Excision of skin lesions takes place regularly in general practice. The procedure is simple, but correct execution depends on a knowledge of skin anatomy and basic surgical principles.
This article presents indications for excision of skin lesions and a recommended method based on clinical experience and relevant literature. The method can be used on both pigmented and non-pigmented lesions. Seborrheic keratoses are not discussed (1). The contents of the article apply to the primary health service.
Indication
Skin lesions are excised with a view to obtaining a histological diagnosis. Pigmented naevi and benign, non-pigmented lesions are thus distinguished from premalignant and malignant lesions (such as malignant melanoma, basal cell carcinoma and squamous cell carcinoma).
The indication for excising a skin lesion is based on the patient’s medical history and the clinical examination. The ABCDE rule is used to assess pigmented lesions (1). Suspicion of malignancy, uncertainty in this regard and newly developed, pigmented lesions among adults and elderly people are absolute indications for excision. Pigmented naevi, which are benign collections of melanocytes in the skin (2), should not be excised. However, if a pigmented naevus causes substantial discomfort – either functional (makes shaving difficult, gets caught in a waistband/bra strap) or psychological (particularly as a cosmetic blemish) – it can be excised on a relative indication (3). Patients must be informed that all surgery results in scars.
The primary health service plays a key role in patients’ perception of pigmented lesions. Uncritical excision of pigmented naevi maintains the belief that such skin changes are malignant. It also places a burden on the pathology service and many patients get disfiguring scars. Patients must be informed which skin changes should, and which should not, be excised.
Age limit
There is no absolute upper/lower age limit. In cases of pigmented naevi with a relative indication for excision, it is an advantage to wait until the patient is fully grown (16–18 years), as scars on a growing body may become broad or hypertrophic. Skin changes suspected of malignancy must be excised irrespective of age.
Anatomical principles
Tension lines
The microscopic structure and tension of the skin depend on age and location. These factors contribute to the natural contours and wrinkles of the skin – often called relaxed skin tension lines (RSTL) (4). The excision is sited in or parallel to these wrinkles. This results in less tension in the closing, faster healing and neater scars. More than 30 skin tension guidelines have been developed. The most widely known of these are Langer’s lines (5), but they are not necessarily the best guide (4–6). We recommend trying oneself to determine the tension of the skin – by having the patient move the body part in question and/or by using the pinch test. In the latter, the skin is pinched in different orientations. As a rule, the natural wrinkles are perpendicular to the pinch orientation that is easiest to carry out. This is usually transverse to the longitudinal orientation of the underlying musculature. We recommend making vertical incisions on the extremities, with the exception of around joints, where there are distinct wrinkles in some places.
Anatomical danger zones
The face and neck have anatomical danger zones where there is a risk of damaging underlying structures and/or creating an undesirable pull on the eyelid or lips/corners of the mouth. Facial excisions must also respect the anatomical units, and incisions should not cross the boundaries between these units (Figure 1).
