Measures targeting children and adolescents in Norway have attracted great attention since the pandemic outbreak of SARS-CoV-2, the virus that causes the disease COVID-19. Children and adolescents can be infected by SARS-CoV-2 and become ill, but their symptoms appear mainly to be substantially milder than in adults and elderly people (1). The incidence of complications and hospitalisations is also low among children and adolescents (2).
Screening of young children in Iceland reveals a low incidence of SARS-CoV-2 in groups both with and without respiratory tract symptoms (3). Similar findings have been reported in a non-peer-reviewed article from Italy (4). So far, there have been few reports of outbreaks of infection in day-care centres and schools (5). Norwegian day-care centres and schools were closed in mid-March 2020, as one of a number of measures to prevent the spread of infection. As of 12 May 2020, 169 countries had closed all schools, affecting over 1.2 billion pupils (6). One review assesses the effectiveness of this measure as low (5) and another study considers it equivocal (7), but its negative consequences are considerable (8).
In all countries where data are published, and in one European register, a small percentage of children and adolescents are found among all those with confirmed infection (1, 3, 9–11). Little is known about whether children with chronic diseases are more susceptible. Knowledge of possible risk factors is important for enabling evidence-based advice to be given about targeted measures for and shielding of at-risk groups. The Norwegian Institute of Public Health in consultation with the Norwegian Society of Paediatricians has issued general (12) and more specific (13) advice on preventive measures for groups with underlying conditions, based on the best available evidence.
This article presents data from the initial period of the epidemic, with a description of the incidence of confirmed SARS-CoV-2 in the age group 0–19 years, both for the age group as a whole and specifically for children and adolescents with underlying conditions.
Material and method
In this register-based study, we use data from the Norwegian Patient Registry (NPR), the Norwegian Registry for Primary Health Care (NRPHC) (14) and the Norwegian Surveillance System for Communicable Diseases (MSIS).
NPR is an administrative database that contains data on activity at all publicly funded hospitals and clinics. Reporting to NPR is mandatory, and forms the basis for reimbursement in the specialist health service. The registry contains identity and ICD-10 codes (International Classification of Diseases). NRPHC covers other claims for reimbursement from primary health service therapists to the state. The ICPC-2 (International Classification for Primary Care) code system is used for claims for reimbursement. MSIS receives regular reports from microbiology laboratories on confirmed SARS-CoV-2 infections. Population data were obtained from Statistics Norway’s website (population data as of 1.1.2020).
The Norwegian Directorate of Health received data from MSIS and the Norwegian Institute of Public Health on all individuals who had tested positive for SARS-CoV-2 between 1 March 2020 and 13 May 2020. MSIS data were linked to data from NPR and NRPHC in the Directorate of Health’s Health Register Department with the aid of project-specific serial numbers that were common to all three registries. Extraction and linking of data and compiling of statistics were conducted with the aid of the database tool SQL Server Management Studio (SSMS, Microsoft) and the statistics tool R (16).
The analyses were conducted on aggregated data for maintaining surveillance of the pandemic in Norway and of groups that are particularly vulnerable to the disease.
Definitions
We defined seven groups of underlying conditions that might increase the risk of contracting SARS-CoV-2 or of serious outcomes in children and adolescents. These groups were identified on the basis of evidence on COVID-19 from other countries and of the risk of influenza disease and complications, and on general knowledge regarding the course of diseases and possible effects on the immune system that may result in increased susceptibility to infection (15).
We used NPR data for the period 2008–19 and NRPHC data for the period July 2016–March 2020 (all available data) to determine whether a person belonged to one or more of these groups. Table 1 shows which codes in ICD-10 (primary and secondary diagnoses) and in ICPC-2 formed the basis for the definitions. NPR and NRPHC have data from the National Population Registry Office for all persons in the registers. We removed data on all persons registered as deceased or emigrated as of 1 March 2020.
Table 1
Prevalence of diagnosis groups with chronic diseases in the population aged 0–19 years (n = 1 248 749).
