In 1992, the National Insurance Agency determined that primary care doctors should use ICPC (International Classification of Primary Care) for coding of diagnoses on reimbursement cards and sickness certifications. The purpose was to establish a consistent system for coding of diagnoses. Norway was thereby the first country to apply ICPC as an official national standard. Since 2004, the follow-up version ICPC-2 has been used (1).
ICPC is based on a letter code for the organ system, including separate letter codes for general conditions, mental disorders and social problems, followed by a two-digit code for a more specific categorisation. The numeric codes 00–29 denote symptoms and ailments, while 70–99 denote diagnoses and diseases For example, the diagnostic code for pneumonia consists of the letter R for respiratory disorders and the numeric code 81.
The first case of COVID-19 infection in Norway was detected on 26 February 2020. It is assumed that many cases go undetected, since many of those infected have minor symptoms and will never be tested. To obtain a better overview of the pandemic one will therefore also use diagnostic data from the primary care doctors’ electronic patient records, including those from out-of-hours services (2). In connection with the COVID-19 pandemic new diagnostic codes have been introduced: R991 (suspected or probable COVID-19 infection) and R992 (confirmed COVID-19 infection) (2).
For a number of years, the National Centre for Emergency Primary Health Care has prepared statistics based on reimbursement cards from out-of-hours services (3). We have gradually become concerned by an increasing use of non-specific diagnoses, especially for telephone contacts. In 2018, altogether 65.5 % of all telephone contacts were given one of three such diagnostic codes: A29 (General symptom/complaint, other), A97 (No disease) or A99 (General disease/non-specific) (3). Such use of non-specific diagnoses erodes the basis for using these data for disease surveillance. The objective of this study was to analyse the trend in the use of diagnostic codes for respiratory infections and non-specific diagnoses in the period 2008–2019.
Material and method
The material consists of data from all electronic reimbursement cards submitted by doctors on out-of-hours duty in the period 2008–2019, previously used in preparation of the Annual statistics from out-of-hours emergency health care (3). Anonymised data files were provided by the Norwegian Health Economics Administration (Helfo)/the register for control and payment of reimbursements for health care (KUHR). We have no information that can identify the municipality or out-of-hours service in question, nor the form of payment, but each therapist has been assigned a unique number that enables aggregation of fee codes per doctor.
An increasing number of out-of-hours facilities have a fixed salary scheme for their on-duty doctors, and this has previously meant that many reimbursement cards were sent with the out-of-hours facility’s or the municipality’s organisation number, with no information about the treating physician. Since 2016, however, all billing must include information to identify the therapist who provided the treatment. Nurses in local emergency medical communications centres often provide advice to patients, but cannot complete a reimbursement card in their own name. These telephone contacts must therefore be linked to an identifiable doctor. How and to what extent this is done in practice is likely to vary from one out-of-hours facility to the next.
Consultations and home visits (fee codes 2ad, 2ae, 2ak, 2fk, 11ad or 11ak, hereafter referred to as consultations) and telephone contacts (fee codes 1bd, 1bk, 1be and 1 g) were registered. The sum total of all out-of-hours contacts was defined as the sum of consultations and telephone contacts. Contacts that were coded with diagnostic codes for respiratory infections (R71–R83) or three general, non-specific diagnoses (A29, A97 and A99) were included. For each year, we estimated the proportions that these diagnostic groups accounted for in the total number of consultations or telephone contacts.
The Annual statistics from out-of-hours emergency primary health care were assessed by the data protection officer of the Norwegian Labour and Welfare Administration (NAV) and the data protection officer for research (3). Since no individuals can be identified in the material, either directly or indirectly, the project is not subject to notification pursuant to the Personal Data Act.
Since the material includes all electronic reimbursement cards and does not constitute a sample, the differences identified are genuine and not fraught with statistical uncertainty. The data are therefore presented without confidence intervals, and no statistical tests have been undertaken.
Results
The number of consultations per year increased from 1 402 452 in 2008 to 1 417 395 in 2019, a relative increase of 1 %. The number of telephone contacts per year increased from 286 515 in 2008 to 684 773 in 2019, a relative increase of 139 %. The total number of contacts with out-of-hours services involving respiratory infections fell by 26 % from 240 037 to 176 909, while out-of-hours contacts registered with non-specific diagnoses increased nearly thirteenfold, from 40 280 to 514 715. The proportion of respiratory infections and non-specific diagnoses in all telephone contacts is shown in Figure 1, and the equivalent proportion of all consultations is shown in Figure 2. In absolute numbers, the use of non-specific diagnoses for telephone contacts increased by a factor of 19, from 24 802 to 473 257. For consultations, it increased by a factor of 2.7, from 15 478 to 41 458.
