The Communicable Diseases Control Act (1995) requires all Norwegian health institutions to record, analyse and report hospital infections. The Norwegian Institute of Public Health set up a national register for postoperative hospital infections, NOIS (1), in 2005. All hospitals are required to report to the register for the same three-month period every year. 18 prevalence studies of hospital infections have been carried out in Norway the last 2 decades. Several of these have been published in the Journal of the Norwegian Medical Association, and the results vary greatly. According to the studies, 3 - 16 % of the patients in somatic hospitals have had a hospital infection at some time (2, 3). In a larger prevalence study from the U.K., 5.6 % of the patients had a postoperative surgical site infection (SSI) (4). Cruse & Foord claim, in their classic study from 1980, that in the case of clean operations fewer than 2 % of the patients should have a deep or superficial SSI (5).
This article presents the results of 7 years’ consecutive recording of SSIs after orthopaedic surgery and the various preventive measures set in motion. After an analysis of the data, we discuss the possible causes of SSIs in a hospital within our category. Consequences of the analyses are discussed.
Material and methods
A committee was appointed at Blefjell Hospital, Kongsberg, in the autumn of 1997, and given the name Find and Win. Its task was to undertake continuous SSI surveillance. The committee based their work on the recording done by Aamodt and colleagues in 1989 and 1990 (6). The hospital management, heads of department, staff at the convalescent homes and the GPs who used the hospital were informed about the recording before the start.
We recorded nine types of orthopaedic surgery in the period 1.2. 1998 - 31.12. 2004 (tab 1). The surgery department (built in 1968) performed both orthopaedic and general surgery. A separate operating theatre was allotted for orthopaedic implant surgery (without being isolated from the rest of the surgery department). The theatre was only for clean operations and the ventilation system provided fresh air 8 - 10 times an hour. 37 total hip replacements were carried out in a newly built surgical outpatient centre the autumn 2004.
|
Table 1 Deep and superficial infections after 2 421 surgical procedures at Blefjell hospital in the period 1.2. 1998 - 31.12. 2004
|
|
Deep infection
|
Superficial infection
|
|
Number and percentage (%) (95 % CI)
|
Number and percentage (%) (95 % CI)
|
|
Primary total hip replacement
|
28/753 3.7 (2.4 - 5.0)
|
44/753 5.8 (3.1 - 7.5)
|
|
Hemi-arthroplasty in hip
|
10/202 5.0 (2.0 - 8.0)
|
22/202 10.9 (6.6 - 15.2)
|
|
Prolapse and stenosis operations and intertransversal fixation without implant
|
1/571 0.2 (0 - 0.6)
|
10/571 1.8 (0.7 - 2.9)
|
|
Dynamic compression screw in hip
|
10/131 7.6 (3.1 - 12.1)
|
5/131 3.8 (0.5 - 7.1)
|
|
Gamma nail for proxmal femur/hip fracture
|
2/130 1.5 (0 - 3.6)
|
6/130 4.6 (1.0 - 8.2)
|
|
Hip intramedullary nailing
|
1/187 0.5 (0 - 1.5)
|
3/187 1.6 (0 - 3.4)
|
|
Total knee replacement
|
1/212 0.5 (0 - 1.4)
|
8/212 3.8 (1.2 - 6.4)
|
|
Unicondylar knee replacement
|
1/55 1.8 (0 - 5.2)
|
0/55 0
|
|
Ankle fracture (nail/screw plate)
|
2/180 1.1 (0 - 2.6)
|
4/180 2,2 (0.1 - 4.3)
|
|
Total
|
56/2 421 2.3 (1.7 - 2.9)
|
102/2 421 4.2 (3.4 - 5.0)
|
consultant posts within surgery/orthopaedics in 1998. Two new consultant posts in orthopaedics were added in 2001. 753 primary total hip replacements were performed: 715 by six full-time orthopaedic surgeons and 38 by hired locums.
Data collection
Infections were recorded in a form based on the same template used by Aamodt and colleagues (6), and equivalent to that now used by the Norwegian Institute of Public Health (fig 1). The form has two pages. Page 1 was filled in when the patient was in hospital. Page 2 and a stamped addressed envelope were given to the patient on discharge, it was filled in by the patient or medical staff and returned within four weeks. SSIs were defined in accordance with recommendations from Centers for Disease Control and Prevention (CDC) in Atlanta, USA and this information was printed on the back of page 2. As a reminder to medical staff that the patient was included in the SSI records and as an encouragement to fill in the forms, the patient’s medical record was given a black and yellow sticker with a black and yellow sticker containing a drawing of «Mr. Detective and his magnifying glass». An operating room nurse, who was given 25 % of the available working time for this work, was responsible for recording and follow-up. If the form had not been returned by 2 - 4 weeks after the due date, the patients were contacted via phone, letter, their regular GP, the convalescent home, nursing home or nearest relative. The same orthopaedic surgeon (from Find and Win) assessed assessed all the recorded infections. Quarterly reports on the incidence of infection were sent to the hospital management, head consultant, all surgeons and heads of department on the wards. Furthermore, all surgeons received personal feedback about the operations they had performed.
