A man in his sixties was hospitalised with vision loss due to second-stage syphilis. Ocular syphilis is a rare and serious condition. The incidence of syphilis is increasing, and since delayed diagnosis can result in permanent visual impairment, syphilis should be considered as a possible cause in patients with vision loss.
The patient contacted A&E because he had experienced relatively acute, painless loss of vision in his right eye four days previously. He described it as pronounced, darkened and blurry vision. An examination by an ophthalmologist revealed substantially reduced visual acuity in the right eye. The patient managed to count fingers at 2 metres. Visual acuity in the left eye was 1.2, so completely normal. Swinging flashlight test revealed a relative afferent pupillary defect in the right eye, i.e. that the pupils constricted less when the right eye was directly illuminated than when the left eye was directly illuminated. This suggested optic nerve damage or a large retinal injury of the right eye.
Field of vision testing revealed central scotoma of the right eye. The ophthalmologic exam was otherwise normal. No signs were found of uveitis or vasculitis. The retina and macula were normal in appearance. The optic nerve head was well defined with a physiological excavation (cup/disc ratio of 0.5). The ophthalmologist concluded that the vision loss was due to optic nerve involvement. As there was no pain, and the loss of vision was sudden, an ischaemic cause was suspected.
Temporal arteritis is an important differential diagnosis in cases of ischaemic involvement of the eye and acute vision loss in patients over the age of 50. Untreated temporal arteritis can cause irreversible blindness, and in rare cases stroke (1). The patient’s history was scrutinised with the possibility of temporal arteritis in mind.
The patient related that he had an ‘infection in his body’ that the doctors could not identify. He had felt seriously ill for about four and a half months. He had no energy, experienced hot flashes, diarrhoea, headache, pain in the abdomen and large muscle groups, and in the gums and throat. He himself was sure it was caused by vitamin deficiency following gastric bypass surgery he had had earlier. His family doctor had therefore referred him to the Centre for Obesity. A rheumatologist and an endocrinologist had previously examined him without arriving at a diagnosis. However, enlarged lymph nodes were found in his neck and a rash had been present on his back. Blood tests showed an elevated sedimentation rate (SR) and C-reactive protein (CRP), but no definite cause was found.
