In 1912, an epilepsy colony was established in Bærum, inspired by similar colonies in other countries. Its first years were marked by financial constraints and limited treatment options.
In the basement of the National Centre for Epilepsy in Bærum we recently came across a number of historical documents. These give an insight into the first years of what can be referred to as organised epilepsy care in Norway, and include patient protocols for the period 1913–20, five copybooks for the period 1905–23 and a ledger for the period 1905–20 (Figure 1).
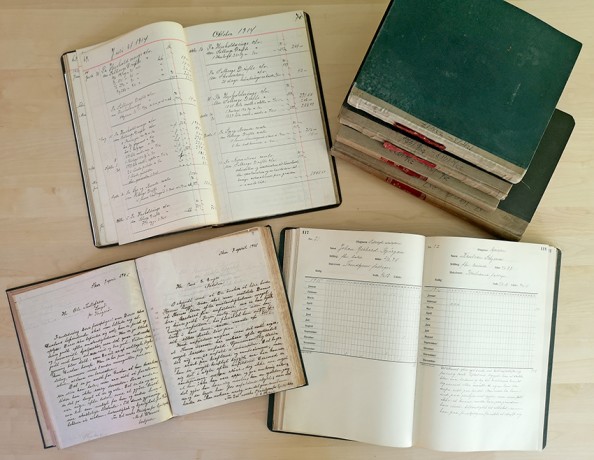
Figure 1 Books found in the basement of the National Centre for Epilepsy that have given an insight into life at the institution during its first years of existence (1913–20). Photo: Oliver Henning
Prior to 1920, patients did not have individual records such as we know them today. The copybooks and the ledger mainly provide information about the daily running of the colony, while the patient protocols and the seizure calendars give some clinical information about the patients who were admitted at the time.
Establishment of epilepsy colonies
In the early 19th century, many countries established asylums for people who could not take care of themselves, mainly those with mental disorders, epilepsy or intellectual impairment (1). The idea was that society had to be protected from such persons. People with epilepsy who could not be accommodated by an asylum usually had major problems with coping in society. Children with epilepsy were excluded from the regular schools, and adults had problems finding paid work. In the cities, many of them lived in poorhouses, and in rural areas, many were sent to farms where they were provided for. This system of poor relief was an obligation placed on farmers by the social welfare authorities, and everybody was required to participate. Those who were sent ‘on the parish’ tended to stay at the same farm for one year at a time.
The intention was to create small independent communities for people with epilepsy away from society at large
In the latter half of the 19th century some European countries, including Germany and England, established epilepsy colonies (1, 2). The intention was to create small independent communities for people with epilepsy away from society at large. As a rule, the colonies were located in isolated spots in the countryside, and most of them were established on the initiative of philanthropists associated with a Christian humanist movement that had its origins in Germany.
The pioneer Ludvig Waale
Inspired by a visit to the Bethel epilepsy colony in Bielefeld, Germany, deacon Ludvig Waale (1861–1932) established a small epilepsy institution in Kristiania (now Oslo) in 1895. At first it was located at Lindern before moving to Skar in the Maridalen valley and later to Sandaker (3). Waale’s pioneering effort met with a lot of resistance. It was a common notion that people with such a frightening disease as epilepsy belonged in the asylums.
In the early 20th century, Hartvig Halvorsen (1854–1910), an elder on the board of Diakonhjemmet Hospital, argued that the deacons should include epilepsy care in their programme. In 1904, an agreement was therefore made with Waale to the effect that his care home should come under the jurisdiction of Diakonhjemmet Hospital. From 1 January 1905, the care home became known as the Norwegian Nursing Home for Epileptics, and deacon Mikal Antonius Wærnes (1865 – year of death unknown) was appointed director. Patients of all ages, including children as young as 5–6 years, were admitted. From the ledger we can see that in 1907, public authorities paid NOK 420–445 per patient per year, while private individuals were charged NOK 480–600.
Solberg farm becomes an epilepsy colony
Partly because the nursing home had too few places to cover the need, and partly because of complaints from neighbours, the Association of Deacons chose to purchase Solberg farm, which was centrally located in Bærum, and move the nursing home there in 1912 (Figure 2). The farm owned 50 hectares of cultivated land and cost NOK 63 000. The institution was patterned on epilepsy colonies in other European countries, and started its activities in the spring of 1913.