|
Diagnosis
|
ICD-10 codes
|
ICPC-2 codes
|
No. (%)
|
|
Asthma
|
J45, J46
|
R96
|
30 259 (2.4)
|
|
Neuromuscular disorders (cerebral palsy, congenital malformations of the nervous system, muscular diseases)
|
Q00–07
G80–83
G70–73
|
L82
N81, N85
N99
|
14 320 (1.1)
|
|
Rheumatoid disorders and inflammatory bowel diseases
|
M05–09
K50–52
|
L88 D94
|
8 051 (0.6)
|
|
Chromosomal abnormalities
|
Q90–99
|
A90
|
4 732 (0.4)
|
|
Chronic cardiac/pulmonary disease other than asthma
|
Q20–28, I40–43, I50, Q30–34, J44, J47, E84
|
K73
R79, R95, R99
|
4 119 (0,3)
|
|
Diabetes mellitus
|
E10–14
|
T89, T90
|
3 615 (0.3)
|
|
Impaired immunity
(cancer, transplanted organs or congenital immunodeficiency)
|
C00–97
Z94
D80–84
|
B73, B74 B99
|
2 561 (0.2)
|
Data on hospitalisations are based on completed stays in hospital reported to NPR. Hospitals report these monthly, and the linkage is based on data reported for the period 1 January 2020–30 April 2020.
We defined hospitalisation for COVID-19 as testing positive to SARS-CoV-2 in MSIS and hospitalisation with the diagnostic code U07.1 (“COVID-19, virus identified”), B34.2 (“Coronavirus, unspecified”) or B97.2 (“Coronavirus as cause of diseases classified to other chapters”).
Statistical analyses
We calculated the percentages with confirmed SARS-CoV-2 by sex and age group for the whole period. For the total under-20 age group, we calculated the incidence of hospitalisations for COVID-19 (per 100 000) and the percentage of all hospitalisations for COVID-19 that were in this age group.
We conducted descriptive analyses of groups with confirmed SARS-CoV-2 with and without underlying conditions. Because the incidence of both underlying disease and SARS-CoV-2 increases with age, we show the results for those infected as estimates adjusted for age, presented as percentages compared with the percentage with confirmed infection in the under-20s population. For age adjustment, the R function “ageadjust.indirect” from the R package “epitools” was used with the population in the one-year age groups as reference populations. This also calculates the confidence interval (16).
Ethical considerations
The Norwegian register regulations constitute the legal basis for compiling of statistics. At no point in the process did Directorate of Health staff have access to national identity numbers or other directly identifying data, and Institute of Public Health staff only had access to statistics.
Results
