A bang is heard in connection with endoscopic removal of a rectal polyp from a 71 year old patient, and the endoscope is expelled from the rectum. Explosions in the rectum are a rare, but feared, complication of polypectomy that may be avoided by using new knowledge stemming from medical research.
A 71 year old woman was referred to our gastroenterology laboratory as a result of a couple of episodes of fresh rectal bleeding; the most recent occurred two months earlier. She had no other abdominal problems. She was previously well and did not use acetylsalicylic acid, NSAIDs or anticoagulants.
On the basis of available information, the patient was scheduled for a rectosigmoidoscopy. In an examination of patients with fresh red rectal bleeding, particularly if it is fluid, on the outside of the faeces or prior to or after defecation, an endoscopic examination of the rectum and distal colon will be adequate.
In the rectosigmoidoscopy, following evacuation with 240 ml Klyx, we advanced 30 cm inside the anal canal before having to stop owing to poor cleansing more proximally. Distal to this level emptying was reasonably good, but with some small faecal residues (Fig. 1). A large polyp about 3 – 4 cm in dia-meter and with a base estimated to be approximately 2 cm in diameter (Fig. 1) was found a few centimetres inside the anal canal.
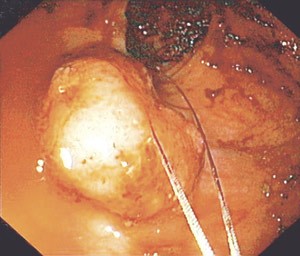
Figure 1 The sessile rectal polyp before resection
Almost all polyps in the colon exceeding 1 cm in diameter are adenomatous, i.e. with a malignant potential if not removed. When polyps of this kind are found, the entire colon must be examined by means of a total colonoscopy, as one in three polyp bearers harbour multiple polyps. The prevalence of adenomatous polyps in the right colon also increases with age. With this patient, we might therefore have postponed the resection of the polyp that had been found until the forthcoming total colonoscopy, but we chose to remove it during this procedure.
It was decided to perform a piecemeal resection of the polyp by means of a polypectomy employing snare diathermy. The resection was performed without complications until the polyp had been shaved right down. There was slight blood seepage from the resection site, but we chose to cauterise carefully with the snare.
Clinically significant bleeding occurs in 0.5 – 2 per cent of polypectomies, and figures as high as 6.1 per cent (1) have been recorded. Slight bleeding occurs more frequently, as in the case of our patient. This will often stop spontaneously, but as a rule prefers to ensure this. There are a number of endoscopic methods for stopping bleeding, such as submucosal injection of dilute adrenaline, argon plasma coagulation (APC), clips and ligation of the polyp stem with an endoloop prior to resection. Perhaps the simplest method for the most limited bleeding is to use what is at hand, i.e. to cauterise with the snare.
We therefore placed the almost closed snare on the resection site, and cauterised with diathermy. The next moment there was a loud bang and the whole endoscope was expelled from the anus. Repeat endoscopy after a few minutes revealed no signs of damage to the mucosa, and the patient complained only of slight tenderness in the lower abdomen. The discomfort ceased after a short time. An X-ray overview of the abdomen taken after the examination showed no signs of free air. The patient was therefore discharged with instructions to contact us in the event of symptoms. At a repeat total colonoscopy a month later, the patient reported that she had experienced no further problems. A lactose breath test taken somewhat later showed that she is a methane producer (Fig. 2).
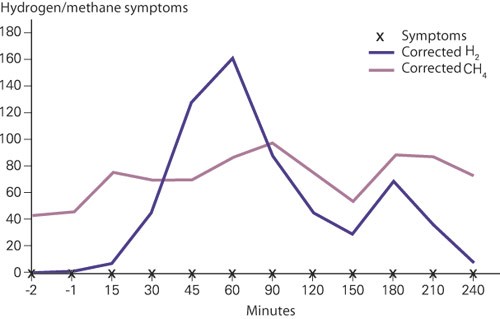
Figure 2 The patient’s hydrogen/methane breath test after intake of 25 g lactose. The H₂ level rises when the substrate reaches the colon, while CH₄ production takes place only in the left colon, and is not affected by the addition of substrate on the right side. A persistently high level of CH₄ shows that the patient is a methane producer. A rise in the H₂ level shows that the patient has lactose intolerance (malabsorption)
It took a little while to understand that we had experienced a gas explosion in the rectum. The whole polyp had been resected with the snare without problems, but only when we cauterised the surface of the resection, and probably created a small electrospark, did ignition take place. Fortunately, this happened in the rectum, so that the gas could be evacuated spontaneously through the anus. Episodes of this kind further up in the intestine can have serious consequences, and fatal outcomes have been described. If perforation had occurred, the patient would have developed symptoms. An X-ray overview of the abdomen showed that there was no free air, and the patient was therefore not admitted for observation, but was told to get in touch if symptoms developed.
Discussion
Gas explosions are a rare phenomenon in connection with endoscopy. As far as we know, they have not been reported previously in Norway, although there may have been occurrences.
Gasses in the intestine are due to swallowed air, bacterial production, chemical reactions and absorption from the blood. 99 per cent of intestinal gas consists of:
The atmospheric gases (blood gases): nitrogen (N₂), oxygen (O₂) and carbon dioxide (CO₂)
Those produced by bacterial action: hydrogen (H₂), methane (CH₄) and CO₂.
