Most cases of thoracic injury do not require hospitalisation, but there are multiple potential complications. Haemothorax is among the most common cases requiring treatment. This case report describes an atypical presentation of delayed haemothorax in a patient following rib fractures.
A man in his sixties was a front seat passenger in a collision between two vehicles. Upon arrival in hospital, the trauma team examined the patient. His condition was stable and physical examination only revealed tenderness of the left hemithorax. A CT scan from head to pelvis confirmed multiple fractures on the left 2nd to 9th rib, with sparse surrounding haematoma. There were no signs of intrathoracic or intra-abdominal injuries. During the five-day hospitalisation, he exhibited no signs of respiratory distress and the pain was relieved with oral analgesics.
The patient was readmitted from the outpatient clinic after two weeks. Although he had only experienced mild pain after discharge, the chest X-ray revealed a considerable left-sided pleural effusion. Clinical findings included; left-sided percussive dullness, peripheral oxygen saturation 97 %, blood pressure 138/84 mmHg, heart rate 84 bpm and a haemoglobin concentration at 10.5 g/dL (13.4–17.0 g/dL). A 6 French pigtail drain was used for an ultrasound-guided thoracentesis, and approximately 1 litre of serosanguineous fluid was initially drained. In the days that followed, drainage was limited, despite flushing with 100 mL saline solution three times daily. On the third day, a second X-ray showed a large retained pleural effusion. Treatment with intrapleural fibrinolysis was initiated, in a regime of 10 mg alteplase daily for three days.
After two days of treatment with intrapleural alteplase, the patient became unwell and developed left-sided chest pain. The symptoms subsided when he lay down, following which his blood pressure was 130/80 mmHg, heart rate 70 bpm and the peripheral oxygen concentration 97 %. A total of 400 mL of bloody fluid in the drainage bag was recorded. A few hours later, the patient again became unwell and hypotensive. The blood pressure was now 55/30 mmHg and the haemoglobin concentration had dropped from 9.4 to 8.2 g/dL during the course of the day. The patient received intravenous fluids and a unit of erythrocytes, and his condition stabilised. He was awake and pale, and his blood pressure was 100/60 mmHg. A chest X-ray revealed an increasing pleural effusion (Figure 1). The subsequent chest CT confirmed massive haemothorax with mediastinal deviation and a fatty structure in relation to the diaphragm (Figure 2). Shortly after the scan was taken, the patient’s heart rate had increased to 118 bpm. His blood pressure remained steady at 110/72 mmHg. A thoracostomy was performed urgently with a 28 French chest tube, which immediately drained 1 litre of blood.
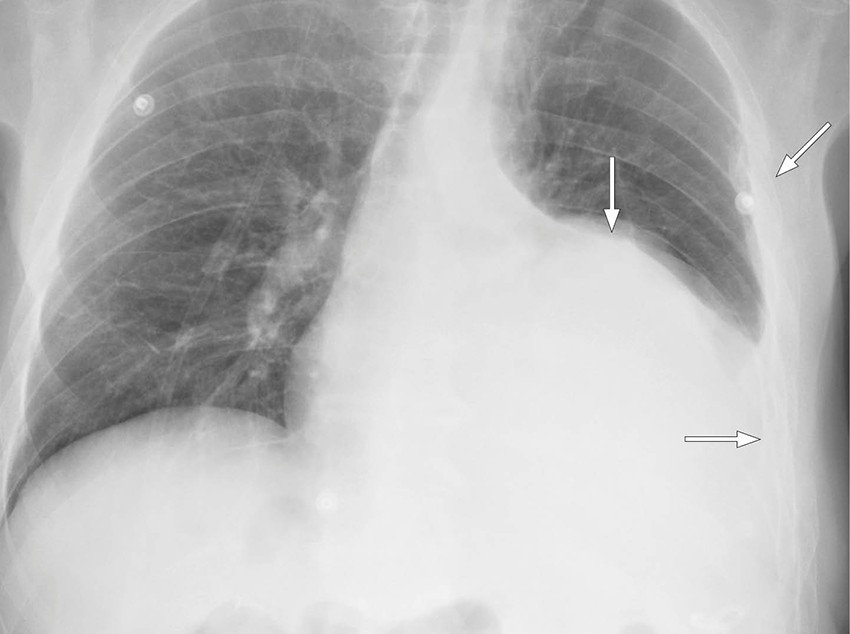
Figure 1 Chest X-ray with multiple left rib fractures and a large pleural effusion.