In the period 1 March to 13 May 2020, 8 125 persons in the whole population of Norway tested positive for SARS-CoV-2. This included adults and elderly people, and 493 (6.1 %) were under the age of 20 years. Of these, 115 (1.4 %) were under 10 years old, and 378 (4.7 %) 10–19 years old (Table 2 and Figure 1). The median age of the under-20s group that tested positive was 15 years, and 252 (51.1 %) were girls.
Table 2
Population and number of individuals with confirmed SARS-CoV-2 registered in the Norwegian Surveillance System for Communicable Diseases (MSIS) in the period 1.3.2020–13.5.2020 (n = 493) aged 0–19 years, by age group and sex.
|
|
0–4 years
|
5–9 years
|
10–14 years
|
15–19 years
|
|
Population
|
290 063
|
315 295
|
324 769
|
318 622
|
|
Boys
|
29
|
26
|
67
|
119
|
|
Girls
|
28
|
32
|
58
|
134
|
|
Total
|
57
|
58
|
125
|
253
|
|
Incidence per 100 000
|
19.7
|
18.4
|
38.5
|
79.4
|
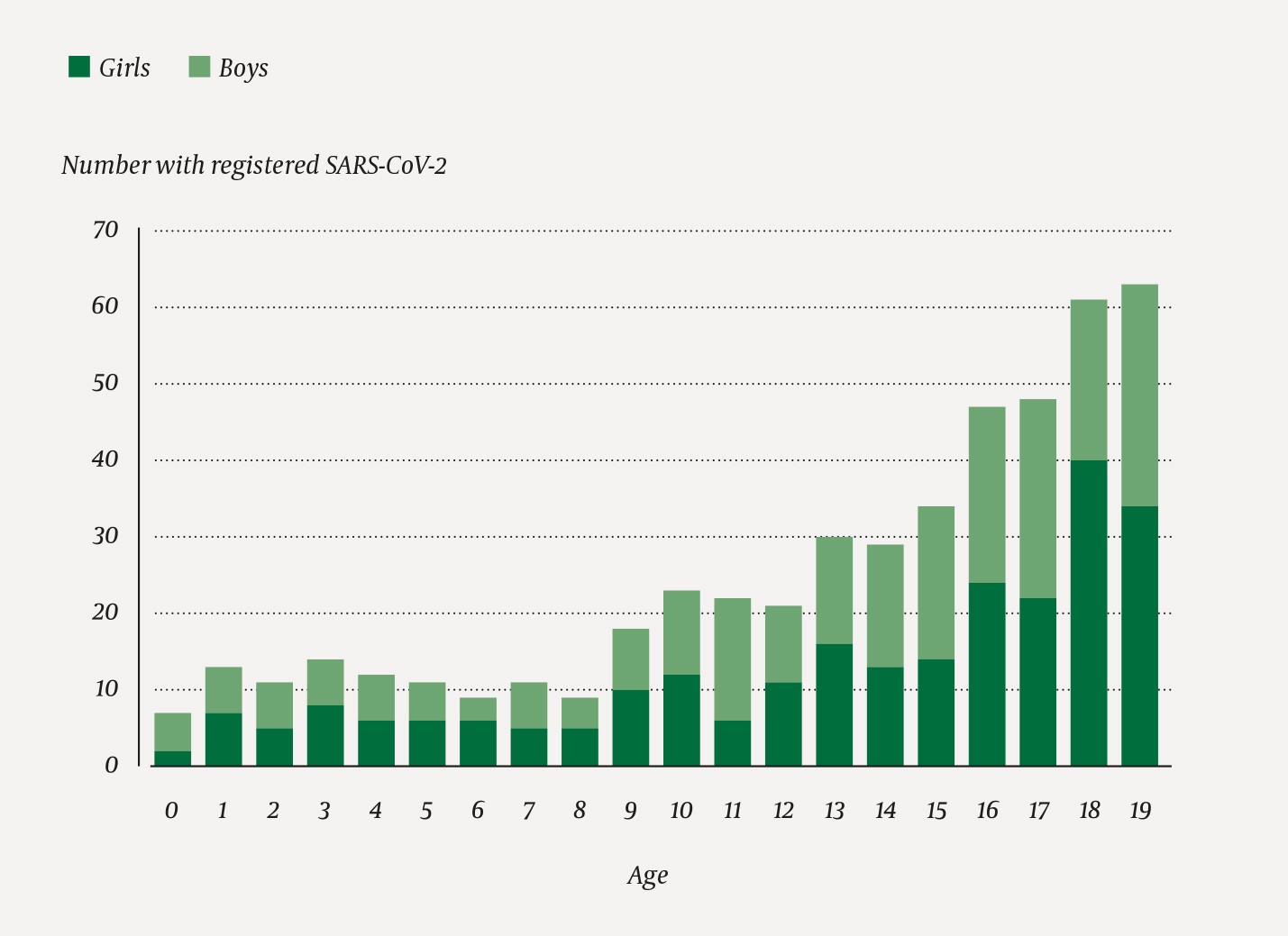
Figure 1 Confirmed SARS-CoV-2 in children and adolescents aged under 20 years registered in the Norwegian Surveillance System for Communicable Diseases (MSIS) in the period 1.3.2020–13.5.2020 (n = 493) by age and sex.
Up to and including April 2020, 14 individuals younger than 20 years (six girls) were discharged from hospital in Norway with confirmed SARS-CoV-2. This amounts to 3 % of all children and adolescents with confirmed infection up to and including April (n = 462). The incidence of hospitalisations for SARS-CoV-2 in the age group was 1.1 per 100 000 in the period in question. Of the in all 1 093 hospitalised with SARS-CoV-2, children and adolescents aged under 20 years accounted for 1.3 %. No deaths in the under-20s age group were registered in Norway.
The under-20s population consisted of 1 248 749 persons. Of these, 67 657 (5.4 %) had an underlying condition (Table 1). A total of 41 of 493 individuals (8.3 %) with confirmed SARS-CoV-2 and aged under 20 were registered as having one or more underlying conditions. The incidence of confirmed SARS-CoV-2 in this group was 61 per 100 000, compared with 39 per 100 000 of the total under-20s population.
Figure 2 shows the incidence of confirmed SARS-CoV-2 in the whole under-20s population compared with the incidence among individuals with underlying conditions. Children and adolescents with muscular and nervous system diseases were over-represented in the group with confirmed infection. Children with asthma, diabetes, chromosomal abnormalities, chronic cardiac disease, chronic pulmonary disease, rheumatoid disease or inflammatory bowel disease did not stand out through an increased incidence of infection. No-one in the group with impaired immunity (cancer, transplanted organs or primary immune deficiency) had confirmed SARS-CoV-2.