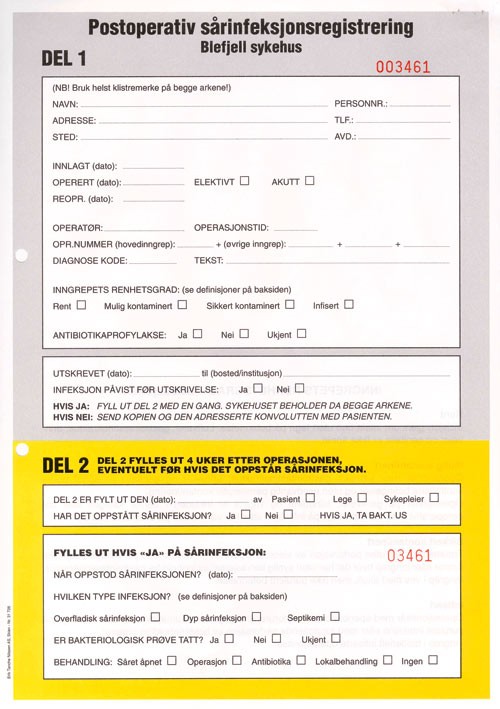
Figure 1 Form used for recording postoperative hospital infections
Other information
In addition to the questions on the form, information was retrieved about pre-operative haemoglobin values, other diseases (diabetes, heart failure, cancer, senile dementia), use of special medication (cortisone, non-steroid anti-inflammatory drugs, acetylsalicylic acid), preoperative and postoperative length of stay, blood transfusions, and whether it was a primary or revision hip replacement. With total hip replacements the peroperative bleeding and length of operation were also recorded. Intravenous prophylactic antibiotics were given in all replacement surgery: i.e. 2g cephalotine i.v every 6 hours four times. With cemented implants, cement with gentamacin was used. For bone marrow nails and ankle fracture operations, all the patients should in principle have received prophylaxis but 10 % of patients with bone marrow nail operations and 40 % of those with ankle fractures did not in fact do so. In the case of intramedullary nailing of femoral neck fractures it was up to the individual surgeon to decide if antibiotics should be given.
Air freshness in the operating theatres was regularly checked by measuring the colony forming units per m3 (CFU/m3). In parallel with this, all category 1 preventive measures recommended by the CDC were updated in the surgical department and on the three surgical wards (2).
Results
The study included 2 421 patients, of whom 1 555 are women (64 %). 63 patients were excluded: 57 died within four weeks postoperatively and six were reoperated with the same incision at another hospital during the observation period, with no infection recorded up to that point.
48 % of the patients replied after 4 weeks and all but one replied after a reminder. 158 infections were recorded with an average of 6.5 %. Annual variations were from 4.8 % to 10.5 %. 56 infections (2.3 %) were deep and 102 (4.2 %) superficial. 28 of 56 deep infections arose in total hip replacements (tab 1). In the quarterly reports for the whole material, the infection frequency was 1.6 % - 8.9 %.
There was no connection between infection incidence and factors such as preoperative length of hospital stay, underlying illnesses in the patient, haemoglobin level, use of medicine and the personal composition of the operating team (data not shown).
Antibiotic prophylaxis was given to a total of 1 588 patients (58 %). Table 2 shows the incidence of deep infections for acute and elective surgery with and without antibiotic prophylaxis. Positive cultures were found in 59 of 72 patients operated for total hip replacements. Yellow staphylococci were identified in 62 % of the infections, white coagulase-negative staphylococci were found in 23 % and other types (Enterococci, Klebsiella, E.coli, Pseudomona, Coryne bacteria) in 15 % of the cases.
|
Table 2 Incidence of deep infections for elective and acute procedures with and without antibiotic prophylaxis
|
|
Number
|
Deep infection
|
Incidence (%) (95 % CI)
|
|
Elective procedure
|
|
|
|
|
With prophylaxis
|
1 275
|
40
|
3.1 (2.1 - 4.1)
|
|
Without prophylaxis
|
518
|
1
|
0.2 (0 - 0.4)
|
|
Acute procedure
|
|
|
|
|
With prophylaxis
|
313
|
10
|
3.2 (1.2 - 5.2)
|
|
Without prophylaxis
|
315
|
5
|
1.6 (0.2 - 3.0)
|
During the first year, we recorded when the postoperative infections were discovered. 28 % were found while the patient was in hospital, 72 % after discharge.