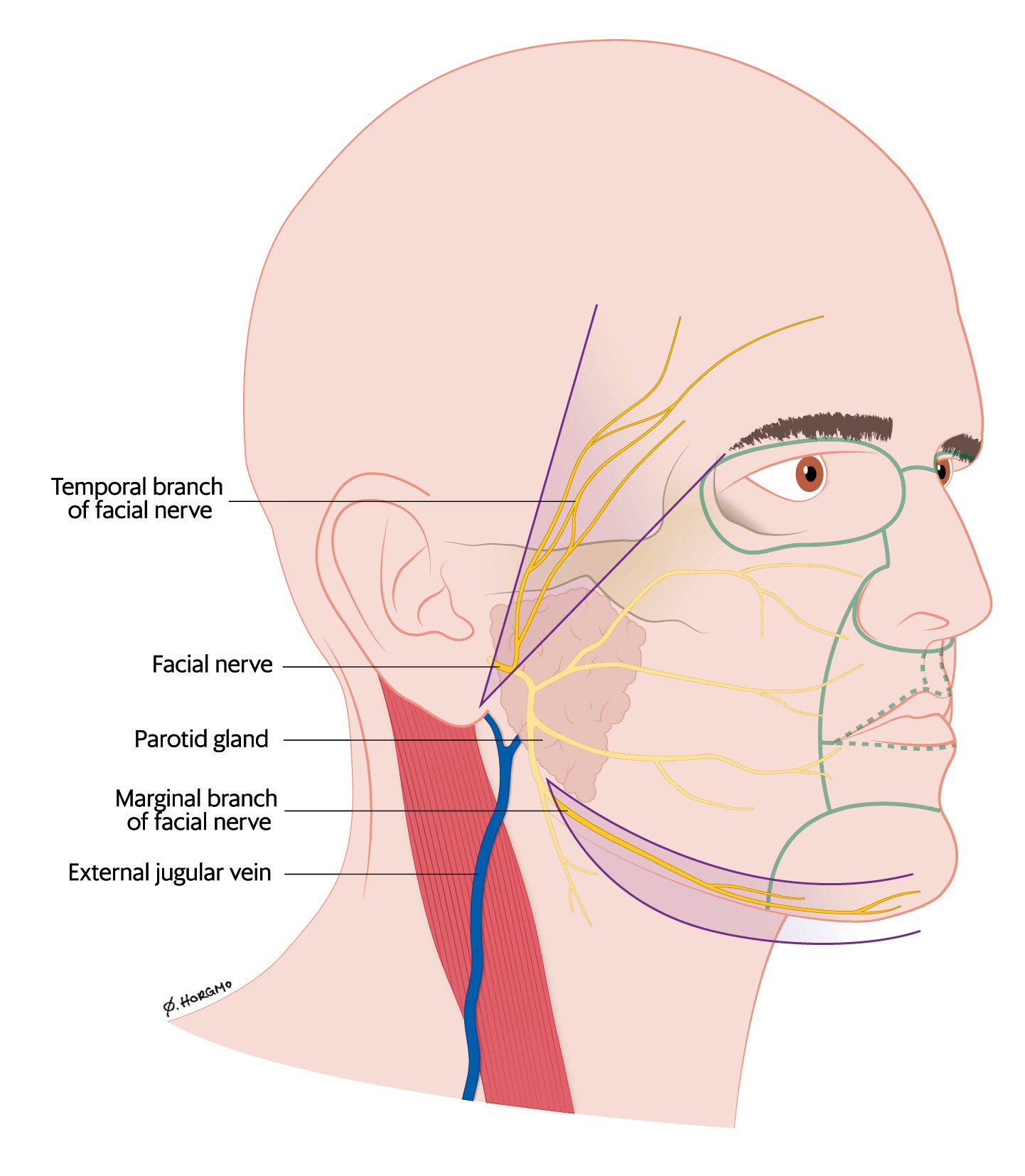
Figure 1 Temporal branch of facial nerve, marginal branch of facial nerve and external jugular vein. The boundaries between important anatomical units in the face are marked with green lines. Illustration: Øystein Horgmo, University of Oslo
In the face, it is important to be aware of two branches of the facial nerve, the temporal and the marginal. These nerve branches are located more superficially than other branches and may be damaged by surgery in the areas shown in Figure 1 (7). The external jugular vein is located very close to the surface in the neck.
The upper body and extremities are regarded as safe areas for excising skin lesions. However, there is risk of disfiguring scar formation on the shoulders, back and the extensor side of joints.
Basic surgical principles
Macroscopic free margin. The skin lesion is excised with a macroscopic free margin of 2 mm (8). Even in cases of lesions suspected of malignancy it is not necessary to add extra margins for the primary excision. If dysplasia is found, the patient will be referred for extended excision regardless (9).
Fusiform markup. A fusiform markup, as illustrated in Figure 2, is desirable. This markup prevents surplus skin along the excision, referred to as ‘dog ears’.