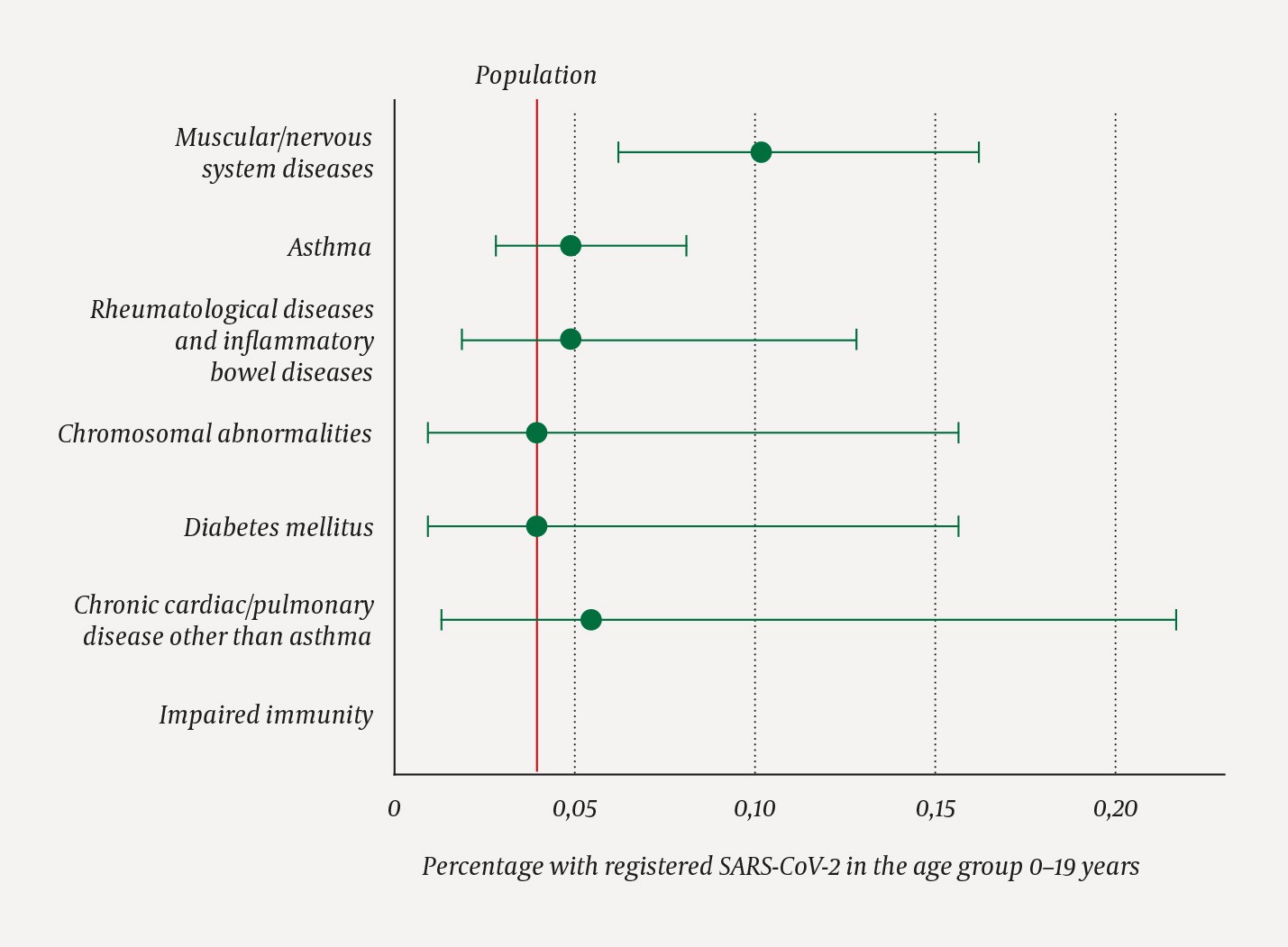
Figure 2 Percentage with registered SARS-CoV-2 in the population aged under 20 (red vertical line, n = 493 of 1 248 749) and among individuals aged under 20 with underlying conditions (n = 41, age-adjusted with 95 % confidence interval) in the period 1.3.2020–13.5.2020. No-one in the group with impaired immunity had confirmed SARS-CoV-2.
Of the 14 who were treated in hospital, three had an underlying condition.
Discussion
There were few children and adolescents with confirmed infection in Norway in the first phase of the pandemic, and very few were hospitalised. Diagnostic groups where there is an indicated increased risk of COVID-19 in adults, for example patients with diabetes and cardiac/pulmonary diseases (17), were not over-represented among individuals under the age of 20 with confirmed infection. A generally low number of children and adolescents with underlying conditions tested positive for the virus.