When examined by the ophthalmologist he had a pink, scaly maculopapular rash over his entire back (Figure 1). A weaker pulse was palpated in the right temporal artery, and the right temple was tender to palpation. Blood tests showed anaemia with Hb 10.4 g/dL (reference range 11.1–14.9 g/dL) and elevated inflammatory parameters with CRP 23 mg/L (0–5 mg/L) and SR 50 (2–20 mm).
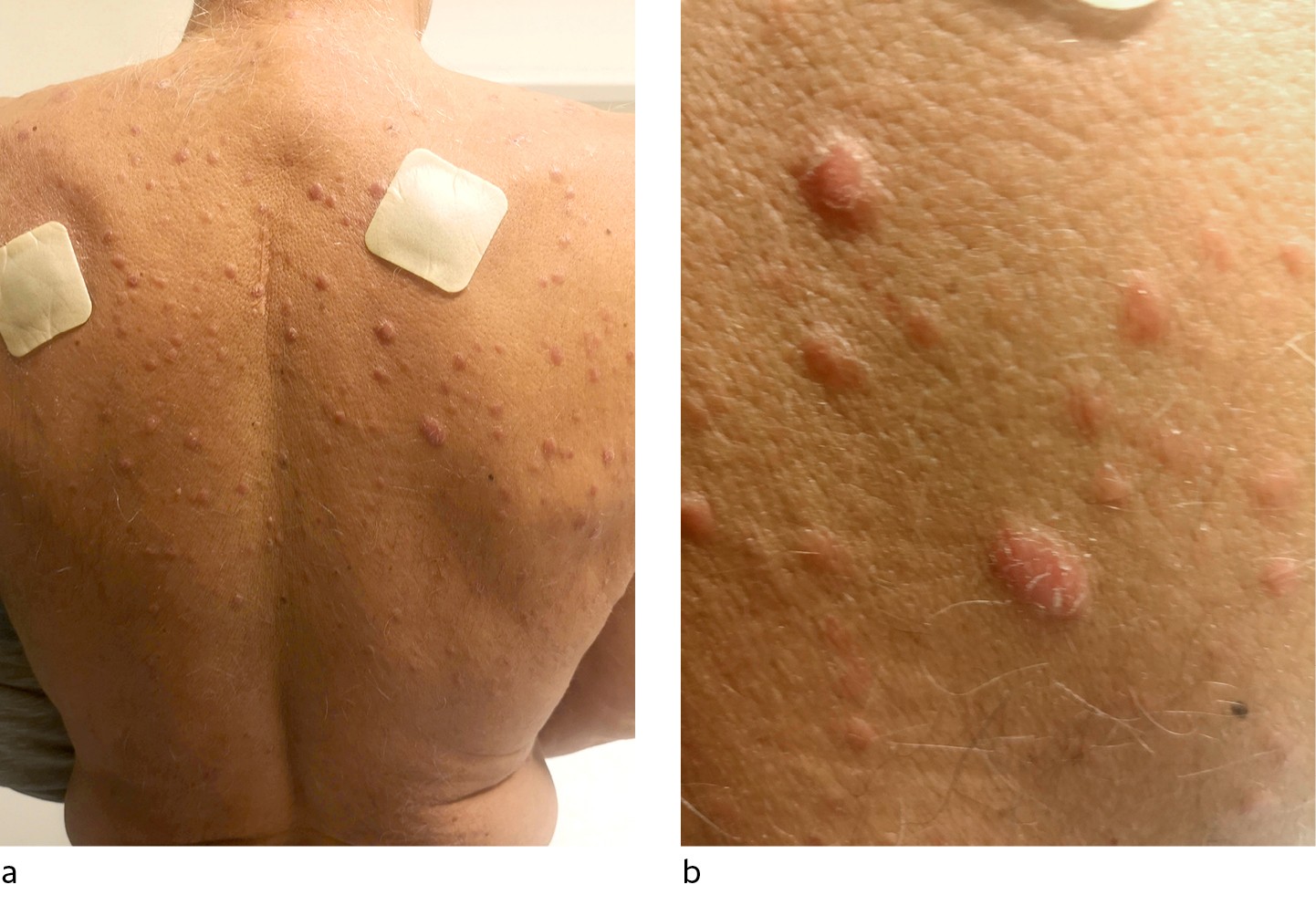
Figure 1 Multiple pink papules distributed over the back
Elevated SR and CRP, malaise, age, optic nerve involvement coupled with tenderness to palpation and weakened temporal artery pulse aroused suspicion of temporal arteritis. The patient was admitted to the Department of Ophthalmology, and started treatment with prednisolone 80 mg once a day and acetylsalicylic acid 75 mg once a day as prophylaxis against further ischaemic events. Temporal artery and dermal biopsies were performed. The following day the patient was transferred to the Department of Rheumatology, where steroid therapy was continued with intravenous methylprednisolone 1 g per day.
An expanded patient history revealed that he had been in Thailand five months previously and had had unprotected intercourse with multiple women. Two months later a non-tender, hard lesion had developed on his penis, and several weeks after that he developed a rash on chest and back. The penile lesion resolved after two weeks, but his general malaise and rash persisted.
Tests were conducted for chlamydia, gonorrhoea, HIV, hepatitis B and C, tuberculosis and syphilis, as well as for antinuclear antibodies (ANA) and antineutrophil cytoplasmic autoantibodies (ANCA). A CT angiogram was performed to evaluate for large-vessel vasculitis. The scan revealed a 55 mm dilated thoracic aortic aneurism, but there were no inflammatory changes in the large blood vessels suggestive of vasculitis.
Syphilis antibody tests, Treponema pallidum particle agglutination assay (TPPA) and rapid plasma reagin (RPR) tests were positive in very high titres. Temporal arteritis was deemed unlikely, and methylprednisolone was discontinued.