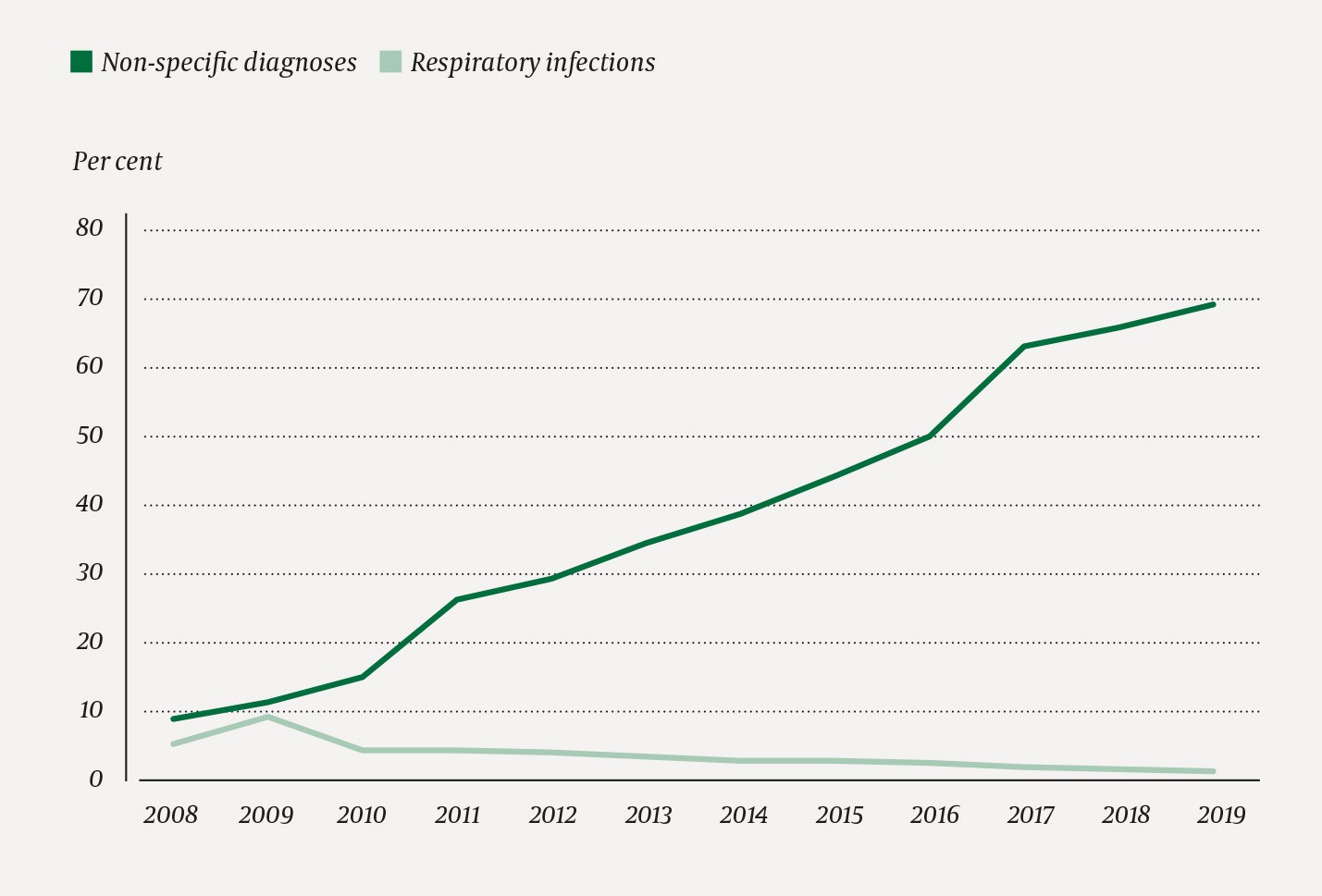
Figure 1 Proportion (per cent) of all telephone contacts that were given a diagnostic code for respiratory infection or one of three non-specific diagnoses (A29, A97, A99).