Other studies have also found that children and adolescents constitute a small proportion of all cases of confirmed SARS-CoV-2. In a European register, the European Surveillance System (TESSy), with over 576 000 registered infection cases, 1.3 % are under the age of 10 years (11), which is comparable with 1.4 % in our data. In the Madrid region and in the USA, 0.8 % and 1.7 %, respectively, of those with confirmed infection were under 18 years old (1, 9), and in China 2.2 % were less than 20 years old (10). We found a somewhat larger share of 6.1 % under 20 years old, which may be due to greater testing capacity and activity in Norway. In Iceland, 3 % of all positive tests were in children aged under 10 years. This may also be due to higher testing activity and a lower threshold for testing (3). However, none of the in all 848 under 10-year olds in the Icelandic study of a random sample tested positive, compared to 0.8 % of adults. In the area in Italy that was first affected, 2.6 % tested positive for SARS-CoV-2 in a population screening, but none of them were children under 10 years old. The percentage of positive tests increased particularly for over-50s (4).
We found no notable gender difference for those with confirmed infection, and equal distribution between the sexes also applies to Norway’s population as a whole (18). Icelandic data show a higher risk for men, both through population screening and in targeted testing according to symptoms and risk (3), and studies from China and the US also find a non-significant excess of boys (1, 19). There is a somewhat larger percentage of men than women among hospitalised adults in Norway (18), and other countries also have an excess of adult men among hospital patients (17, 20). The figures for children and adolescents hospitalised in Norway are too low for any conclusions to be drawn.
The proportion of under-20s among patients hospitalised with SARS-CoV-2 was 1.3 % in our dataset. In other places there is a similarly small share of approximately 1 % (1.3 % in New York, 0.9 % under the age of 15 in China) (17, 20).
Reports from the US indicate that about 6 % of children and adolescents with confirmed SARS-CoV-2 were hospitalised (1). The corresponding figures from Italy are 11 % (21) and from Spain a full 60 % (9). A smaller percentage of children and adolescents are hospitalised in Norway, which may be due to greater testing activity and to more youngsters being tested because of mild symptoms or contact tracing. To prevent the spread of infection, some countries have practised hospitalisation instead of isolation at home of confirmed infected persons, and this will also result in a far larger percentage of SARS-CoV-2 patients in hospital (10). The percentage of infected persons who were hospitalised in Norway is far lower among children and adolescents than in the over-20s population (18).
Our study has several strengths, not least that the compilation of data from national registers makes it possible to analyse the whole population. We have looked at large groups with underlying conditions identified through diagnostic codes from both the primary and the specialist health service, and have thus included data from groups of diseases that pose a potentially higher risk of an infectious disease taking a serious course. With such a low number of infected cases, it is not possible to study groups of less common underlying diseases. Our estimates even for combined groups of less common underlying diseases are equivocal. Mild cases of the disease, where health services have not been contacted or no final diagnosis has been made, will also be absent from data sources. Registered data on underlying conditions for the youngest age groups may be incomplete.
A weakness of the study is that testing capacity was limited during the first weeks of the pandemic, and groups such as health workers, potential hospital patients and close contacts of infected persons received priority. This may have led to somewhat fewer children and adolescents with SARS-CoV-2 being tested, compared with adults. We therefore cannot draw conclusions on the incidence of infection, and wait for serological studies to provide greater clarification. Data from Iceland, where large-scale testing was conducted both as screening of a random sample and on the basis of symptoms and risk, indicate a real lower incidence of infection among children under 10 years old (3). A study based on transmission in Wuhan and Shanghai estimates that the risk of being infected with SARS-CoV-2 is three times as high for adults as for children and adolescents (7).
There has probably been a lower threshold for testing children and adolescents with chronic diseases and higher susceptibility to infection. Healthy children with mild symptoms are probably tested to a lesser extent. Testing practice may therefore create a false association (confounding by indication). The association between increased infection incidence and neuromuscular disease must therefore be interpreted very cautiously, also because the number infected in groups with rare diagnoses such as cerebral palsy and muscular diseases is very low. We found that the other diagnosis groups were not over-represented among infected under-20s. However, the figures are small, and any differences may therefore be difficult to demonstrate (type 2 error). We do not have a sufficiently large dataset to study the association between risk of hospitalisation and underlying disease. Studies in the US have found that eight of ten hospitalised children and adolescents in ICUs have an underlying condition (22), and that especially children with chronic complex disorders were over-represented.
Our data show that the incidence of confirmed SARS-CoV-2 is low among children and adolescents, and that very few of those with confirmed infection require hospitalisation. Groups with underlying conditions such as cardiac and pulmonary disease, diabetes or impaired immunity were not over-represented among infected under-20s in Norway in the initial period of the outbreak of the coronavirus.