Figure 2 Solberg farm. The farmhouse has been demolished and replaced by a laboratory building. This picture was taken around 1965. Photographer unknown, property of the Norwegian Centre for Epilepsy.
Patients from all over the country were referred to Solberg farm. Approximately 80 % of the admissions were funded by public authorities, mainly by local poor relief agencies. The remaining 20 % were paid for by the patients’ relatives. Sometimes the willingness to pay was low, and perhaps also the ability. The following is written about one patient who was admitted from February 1913 until August 1914: ‘His father wanted to take him home. Unable to pay for him in this time of high costs.’ About another patient who was admitted for six months in 1914, it says: ‘Moved back home to his mother, since Larvik poor relief fund no longer wanted to pay for him.’
Financial constraints were a major problem during the first years. Professor Christopher Blom Leegaard (1851–1921) at the National Hospital, who was the first medical supervisor, was paid an annual salary of NOK 500. When Peter Christen Barth (1872–1942) took over in 1920, the annual salary was raised to NOK 600.
According to Wærnes’ estimates of dietary costs in 1909, the payment per patient per day was NOK 1.21, while the costs amounted to NOK 1.45, i.e. a difference of NOK 0.24. By 1919, this difference had increased to NOK 2.16. There were also other worries: ‘… for next winter we will need to purchase firewood. The forest has been so drastically thinned that no more of it can be felled …’
Elsewhere, Wærnes writes: ‘We all surely agree that good care of the sick should not only be endeavoured, but also realised, but this is where finances often intervene to the patients’ detriment. Compassion on the part of the staff may smooth out the deficiencies, this is true, but …’
The number of patients varied from 50 in 1905 to 82 in 1917, while the number of annual hospitalisation days varied from around 13 000 in 1908 to around 23 000 in 1917.
Frequent seizures and high mortality
In the epilepsy colony, a seizure calendar was kept for all admitted patients (Figure 3). According to our estimates, an average of 0.45 seizures were recorded per patient per day in the years 1908–19. Some had very frequent seizures; for example, 2 526 seizures were recorded in one male patient in August 1915. The seizures were not sub-classified, as we do today, but we can assume that most of the seizures registered in the calendars were of the tonic-clonic type.

Figure 3 Seizure calendar for a patient who was admitted in 1913. Photo: Oliver Henning
In the period 1912–19, an average of 8.5 deaths occurred in the colony annually (4–24 deaths). No antiseizure treatment was available at the time, and many died in status epilepticus (Figure 4). The especially high death toll in 1918 is mainly attributable to the Spanish flu.
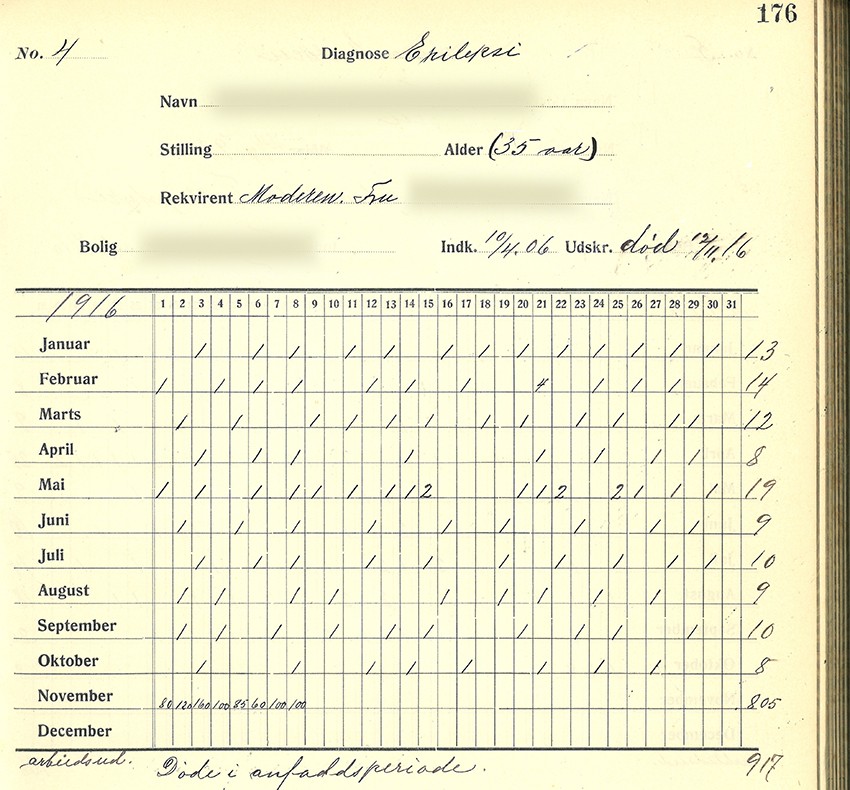
Figure 4 Seizure calendar for a patient who died in status epilepticus in 1916. Photo: Oliver Henning
In a letter to next of kin who had lost their son, Wærnes writes: ‘My opinion is that this outcome was the best for him. A longer life in this state of mental confusion and distress would only have caused him and his family greater pain than this relatively calm end to a life of hard struggle against an incurable and highly degenerative disease.’