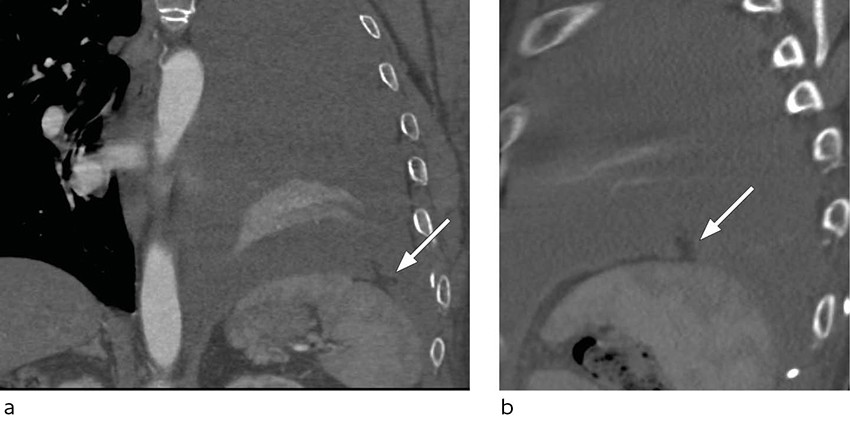
Figure 2 Chest CT with intravenous contrast, in coronal (a) and sagittal (b) plane, with a small defect in the left side of the diaphragm with a small fatty structure protruding up into the pleural cavity, representing the bleeding omentum.
Video-assisted thoracic surgery the same day revealed bleeding omentum protruding through an antero-lateral laceration in the diaphragm. The protruding omentum was excised and the laceration sutured thoracoscopically. A laparoscopy was performed, but no additional lacerations were found. The recovery period was without further complication and the patient was discharged after seven days.
Discussion
The most common trauma mechanisms for blunt thoracic traumas are falls and traffic accidents. The number of rib fractures is associated with trauma energy and the risk of other intrathoracic or extrathoracic injuries (1, 2). At a Norwegian regional trauma centre, haemothorax was diagnosed in 7 % of patients admitted after a thoracic trauma (1). Diaphragmatic injury is reported in under 1 % of cases following blunt thoracic trauma and is associated with a high trauma energy and severe intrathoracic or intra-abdominal injuries (1, 3).
First-line treatment for haemothorax is drainage. Retained haemothorax is seen in 5–30 % of patients and can be complicated by fibrothorax or empyema (4, 5). American guidelines recommend early video-assisted thoracoscopic surgery 3–7 days after the trauma if drainage is unsuccessful (4). Intrapleural fibrinolysis is recommended when there is an increased surgery risk. A recent review of literature on intrapleural alteplase treatment suggests this to be both safe and effective (5). The bleeding rates in the studies included were 0–6.6 %, and the consensus-based contraindications for treatment included surgery, bleeding or trauma within the last two days (5).
In our case study, the standard regime of treatment exacerbated the medical condition before the underlying cause was identified and corrected. Intrapleural alteplase was preferred due to the time passed since the trauma, the patient’s stable condition and his multiple comorbidities, including diabetes and pancreatitis. The CT scan from the patient’s first period of hospitalisation and the subsequent X-rays have been reviewed and show no missed signs of diaphragmatic injury. These injuries are rare and can be clinically and radiologically difficult to diagnose, but should be considered in patients with relevant high-energy traumas.
Most blunt thoracic injuries are considered minor and are treated out of hospital, where the focus traditionally has been to ensure sufficient pain management to prevent delayed functional impairment, respiratory failure and pneumonia. Risk of pneumonia is less than 2 %, while the risk of delayed haemothorax has been reported with an incidence between 7.4–11.8 % following minor thoracic injury (2). Based on a cohort study, a clinical decision rule has been developed in order to identify patients at higher risk of developing haemothorax (2). When treating these patients out of hospital, it is important to be aware of this complication, especially in cases of slow recovery. In patients admitted to hospital because of thoracic trauma, a routine X-ray control after 7–10 days should be considered.