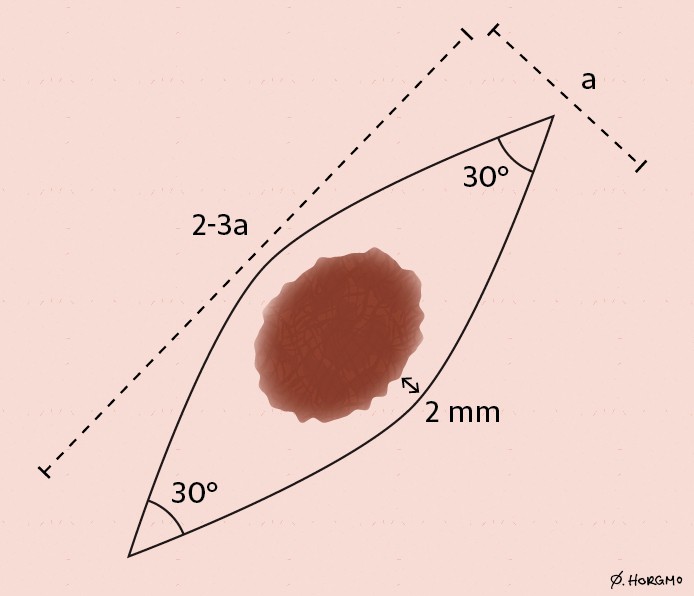
Figure 2 Fusiform markup with macroscopic free margin (2 mm). Ratio 3:1 and acute 30o angles. The 3:1 ratio is not absolute, and can be adjusted down to 2:1 if this is considered sufficient. Illustration: Øystein Horgmo, University of Oslo
Full skin excision down to subcutaneous fat. The excision should go down to subcutaneous fat corresponding to the whole markup (10). There are many reasons for this: Whole skin specimens yield better histological assessments, reduce the risk of recurrence, remove dermal tissue that could make closure difficult, present the transition between dermis and subcutis – which is the recommended layer for undermining (11) – and provide wound edges that are sufficiently thick for suturing in two layers.
Applying the scalpel. The scalpel is directed perpendicularly downwards, or 10o outwards in relation to the markup. Avoid making a boat section, where cutting is inwards (like the keel of a boat) (1). The scalpel should be drawn with a smooth movement from start to end on each side. Use the point of the scalpel in the angles and the curved cutting edge of the scalpel in the middle. Repeat the cutting on alternate sides until you reach the fatty tissue. Lift the one corner carefully up with forceps/skin hook and cut under the specimen such that it is of even thickness. A thin layer of fatty tissue at the base of the specimen is desirable.
Undermining. Undermining is a technique whereby the skin is freed from the underlying tissue. In this way more mobile wound edges are obtained and less tension in connection with closing (11). This is done either by blunt (separate with blunt dissection scissor) and/or by sharp dissection.
Undermining is done just under the dermis to preserve the skin’s blood supply. Normally it is sufficient to go about 5–10 mm from the edge of the excision (including the corners) and out into surrounding tissue. It is important to be aware that the dermis differs in thickness on different parts of the body. On the back it is typically 4–5 mm.
Suturing in two layers. For a good cosmetic result, it is very important to suture in two layers (11). The tension is then distributed over two levels and more sutures. In addition, the dead space at depth is reduced, and accordingly the risk of infection. The larger the excision, the more important it is to suture in two layers. For excisions of more than 10–15 mm, it is often essential (1). With single layer suturing there is a risk of a wide scar with transverse scarring stripes (due to a tight suture thread that suppresses the blood supply to the skin) (10). A layer of interrupted skin sutures is sufficient for excision of skin lesions of 5 mm or less, however.
Choice of sutures. We recommend using absorbable polyfilament sutures with a small needle (semicircular) for the dermal sutures and non-absorbable monofilament sutures for the epidermal sutures. A polyfilament suture is a braided suture that makes stronger knots. A monofilament suture may seem rather stiff, but slides easily through tissue and causes less trauma to the tissue. The smooth surface also reduces the risk of infection (12).