What treatment did the patients receive?
The patients were treated with bromides, mainly potassium bromide (Borate). Bromides had a certain anticonvulsive effect, but occasionally we get the impression that the adverse effects were worse than the epilepsy itself. The adverse effects, referred to as bromism, came in the form of fatigue, mental slowness, apathy, impaired vision, nausea, drooling, trembling and severe acne, pustules or ulcers, especially on the face and neck (4). Bromide-induced facial acne was referred to as facies epileptica. Psychiatric effects in the form of irritability, uninhibited and unrestrained behaviour, depression, hallucinations and sometimes schizophrenia-like psychoses were also not uncommon. Many of the patients are consequently described as deeply sedated. About a woman who was admitted in 1917, it is said: ‘Upon admission, the patient had large ulcers on her arms and legs … skin eruptions reportedly caused by potassium bromide, which has been used for a long period.’
The anticonvulsant effect of phenobarbital was discovered by the German doctor Alfred Hauptmann in 1912 (5), but this drug was not used clinically in Norway until after 1920.
Epilepsy plus
In addition to severe epilepsy, most of the patients also had problems of a cognitive, psychiatric and/or behavioural nature, or what we refer to as epilepsy plus (6). It has been difficult for us to determine whether the patients’ behavioural disorders were linked to the cause of epilepsy, non-recognised focal epileptic seizures, post-ictal psychoses, adverse effects of the treatment, comorbidity or other causes. In a letter dated 6 April 1910, addressed to the governor of Kristians county, Wærnes notes: ‘… ‘the patient had 362 seizures in 1909, potassium bromide was used throughout the year. The patient’s sensory capacities are considerably dulled. Periodically, mental disturbances occur, whereby the patient becomes very agitated, occasionally violent, so that he needs to be isolated.’ Transitory psychosis-like conditions are described in many patients; we interpret these as likely post-ictal psychoses. In 1906, it is said about a patient: ‘On the Saturday before Christmas he went totally out of his mind, he first refused to eat, and then had hallucinations. He had to be confined to bed … For the last two days he has been much better, so he eats and can respond when addressed, and he has asked for his father.’
Because of a precarious economic situation, Wærnes suggests three possible solutions for the colony in 1919
About another patient who was admitted for four months in 1915, it is said: ‘Discharged because of agitation and violent behaviour which occurred nearly constantly. In the last period the patient had to be restrained, because he inflicted harm on himself.’
The state takes over in 1920
Because of a precarious economic situation, Wærnes suggests three possible solutions for the colony in 1919: ‘an increase in the nursing contributions’, ‘transfer of the entire institution to the state’ and ‘temporary closure of the nursing home, the farm’s activities continue’.
An application for a price increase in the nursing contributions was sent to the health authorities, but the application was rejected. In 1920, the deacons saw no other solution than to transfer the entire colony to the state free of charge. The precondition was that the property should be used ‘for the benefit of epileptics’. The first move by the state owners was to increase the daily rates.
Over the subsequent 100 years, the colony was extensively modernised. Today, the institution located at the former Solberg farm (Figure 5) is known as the Norwegian Centre for Epilepsy and is within Oslo University Hospital’s jurisdiction. The centre is Norway’s only hospital for patients with severe, uncontrolled epilepsy. With its history, it is a monument to the rapid development in epilepsy care that has taken place during the last century.

Figure 5 The epilepsy centre at Solberg farm in Bærum in the 1960s. Photographer unknown, property of the Norwegian Centre for Epilepsy.