The contract GP scheme was established in Norway in 2001. The reform entailed a greater responsibility conferred on the municipalities for ensuring medical services to the population, while the inhabitants had the opportunity to choose a permanent GP. In a full curative position, the contract GPs could be charged with the responsibility for a list of 1 500 persons as a minimum – the so-called ‘normative figure’ (1). Although the reform is considered a success, concerns about recruitment and the sustainability of the system have arisen in recent years. Changes that have occurred both inside and outside the health services have impacted on the tasks and workloads of the GPs. The population is ageing, more people are living with chronic diseases, responsibilities are transferred from the specialist to the primary healthcare service, and people have higher expectations regarding the healthcare service (2–4).
In this situation, a group of GPs established the grassroots initiative ‘Fastlegeordningen 2.0 [Contract GP scheme 2.0], also known as ‘the Trøndelag rebellion’, in 2017 (5). The founders of the initiative also work as lecturers on the medical study programme of the Norwegian University of Science and Technology (NTNU). Their goal was to preserve and strengthen the contract GP scheme by raising it on the national agenda. The group recognised a need for updated knowledge on the working conditions and roles of the contract GPs in today’s health services, and launched a mapping study among all Norwegian GPs.
Previous research on the working situation of GPs has followed various traditions. One main basis is registry-based research, which shows that a strong primary healthcare service and continuous doctor-patient relationships are advantageous, both in terms of resource use and reduced mortality (6, 7). At the descriptive level there are publications based on diagnostic codes and reimbursement rates (8). Other studies are based on ‘audit’, meaning manual registration of a given topic as a basis for more detailed analysis and quality development (9). In recent years we have also seen qualitative studies of specific issues (10). A number of international books, articles and reports highlight the generalist perspective and the humanist and complex nature of general practice medicine (11, 12).
The objective of this study was to identify selected issues that the doctors encountered in the course of a typical, clinical day in their practice.
Material and method
The study is based on a collaboration between doctors in clinical practice, professional associations and academia, and is inspired by the primary health service researcher Trisha Greenhalgh’s recommendation of knowledge development on the basis of new collaborative alliances (13). A project group consisting of GPs and academic staff at NTNU devised an online questionnaire in the Netigate application. In the questionnaire, which consisted of two parts, the respondents were asked to register their activity on a full day of their own choosing in their practice, as well as the frequency of 22 pre-defined issues (5, see also Box 1). The second part of the study covered the doctors’ general perception of their work situation. The results from this part as well as the general registration of activities have been published previously (5). The survey was submitted to the Institute for the Study of the Medical Profession and the legal department of the Norwegian Medical Association, and has been pilot tested on experienced GPs.
Box 1 Questionnaire: introduction to the questions and example of issues
In the questionnaire, the questions in the descriptive part of the study were introduced with the following text:
‘In this section we wish to elucidate a sample of issues/topics that contract GPs encounter regularly. The list is not intended to be exhaustive, and some topics may overlap. Some of these are national priorities or topics that are regularly the subject of public debate.’
Issues were exemplified as follows:
‘The patient brings a checklist (dizziness, blood pressure, prescription renewals, check of moles) with four different issues to address. In addition, the doctor has some suspicions regarding alcohol consumption and stress in the home environment. In this example, this will generate a total of six issues.’
The Norwegian Medical Association sent unique links to the study to all GPs with registered email addresses. In addition, doctors were encouraged through social media to contact us if they had not received an email with an invitation to participate in the study. The data collection was undertaken in the period 28 February – 8 April 2018. One reminder was sent. The invitation to participate in the study contained a brief description of the content, objective and privacy safeguards, instructions to select an ordinary, full day of practice outside out-of-hours duty, a unique link to the questionnaire and a checklist for continuous registration of activities and issues on the selected day. The study was anonymous. Background variables such as geographical location, sex, age, specialty and form of practice were also requested.
The data were presented descriptively with calculation of averages in the SPSS software package, version 26. To take account of differences in the number of consultations, the incidence of issues presented by patients was also reported as a percentage of the GPs’ total number of consultations on the day. Differences between women and men GPs were analysed by inspecting the confidence intervals of the average frequency of each individual issue.
Data that could point to the identity of individuals or small groups of doctors were not analysed. The study was submitted to the Norwegian Centre for Research Data (NSD) and the Regional Committee for Medical and Health Research Ethics (REK Central Norway) and assessed as not subject to approval (reference 688223/22.08.19).
