A child of early school age was hospitalised after several days of illness with abdominal pain, vomiting and a palpable mass in the upper abdomen. Further diagnostic workup revealed a very unusual cause.
The child had been vomiting and experiencing abdominal pain for four days. The referring doctor had palpated a large mass in the upper abdomen. Last defecation was at least two days previously. The child was under paediatric psychiatric follow-up because of trichotillomania and trichotillophagia.
On examination the patient’s general condition was good, but there was a hard mass about 20 cm in diameter from the epigastrium down to below the level of the umbilicus. Blood tests revealed haemoglobin 10.5 g/dl (reference range 11.0–15.5) and alanine amino transferase (ALT) 49 U/L (10–45). Other liver and bile tests and CRP and leukocyte levels were normal.
An ultrasound scan of the abdomen revealed a mass located in the stomach. It was also visible on an X-ray scan of the abdomen. A supplementary X-ray scan with contrast revealed a mass that occupied the whole stomach, consistent with a ‘very large bezoar’ (Figure 1). In light of information about earlier trichotillophagia, it was assumed to be a trichobezoar.
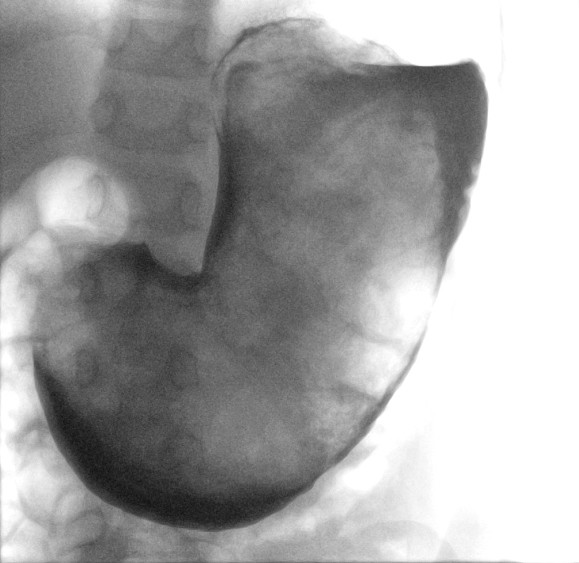
Figure 1 The X-ray image shows a mass (surrounded by contrast) in the stomach.
This was confirmed by laparotomy the same day. A trichobezoar was removed that filled the entire stomach, with an extension about 60 cm long that was withdrawn backwards from the small intestine (Figure 2). The trichobezoar weighed more than 750 g. The post-operative course was uncomplicated, and the patient was discharged on the fifth post-operative day, with an appointment for further paediatric psychiatric follow-up.

Figure 2 The trichobezoar shaped like the stomach, with an extension about 60 cm long
Discussion
A bezoar is an accumulation of indigestible material in the gastrointestinal tract, usually located in the stomach (1–4). If it consists of hair, it is called a trichobezoar (1, 2). In order for a trichobezoar to form, the patient must have been pulling out substantial amounts of hair for a long time (trichotillomania) and then swallowing it (trichotillophagia). If stomach peristalsis does not push the hair on into the small intestine, a large collection of hair will gradually form in the stomach. It is estimated that about 1 % of persons with severe trichotillomania will experience bezoar formation that requires surgical intervention (1, 5).
In a clinical review article on trichotillomania published in the Journal of the Norwegian Medical Association in 2018, this is described as a mental disorder that typically strikes during adolescence and has a chronic course. Medication has a more limited effect than behavioural therapy on this disorder. Most patients respond to behavioural therapy, with about half achieving remission (6). The article estimates a lifetime prevalence of 0.6–2.4 % and that 5–18 % of hair-pluckers swallow the hair (6).
Trichobezoars can attain a considerable size before causing symptoms as described in this case history, where the whole stomach was full of the bezoar (Figure 1). Further preoperative examinations were not necessary. CT scans with contrast are reported to be capable of diagnosing 97 % of stomach bezoars (7), but represent significant radiation exposure, which it was possible to avoid with this child.
As shown in Figure 2, the main portion of the bezoar was more than 20 cm long, and the maximum diameter about 10 cm. It retained the shape of the stomach after removal. This was because it was very compact, and would not have lent itself to endoscopic removal, which often proves unsuccessful (2). Laparotomy with gastrotomy is recommended for removing large trichobezoars from the stomach (2).
The trichobezoar had a 60 cm tail (Figure 2). It was palpable a good way down into the jejunum, and could be removed through the gastric outlet by cautious traction. If this had not been feasible, the tail would have had to be removed through a separate incision in the small intestine to prevent it becoming lodged and causing an intestinal obstruction (2). A tail of this kind occurs in a minority of cases (4, 8), but because of its characteristic appearance has acquired a special name in medical literature: Rapunzel syndrome (2, 4, 6). The name refers to the long hair of Rapunzel, who was imprisoned in the tower, known from the Brothers Grimm’s fairy tales from 1812.
Although a trichobezoar is a rare condition, it must be considered for patients with trichotillophagia and abdominal symptoms. Symptomatic trichobezoars are often so large that they are palpable on simple clinical examination, as in the present case. Such a finding must lead to further diagnostics in hospital.