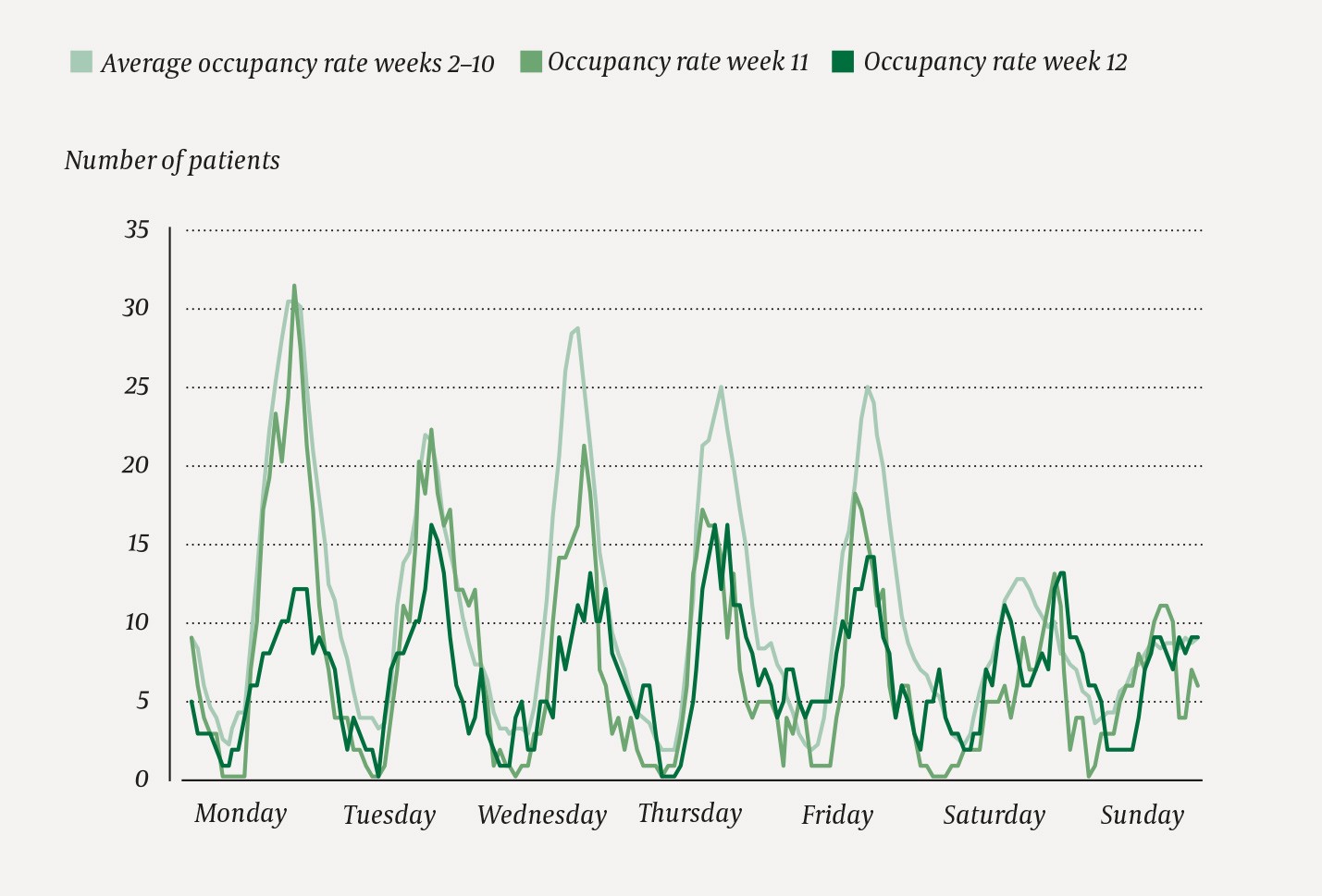
Figure 2 Number of inpatients in the Emergency Department at St Olav’s Hospital each hour on the hour in weeks 11 and 12 in 2020 compared with average visits in weeks 2–10 in 2020.
In week 12 there was a general reduction in acute patients in all medical areas. The reductions in patients in the areas medicine, surgery, orthopaedics and neurology were 98 (35 %), 49 (39 %), 16 (41 %) and 16 (40 %), respectively, compared with the averages for weeks 2–10. For urgency, there were reductions in red, orange, yellow and green of 23 (39 %), 84 (41 %), 87 (36 %) and 13 (48 %) patients. The number of outpatients treated at the clinic was reduced by 76 (47 %). There was no change in the number of patients admitted to the Intensive Care Department or Observation Unit (data not shown).
There was a marked increase in weeks 11 and 12 in patients who were isolated in the Emergency Department because of suspected/potentially infectious disease (Fig. 1). The average time spent by patients in the Emergency Department was 3 hours 14 minutes in weeks 2–10, 2 hours 52 minutes in week 11 and 3 hours 29 minutes in week 12. The time spent by patients in infection isolation was 5 hours 1 minute in week 12, despite the fact that the occupancy rate at the hospital in week 12 was 65 % (internal data from St Olav’s Hospital, PAS-rapporten Korpas database).
Discussion
We found a significant reduction in the number of patients referred to the Emergency Department early in the epidemic. A similar situation was reported during the first two weeks of the epidemic in Italy (5) and in China, where a sharp reduction was seen in the number of patients seeking emergency dental treatment (6). However, there are no studies that describe this trend in more detail. We saw a general reduction in the number of patients coming to the Emergency Department from week 11 already, without any medical disciplines standing out. Other European countries such as Belgium, France and Germany refer to unpublished data on a general reduction in the number of patients coming to the Emergency Department, particularly patients with conditions assumed to be less serious (7).
Our study revealed a similar reduction in the number of patients with low urgency and patients whose treatment would normally be fully dealt with in the Emergency Department. In Norway this may be because the Norwegian primary health service has largely dealt with these issues itself, or because the threshold for referring patients to the Emergency Department has risen now in a time of crisis. The primary health service makes sound clinical judgements that limit the inflow of patients. The fact that the inflow of patients is almost unchanged at the weekend, when GP offices are closed, provides support for this statement (Fig. 2).
An explanatory model for the pronounced fall that is greater cause for concern is that patients are delaying contacting their GP or phoning the emergency number for fear of becoming infected or of being an unnecessary burden on the health service. This fear is shared by emergency doctors in Belgium, the UK and France, among others. From Germany there are reports of a reduction in stroke and heart attack cases in the Emergency Department (7), and there have been similar anecdotal reports in Trondheim, Norway. Possibly in order to avoid being a burden on the health system, or for fear of infection, patients have suffered both stroke and heart attacks without seeking help within treatment time window.
It is crucial that the primary health service acts as gatekeeper and filter for the specialist health service. At the same time, the message must be communicated to the public that people must seek medical assistance as early as possible in the event of symptoms of what may be a serious illness.
The aim during the pandemic is for all patients to have safe, high quality assessment and treatment at the Emergency Department, no matter what the situation. This is challenging, as assessment and treatment of isolated patients takes longer and requires more resources. A rapid test for COVID-19 in the Emergency Department would probably reduce clarification time in the Emergency Department. The greatest potential challenge, however, is to have a sufficient number of health personnel (2). Although no Emergency Department staff are in quarantine at present, there is a high risk of health personnel becoming unavailable. It is the calm before the storm in Trondheim, and the Emergency Department is preparing for a large influx of patients with suspected COVID-19.