Results
Of 4 784 GPs registered in the spring of 2018, we received complete responses from 1 032 (21.6 %). The participants are described in more detail in Table 1. The background variables have been published previously (5). The representativeness of the sample is described in the discussion chapter.
Table 1
Characteristics of the participating GPs.
|
|
|
Participants
|
|
|
Women GPs
N = 529
|
Men GPS
N = 502
|
|
|
n
|
%
|
n
|
%
|
|
|
Total number of consultations, day X
|
|
10 216
|
|
10 552
|
|
|
|
Average number of consultations, day X
|
|
19.3
|
|
21.0
|
|
|
|
List size
|
|
529 000–581 000
|
|
552 200–602 000
|
|
|
|
Average list size
|
|
1 000–1 099
|
|
1 100–1 199
|
|
|
Age group (years)
|
|
|
|
|
|
|
< 40
|
|
213
|
40.3
|
197
|
39.2
|
|
|
40–49
|
|
171
|
32.3
|
148
|
29.5
|
|
|
50–59
|
|
97
|
18.3
|
74
|
14.7
|
|
|
≥ 60
|
|
48
|
9.1
|
83
|
16.5
|
|
|
Total
|
|
529
|
100.0
|
502
|
100.0
|
|
Municipality size (inhabitants)
|
|
|
|
|
|
|
< 5 000
|
|
48
|
9.1
|
32
|
6.4
|
|
|
5 000–10 000
|
|
40
|
7.6
|
45
|
9.0
|
|
|
10 000–50 000
|
|
207
|
39.1
|
204
|
40.6
|
|
|
50 000–100 000
|
|
93
|
17.6
|
70
|
13.9
|
|
|
> 100 000
|
|
141
|
26.7
|
151
|
30.1
|
|
|
Total
|
|
529
|
100.0
|
502
|
100.0
|
|
Experience as a GP
|
|
|
|
|
|
|
< 5 years
|
|
163
|
30.8
|
133
|
26.5
|
|
|
≥ 5 years
|
|
366
|
69.2
|
369
|
73.5
|
|
|
Total
|
|
529
|
100.0
|
502
|
100.0
|
|
Specialty
|
|
|
|
|
|
|
Specialist in general practice
|
|
333
|
62.9
|
336
|
66.9
|
|
|
Specialty registrar or locum
|
|
196
|
37.1
|
166
|
33.1
|
|
|
Total
|
|
529
|
100.0
|
502
|
100.0
|
In total, these 1 032 doctors registered 20 768 consultations. On average, each GP conducted 20.1 consultations with a patient present on the selected day, as well as a number of other contacts. Women doctors conducted somewhat fewer consultations (average 19.3; 95 % CI 18.9–19.7) than their male colleagues (average 21.0; 95 % CI 20.6–21.5).
In total, the in-person consultations covered 44 343 medical issues, equivalent to 43 medical issues during the day and 2.1 issues per consultation.
Table 2 (see tidsskriftet.no) describes the 22 pre-defined issues that the GPs registered on the chosen practice day. Figure 1 shows the 12 most frequent issues of these 22, distributed by women and men doctors.
Table 2
Incidence of 22 pre-defined issues, formulated as in the questionnaire. The table shows average incidence and percentage of the GPs’ total number of consultations on a typical, full day of practice.
|
Issue
|
Average incidence
|
Proportion (%)
|
Number of responses
|
|
The patient had a complex disease picture with multiple diagnoses/ drugs (multimorbidity)
|
5.81
|
29.1
|
1 028
|
|
Mental ailments and disorders
|
4.30
|
21.8
|
1 026
|
|
The patient’s problem/reason for contact was explicitly or potentially related to stresses and strains of life
|
3.62
|
18.2
|
1 022
|
|
Issues for which my most important contribution was to be a supporter/life coach
|
3.06
|
15.3
|
1 013
|
|
Chronic pain
|
3.02
|
15.3
|
1 024
|
|
I discussed preventive measures relatively thoroughly with the patient (with or without prescribing any drugs)
|
2.59
|
12.8
|
1 008
|
|
We were unable to address all the issues in today’s consultation, and a new appointment was made
|
2.30
|
11.4
|
991
|
|
The patient presented a problem that includes cancer among its differential diagnoses
|
2.12
|
10.5
|
1 001
|
|
Complex health challenges/issues related to ageing (e.g. dementia, rapid functional impairment)
|
1.48
|
7.3
|
990
|
|
Gynaecological issues and advice on contraception, not pregnancy-related
|
1.30
|
6.5
|
985
|
|
The patient presented a strong desire/request for an examination/test which was probably not medically indicated
|
1.29
|
6.3
|
980
|
|
Pregnancy check-up and other pregnancy-related contacts
|
1.08
|
5.4
|
972
|
|
Follow-up of cancer diseases
|
1.06
|
5.2
|
970
|
|
Complex health challenges/issues in children and adolescents (i.e. not clinically well-defined issues such as infections etc.)