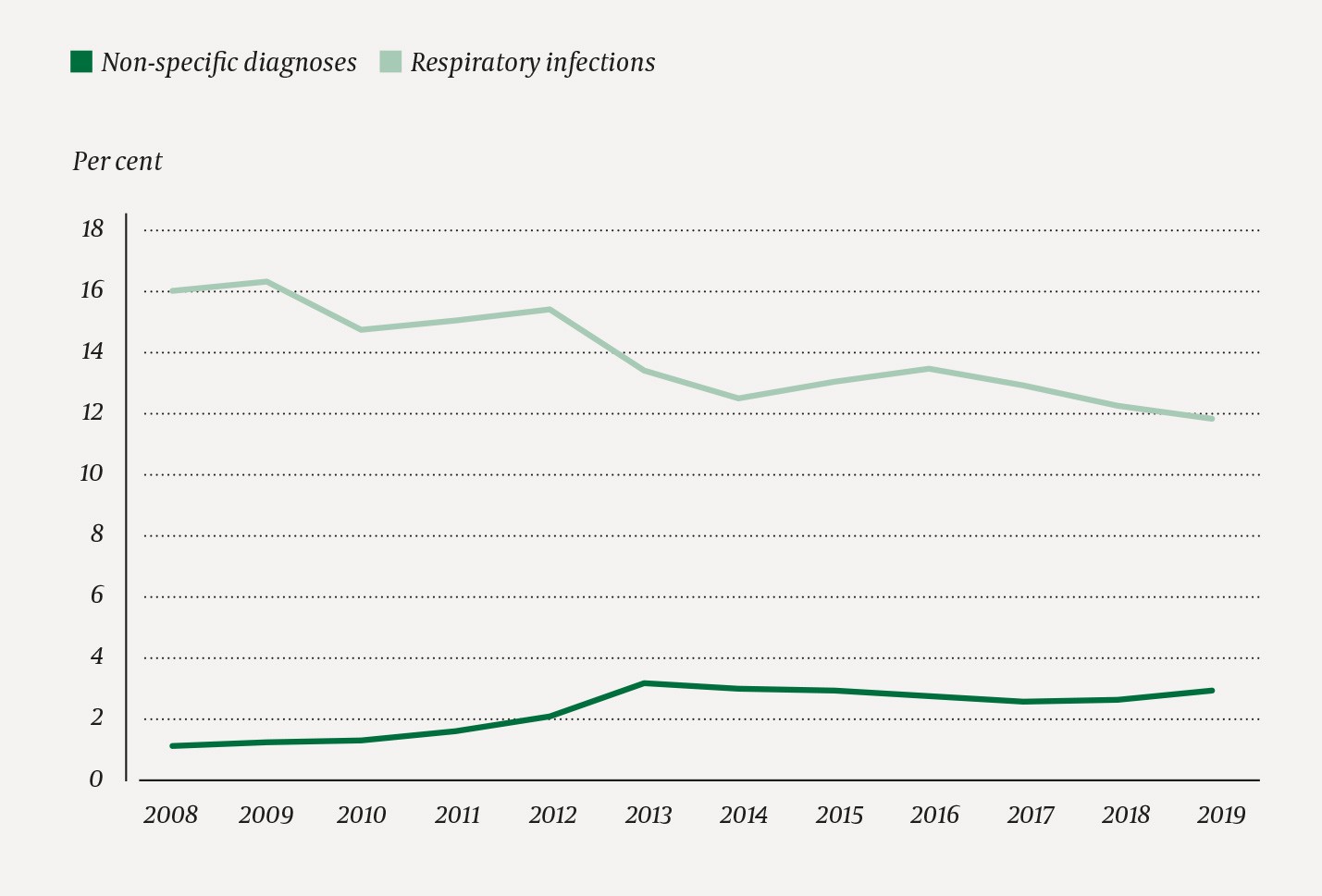
Figure 2 Proportion (per cent) of all consultations that were given a diagnostic code for respiratory infection or one of three non-specific diagnoses (A29, A97, A99).
In 2019, fourteen doctors were responsible for 45 % of all reimbursement cards for telephone consultations, and of these, 99 % were coded with a non-specific diagnostic code.
Discussion
This study shows that the number of consultations in out-of-hours services remains stable, while there is a strong growth in the number of telephone contacts. Moreover, there is a marked increase in the use of non-specific diagnostic codes, primarily for telephone contacts. In parallel with this trend, fewer out-of-hours contacts are registered as respiratory infections.
Previously, telephone contacts with nurses in the local emergency medical communications centres have most likely been underreported, in the sense that telephone contacts have not been billed. Reimbursement cards for such contacts are now likely to be prepared more often. The high number of telephone contacts for a handful of doctors may indicate that some out-of-hours facilities use patient records systems with functions that produce standardised reimbursement cards in the name of a permanent doctor and with an unspecified diagnosis. The Watchtower project, which registers actual telephone contacts in seven selected out-of-hours facilities, finds relatively stable rates of telephone contacts (4).
Diagnostic codes for consultations are entered by doctors. These show less variation over time, but even here we can see a tendency towards increasing use of non-specific codes, at the cost of other and more specific diagnoses. A previous study found reasonably good validity for general practitioners’ use of ICPC diagnoses in consultations, but the authors cautioned against including simple contacts in the underlying data for public statistics (5).
Should the current coding practices continue, the frequency of respiratory infections will be underestimated. This is a matter of concern in the present situation, where the health authorities will monitor the COVID-19 pandemic with the aid of such diagnoses collected from GPs and out-of-hours services.
The volume of non-specific diagnoses is already so large as to undermine the basis for statistics and research based on reported ICPC diagnoses. For medical consultations, the volume is still limited and the possibilities for misinterpretation relatively minor. For telephone contacts, however, the level is so high that the diagnostic system in practice has lost its value when it comes to showing the distribution of diagnoses for telephone contacts with out-of-hours services. This is serious, not only in the context of the current pandemic, but for the validity of all epidemiological research based on such registry data. The Directorate of Health ought to consider impressing on both GPs and out-of-hours facilities that they should strive to use correct diagnostic codes, avoid non-specific diagnostic codes in particular and refrain from automatic generation of diagnostic codes on reimbursement cards.