The thickness of the sutures depends on the location. 4.0 is used widely in skin surgery. The same thickness is normally used for the two suture layers. Alternatively, a thicker suture can be used for the dermal sutures (for example 4.0 for the dermal and 5.0 for the epidermal layer).
Method
Equipment. You need a pair of (non)sterile gloves (13), marker pen, chlorhexidine, sterile gauzes, a syringe (5 ml), two cannulas (blue/orange), Xylocaine 0.5–1 % with adrenaline, sterile instruments (scalpel handle, scalpel blade no. 15, needle holder, forceps, blunt/sharp dissection scissors, suture scissors and possibly skin hook), absorbable polyfilament suture, non-absorbable monofilament suture, sterile saline in sterile container, brown skin tape, self-adhesive bandage, specimen jar with formalin and histology submission form.
Markup. Determine the tension direction and do a fusiform markup (Figure 2). Aim for a macroscopic free margin of about 2 mm. The markup can be done with a non-sterile marker pen.
Sterility. Wash your hands. Put on (non)sterile gloves. Damp a gauze with chlorhexidine and swab the whole area. Chlorhexidine/alcohol must air-dry. Lay out all the equipment on a sterile cloth/ changing set. Drape if possible.
Local anaesthetic. Draw up local anaesthetic and then switch the cannula (one for drawing up and one for injection). Inject the local anaesthetic in the upper layer of the dermis so that the skin rises and forms a weal. As a rule, aspiration is not necessary, but should be carried out in the proximity of major arteries and veins (for example on the hand, in the elbow and on the neck). The maximum adrenaline effect is attained after 6–8 minutes.
Excision. Excise the skin lesion as described above. Bleeding can be compressed for 15–20 seconds (or diathermised). Suture marking of the specimen is not necessary.
Undermining Undermine the wound edges as described above. Try not to vary the level of the undermining.
Suturing. The dermal sutures are applied first. The sutures should be inverted (see video) so that the knots are as deep as possible. Start from one of the sides. After the dermal sutures have been applied, the interrupted skin sutures are applied in the epidermis. Normally, fewer sutures are placed in the dermis than in the epidermis (for example, two at depth and three at the surface), and the different sutures are preferably applied alternately. The dermal sutures reduce the tension, while the epidermal sutures provide precision at the surface.
Dressing. Swab with sterile saline and dry carefully. Apply brown paper tape over the linear closure. Then cover with self-adhesive dressing.
Histology All excised skin lesions must be sent for histological examination.
Information for patients
The surgical site must be kept dry for 2–3 days. The patient must be informed about changing dressings, removal of sutures and reasons for getting in contact again. Standardised information leaflets are recommended. Inform the patient about the anticipated waiting period for histology results.
Alternative procedures
Punch biopsy can be used for small skin lesions provided that the whole lesion is removed in one punch (1). Punch biopsies of more than 5 mm are not advisable, as circular excisions of increasing size may cause dog ears.
Referral
Cases of skin cancer are rising (14), and treating skin cancer patients makes heavy demands on hospitals’ outpatient/day-case surgery resources. Thus diagnosis of skin lesions by the primary healthcare service is desirable.
Non-pigmented lesions suspected of malignancy should be excised/biopsied by a general practitioner or referred to a dermatologist/surgeon. On suspicion of malignant melanoma, the skin change should be excised or referred (15). If there is a relative indication for excision, the skin lesion can be excised by a general practitioner or referred to a specialist. The indication must appear clearly in the referral. Pigmented naevi with no indication for excision should not be referred.
The great majority of skin changes less than 1 cm in size can be closed directly and thus excised in the primary health service by means of the demonstrated method. A lower threshold for referrals is recommended for skin changes located in the risk areas of the face (Figure 1).