|
1.01
|
5.0
|
977
|
|
The patient’s health problem is or may be the result of experience of violence/abuse/neglect
|
0.97
|
5.1
|
947
|
|
The patient’s problem/reason for contact was explicitly or potentially linked to alcohol abuse/addiction
|
0.84
|
4.1
|
963
|
|
Disagreement or difficult discussion concerning prescribing of class A or B drugs
|
0.79
|
3.9
|
949
|
|
Disagreement or difficult discussion concerning sick leave for a patient
|
0.59
|
2.9
|
942
|
|
The patient has experienced war and/or a dangerous flight (refugee/asylum seeker)
|
0.54
|
2.7
|
919
|
|
The consultation was conducted with the assistance of an interpreter
|
0.48
|
2.3
|
923
|
|
There was a significant language barrier between me and the patient, with no interpreter present
|
0.45
|
2.2
|
931
|
|
I experienced threatening comments or demeanour from a patient or his/her next of kin
|
0.15
|
0.7
|
905
|
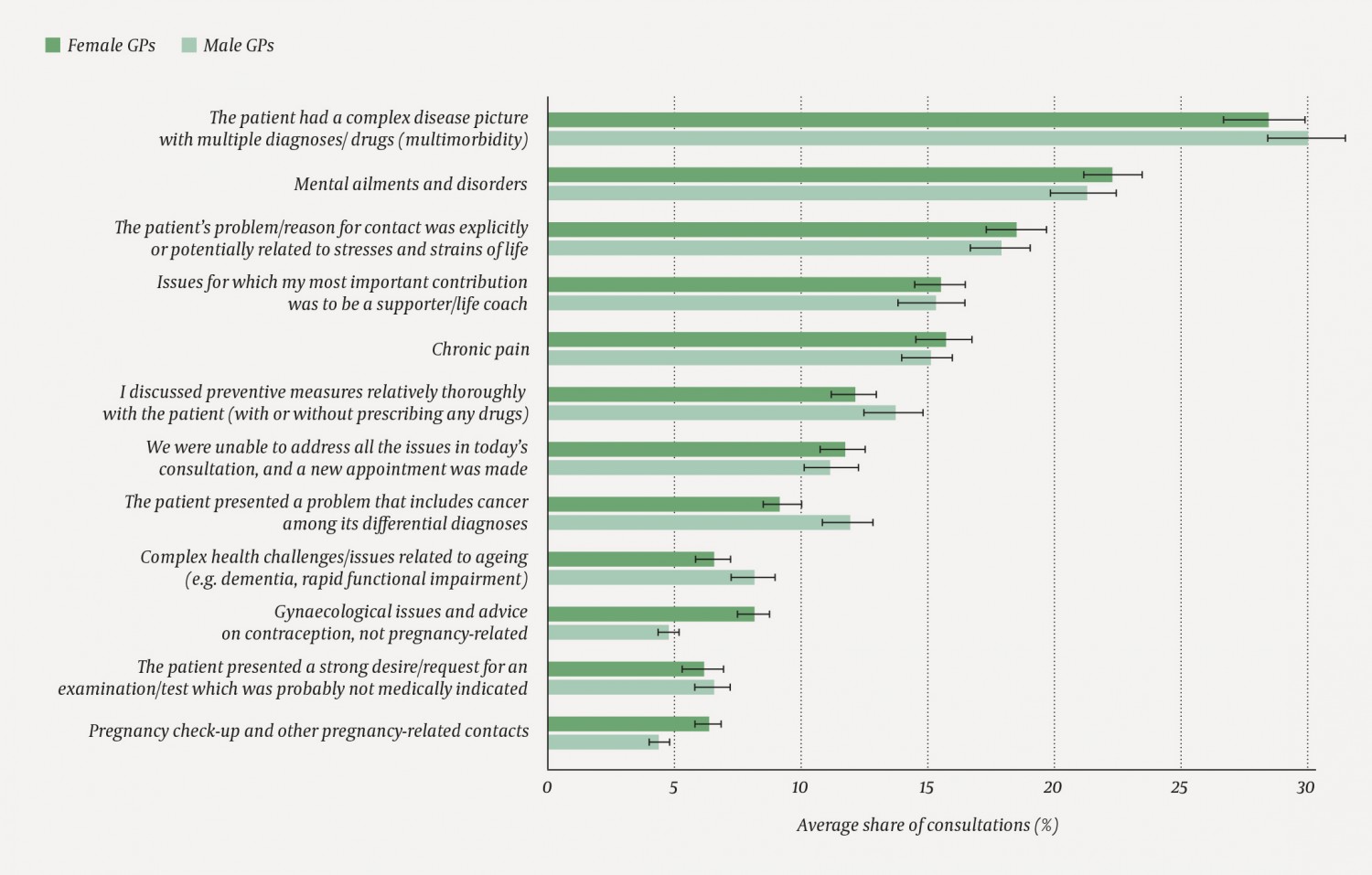
Figure 1 Incidence of the 12 most frequent pre-defined issues, by the doctors’ sex. The incidence is shown as a percentage of the GPs’ total number of consultations on the day of study, with a 95 % confidence interval.
Women GPs encountered issues linked to gynaecology 1.58 times per day on average (95 % CI 1.45–1.70), compared to 0.99 for men doctors (95 % CI 0.91–1.07). The same trend was observed for pregnancy-related issues, of which women doctors reported 1.23 issues per day on average (95 % CI 1.13–1.34), compared to 0.92 for men doctors (95 % CI 0.84–1.01). The opposite trend was observed for issues linked to cancer, of which men doctors handled on average 2.5 issues per day on average (95 % CI 2.28–2.72), whereas women doctors reported an average of 1.76 (95 % CI 1.61–1.90).
Discussion
The study shows that on average, Norwegian GPs conduct approximately 20 consultations in the course of a clinical working day. A number of other contacts and tasks can be added to these. Many of the 22 pre-defined clinical issues occurred frequently. We found relatively small differences between men and women GPs.
The study provides detailed insight into the day-to-day work of 1 032 GPs in Norway. We consider the rate of participation to be adequate, given the scope of the survey. On the other hand, the participants constitute no more than 21.6 % of the total population of GPs. The distribution of participants accords well with the GP statistics published by the Directorate of Health (5), with the