The patient was transferred to the Department of Infectious Diseases, where a lumbar puncture was performed. The cerebrospinal fluid showed an increased leukocyte count, 32 · 106/L (0–5 · 106/L), increased protein, 0.65 g/L (0.15–0.50 g/L), and positive TPPA antibodies. This was consistent with neurosyphilis, and the patient was diagnosed with secondary stage syphilis with optic neuritis. The patient received intravenous treatment with penicillin 3 g x 4 for 12 days.
The temporal artery biopsy showed no signs of temporal arteritis, and the skin biopsy showed non-specific inflammation. The rash disappeared over the course of two months. Follow-up by the ophthalmologist four months after treatment showed almost total resolution of the central field of vision deficit, and visual acuity had improved from finger counting at 2 m to visual acuity 0.8. Follow-up blood tests by an infectious disease specialist one year later revealed a complete absence of RPR antibodies, indicating successful treatment for neurosyphilis.
Discussion
Syphilis is caused by infection with the spirochete Treponema pallidum. The disease is known as “the great imitator”, as it may present in many ways (2).
Syphilis is rare in Norway, but the incidence is rising. In 2008, 56 cases were recorded, while 231 cases were recorded in 2018. Of the 231 cases, 205 were men who have sex with men (3). Syphilis is transmitted primarily through sexual contact, but the spirochete can also cross the placenta and thereby transmit infection from mother to child. Pregnant women are therefore routinely offered a screening test for syphilis.
In sexual contact, the spirochete penetrates through small abrasions in the skin or mucosa. A painless, indurated lesion, or chancre, forms at the inoculation site. If the chancre is in the vagina, anus or throat, it is not certain that the patient will notice it. Thus primary syphilis may be asymptomatic. The chancre resolves spontaneously, but the spirochete rapidly disseminates systemically. About 25 % of those infected develop symptoms of secondary syphilis (4). Common symptoms are malaise, fever, nausea, sore throat, muscular pain, enlarged lymph nodes, rash and weight loss. Our patient had several of these symptoms and had been examined by doctors from multiple specialties without syphilis being considered as a possible diagnosis.
If the infection had not been diagnosed and treated, the patient would eventually have entered an asymptomatic, latent phase. Tertiary syphilis may appear several decades after the primary infection, and may cause vasculitis in the form of aortitis and aortic aneurisms, degeneration of the central nervous system with paralysis, personality changes and severe pain. Necrotic and inflammatory lesions, or gummas, may affect internal organs, the brain and skin (2).
In the assessment of this patient, it was thought that the aortic aneurism might have been caused by syphilis, but this possibility was rejected, as the history of illness with chancre and syphilis antibodies clearly pinpointed the time of infection. The aortic aneurism had been present for several years prior to the time of infection.
Ocular syphilis can affect almost all parts of the eye in the secondary and tertiary stages of the disease. The most common manifestation is a type of uveitis. Inflammation of the optic nerve, as in our patient, also occurs frequently (5). Our patient had severe vision loss in one eye, and was first misdiagnosed with ischaemic optic neuropathy. Delayed diagnosis is not unusual with ocular syphilis, and may lead to irreversible loss of vision (6). Once the patient was diagnosed with syphilis and treated with penicillin, both visual acuity and field of vision normalised almost completely.
Syphilis is on the rise and can present with a wide variety of symptoms that may resemble many different diseases. If untreated, syphilis can cause severe, irreversible damage to several organ systems. Doctors need to be vigilant, and consider syphilis as a differential diagnosis for a number of conditions, including vision loss. This can save sight and in some cases lives. One should inquire about sexual history and possible chancres, and conduct serological tests if syphilis is suspected. Other sexually transmitted diseases must be excluded (3). If syphilis is confirmed, it must be reported to the Norwegian Surveillance System for Communicable Diseases (MSIS) and the source of infection traced.
This case report demonstrates the importance of a detailed patient history, a broad differential diagnosis and cooperation between specialties.