Three quarters of the gasses in the colon are of bacterial origin; the remainder consists largely of N₂. The only combustible gases are H₂ and CH₄. Approximately 33 per cent of the population have a bacterial flora in their faeces that produces CH₄ (methane producers), while more than 95 per cent of the population produce H₂. Flatus can contain up to 44 per cent H₂ and 34 per cent CH₄. Studies have shown that H₂ in a concentration of 4 – 72 per cent and CH₄ in a concentration of 5 – 15 per cent is flammable given an oxygen concentration of more than 5 per cent (2).
All types of gastrointestinal endoscopy are dependent on insufflation of gas to inflate the intestine and thereby ensure good visualisation. At most hospitals, the standard insufflation gas is ordinary atmospheric air. In the 1970s and 1980s gas explosions with fatal outcomes were reported in connection with diathermal treatment during colonoscopy (3, 4). Explosions are contingent on the presence of oxygen in the colon. The partial pressure of O₂ in the colon is normally very low. As air contains O₂, a prerequisite for an explosion during a colonoscopy is air insufflation. Production of H₂ or CH₄ is also necessary. This is dependent on a substrate and bacteria, as in the case of an incompletely cleansed bowel in the area. Methane producers have an intestinal bacterial flora with methane-producing bacteria that consume virtually all H₂ and convert it into CH₄. Methane-producing bacteria occur largely in the left half of the colon, so that methane producers will have an H₂ atmosphere in the right colon and a CH₄ atmosphere in the left colon and rectum. Since the patient’s lactose breath test showed that she was a methane producer (Fig. 2), we must assume that we experienced a methane gas explosion.
In the 1970s and 1980s the bowel was emptied with the aid of a fluid diet and laxative, or perorally with mannitol before colonoscopy. Mannitol forms a substrate for intestinal bacteria formation that may lead to high production of H₂ and CH₄. A study of the intracolonic gases in 20 patients who were examined by means of colonoscopy without gas insufflation was compared with a study of 20 patients for whom insufflation with ordinary air was used (5). Almost all the patients had been evacuated with mannitol. None of the patients with ordinary air insufflation had explosive levels of H₂ or CH₄, but almost all had an O₂ concentration of over 5 per cent. In the group without air insufflation, six patients had explosive levels of H₂ or CH₄, and one of them also had an O2 concentration of over 5 per cent. 20 per cent of the methane producers also had an excessive level of CH₄. In a later study, 30 patients were examined who were cleansed with polyethylene glycol (PEG) prior to colonoscopy. None of these patients were found to have an explosive level of H₂ or CH₄ (6). An equally large group were evacuated with sodium phosphate enema for signoidoscopy, and two patients were found to have an elevated H₂ level, and in one of them the level of CH₄ was too high. However, the concentration of O₂ was not measured in this study. This may thus imply that in modern bowel preparation methods for total colonoscopy, explosive conditions are rarely or never created in the bowel. However, the possibility cannot be excluded as long as O₂ is introduced through air insufflation.
Our patient was evacuated by means of sorbitol enema, which is the most common means used in Norway prior to rectosigmoidoscopy, in contrast to the practice abroad. Since sorbitol, unlike PEG and sodium phosphate, can provide a substrate for bacterial gas formation, there is theoretically a greater risk of a gas explosion when this cleansing method is used.
CO₂ insufflation
Insufflation with carbon dioxide (CO₂) instead of air eliminates the risk of explosion in connection with gastrointestinal endoscopy, because CO₂ gas does not contain O₂, which is essential to the formation of explosive gas mixtures in the colon. However, there are also other good reasons for recommending CO₂ insufflation in connection with colonoscopy. It is now well documented that patients who are insufflated with CO₂ instead of air experience significantly less discomfort in the 24 hours following both sigmoidoscopy (7) and colonoscopy (8), and at the same time no side effects. An hour after colonoscopy, about 45 per cent of the patients experienced abdominal discomfort after ordinary air insufflation, compared with 10 per cent after using CO₂ (8). The explanation is relatively simple. In an average colonoscopy, about 8 l of gas is insufflated, only some of which exsufflated when the scope is withdrawn. The absorption of this gas into the blood depends on the partial pressure difference between the blood and the intestinal lumen. Air contains mainly N₂ (78 per cent), which will result in the same partial pressure in blood. As a result, there will be no partial pressure differential, and minimal absorption. Moreover, blood has little N2 carrier capacity. The opposite applies to CO₂, which has a low partial pressure in blood, and will therefore be absorbed rapidly. It is claimed that CO₂ gas has a half-life of two minutes in the bowel, while air (N₂) can remain for hours until it is eliminated. These gas problems after colonoscopy may be very uncomfortable for patients. Nor does CO₂ insufflation create any problems for the scopist, since the bowel is inflated far enough in front of the scope for the difference not to be noticeable.
Conclusion
The risk of a gas explosion as a result of using diathermy during colonoscopy is small and depends on the presence of the correct mixture of explosive gases, which inpractice will largely result today from enema evacuation without entirely successful cleansing. CO₂ insufflation prevents this possibility of explosion. A more important reason for recommending CO₂ insufflation is that it saves patients from too much gas-induced pain after lower endoscopy.