exception of Trøndelag county, where our sample had more participants (5). Both sexes and different age groups were well represented in the study, although with a certain overrepresentation of younger doctors (30–39 years). In light of the total number of responses and the distribution of the respondents in terms of county, municipality size, sex, age, specialty and experience, we consider the sample to be suited for elucidating the study’s research questions.
The study was undertaken in a period of concern and strong engagement among Norway’s GPs. There is a possibility that the most overburdened doctors did not prioritise participating and therefore are underrepresented in our study. On the other hand, doctors who did not perceive their job situation as especially challenging may have been less motivated to participate. The sample is likely to contain the most engaged GPs, and we cannot exclude the possibility that the participants in general wished to help document large workloads and a large number of challenging tasks. Moreover, we assume that the mood of professional activism may have coloured the responses to the subjective part of the survey (5) to a greater extent than in the prospective registration of specific presentations and tasks. The doctors included in our study described 2.1 issues per consultation on average. This is unlikely to be an overestimate, since a Norwegian study from 2015 found 2.6 issues per consultation (14). It can be added that one strength of our study was that the questionnaires were distributed with a unique link to each respondent, which prevented multiple responses from the same source.
The 22 pre-defined issues in the study can in no way provide a full overview of the medical content of the GPs’ working day. First, the study had little focus on defined clinical reasons for contact, which must be assumed to occur relatively frequently. Second, certain complex consultations may have been categorised more than once among the 22 topics (for example, both as multimorbidity and as disagreement over prescribing). Many essential and complex tasks were not included in the questions, for example supervision of younger colleagues in parallel with the GP’s own clinical activity. Nor did the study document consultations initiated by third parties, such as insurance companies, or follow-up of results from examinations undertaken by private providers on the patient’s own initiative.
The doctors in our study reported that mental disorder was a topic in 22 % of the consultations. Based on diagnostic codes, the evaluation of the contract GP scheme in 2019 referred to mental disorders in 10 % of the consultations (2). However, in the diagnostic coding of cases involving complex clinical issues, diagnoses of mental disorders may be omitted in favour of other relevant diagnoses in the patient’s symptom profile. This may explain some of the discrepancy between the studies. The Norwegian study from 2015 showed an incidence of mental disorders of 26 % (14), which is closer to our finding. Irrespective of the exact prevalence, public policies with regard to the handling of mental disorder may have a considerable impact, both on the GP’s working day and on the total effectiveness of the health services (15). Examples of such policies include clinical guidelines, prioritisation manuals and the introduction of standard pathways for mental illness (10, 16–18).
The Coordination Reform of 2012 (17) shone a light on the role of GPs in preventive medicine. The GPs in our study registered having discussed preventive measures relatively thoroughly in 13 % of their consultations. In comparison, the Norwegian study from 2015 found preventive activity in 38 % of all consultations (14). The difference may be due to the specification of thoroughness in our question. Moreover, elements of prevention can be implicit in many clinical encounters, without the GP actively highlighting it. A recent Norwegian report (19) points to a gap between what the authorities have expressed in their regulations and assessments in terms of expectations for health promotion and preventive work in general practice on the one hand, and what the GPs report about their activities on the other. It is further pointed out that GPs have insufficient competence in preventive medicine and health promotion. In general, we see a need for a more detailed mapping of GPs’ role as preventive health agents, also in a wider perspective that devotes attention to the health-related importance of human relationships and the GP’s unique insight into these (20).
In line with studies from comparable countries we found that on a daily basis, Norwegian GPs assess for potential cancers and follow up patients after a cancer diagnosis, a responsibility which is increasingly delegated to them by the hospitals (21, 22). The study also shows how sensitive and potentially conflictual situations regularly occur in the GPs’ practice, including issues associated with addiction and alcohol (23, 24), prescribing of class A or B drugs, assessment of indications for examination or sick leave in doubtful cases, and threatening comments or demeanour by a patient or accompanying relative.
A high prevalence of multimorbidity and other challenging clinical presentations in the primary healthcare service indicates that a key task for the GP is to undertake good overall assessments and set the right priorities (3, 4, 25–27). This applies to previous diagnoses and ailments, social conditions, use of medicinal and recreational drugs, if relevant, concerns, preferences and inherent resources (28). To this can be added stressful life experiences that have a significant impact on health over the life course (20). Personal knowledge can be gradually established and the doctor-patient relationship strengthened through a number of clinical encounters, preferably also consultations involving simple issues. As noted above, good clinical continuity is associated with lower rates of mortality (6, 7).
It was recently documented that the working hours for Norwegian GPs amount to 55.6 hours per week on average (29). Combined with the frequency of challenging, complex issues that we have described here, a picture emerges of a working situation that could become untenable in the long term (10). In the public evaluation, nearly 70 % of the GPs reported suffering from work-related stress to a large or very large extent that compromised their quality of life (2). Stress in the GP can also compromise the quality of the clinical dialogue, especially in emotionally charged situations where cool-headedness and sufficient time are crucial for establishing trust, a shared understanding and good self-care on the part of the patient (27, 30, 31). Ten per cent of the GPs have reported to their municipalities that they wish to stop working as contract GPs, citing a large workload as the main reason (2). In other words, it is urgent to identify important measures that can make the working situation of GPs more manageable and sustainable. A recent European multicentre study shows that flexible working, frameworks that encourage competence development and stable doctor-patient relationships are key factors for the GPs’ well-being (32). It would also be natural to take a closer look at the extent to which current basic and advanced training programmes help prepare future doctors for the challenges of the primary healthcare service. In particular, we call for updated knowledge on how inexperienced GPs perceive their working situation.
Conclusion
On average, Norwegian GPs undertake 20 consultations in the course of a full clinical day of practice, involving twice as many patient issues. The study presents an updated picture of the total workload, complexity and bustle of a Norwegian GP practice. We observe that the contract GP encounters a high incidence of complex presentations and mental ill-health, where the doctor often functions as the patient’s life coach.