The normal length of hospitalisation after a total hip replacement was 7 days. In the study period there were 1 678 extra days in hospital because of infections; 1 430 of these concerned patients who had received a total hip replacement. 195 extra days in 2004 were due to one patient who had a deep infection after revision because of dislocations in a primary total hip replacement.
During the entire period, air samples were taken in the theatres used for orthopaedic surgery. From January 1999 there was a marked decline in colony forming units after the introduction of ultra-clean air systems, helmets and reduced traffic in and out of the theatre. Table 3 shows the tactics employed and the result of the air measurements.
|
Table 3 Measurement of colony forming units per m3 air, CFU/m3 and preventive action taken
|
|
Year
|
CFU/m3
|
Action
|
|
1997 - theatre 3
|
41.5
|
|
|
1998 - theatre 3
|
45.4 - 47.7 - 73.3
|
|
|
1999 - theatre 3
|
0.4 - 19.1 - 9.1 - 14.2
|
Introduction of clean air suite, helmets, change of filter in ventilation system, telephone/cupboard in theatre, education, attitude formation
|
|
2000 - theatre 3
|
0,3
|
|
|
2001 - theatre 3
|
16.6 - 2.1 - 1.9
|
|
|
2002
|
No measurements
|
New autoclaves; whole ventilation system cleaned
|
|
2003 - theatre 1
|
7.2 - 11.5
|
Changed to theatre suite with own preparation room
|
|
2004
|
No measurements
|
New instrument washing machine in surgical department
|
We found no connection between deep infections and the time of day when the operation took place; or between the incidence of superficial and deep infections with each surgeon (data not shown). Multivariate regression analysis of the connection between deep infections after surgery for primary total hip replacement showed significant associations between deep infection and the age group 65 - 74 years (adjusted odds ratio 4.7; 95 % CI 1.3 - 17.3) and for one of the surgeons (adjusted odds ratio 5.7; 95 % CI 1.9 - 17.3) after assessing preoperative length of hospital stay, peroperative bleeding, length of operation, age, operation theatre and type of prosthesis (cemented or uncemented) as variables.
Discussion
Blefjell Hospital, Kongsberg, is a medium-sized local hospital. Between 1 700 and 2 000 large and small operations are performed in the surgical department annually; and between 1 000 and 1 100 operations in the outpatient department. The choice of type of operation to record was based on three considerations: that orthopaedic surgery involves a relatively large part of the hospital; that infections after orthopaedic surgery have important consequences and that SSIs in orthopaedic patients are considered to be a good indicator of quality. In the period 2001 - 03, infections were also recorded after operations for hernia, varicose veins, breast tumour, hallux valgus and the removal of fracture fixation implants (a total of 315 patients). There is a lot of work involved in post discharge surveillance and the frequency of infection was relatively low (four deep and six superficial infections), so we decided to stop monitoring these operations.
The strength of the study is that all the patients were monitored for four weeks postoperatively and the follow-up was almost 100 %. The follow-up was demanding because the recording depended on many links both within and outside the hospital. It was made more difficult by the negative attitudes of certain orthopaedic and general surgeons and among the nursing staff. The report forms were not filled in, torn in shreds or boycotted in some other way. All patients that were meant to be included were registered anyway because the nurse regularly checked the operation records. It could not be taken for granted that infections arising after the four weeks would be reported to the hospital. Much of the nurse’s time was spent on following up the report forms both internally in the hospital and after discharge.
Postoperative hospitalisation is ever shorter. The high number of infections after discharge underlines the importance of monitoring patients also after their time in hospital. This fact is supported by other studies (1, 5, 7).
Similar studies at other Norwegian hospitals have not previously been published. This makes it hard to be certain of what our figures actually say about the hospital’s standard. After the introduction of preventive measures in 1999 and 2000, there was a temporary reduction in infections. From 2001 the number of hospital surgeons rose and as a result there were more operations. Uncemented total hip replacements were mainly used.
During the second and third quarter of 2003, unacceptable numbers of deep infections were recorded for total hip replacements. Elective orthopaedic implant surgery was therefore moved from theatre 3 to theatre 1. This had an adjacent room and the possibility of bringing in equipment through airlocks during operations. When the 2003 total hip replacement results emerged, during spring 2004, still with an unacceptably high deep infection frequency, it was decided to stop these operations in the general surgery department. They were moved to the outpatient centre because the operating theatres there had a Weiss ceiling with about 20 changes of air per hour. The same staff performed the operations. The change of theatre did not lead to any change in the frequency of infections following hip implants.
The Norwegian Arthroplasty Register’s report for 2005 shows that the incidence for primary total implant reoperations caused by deep infections, has lain between 1.3 % and 2.0 % in recent years (8). The figures for deep infection recorded in the hip register are based on implant replacement. It is believed that these figures represent about half of the deep hip prosthesis infections. This agrees with our findings. Of our in all 28 deep infections, revision with replacement of implants was performed on 14 patients. The others were successfully treated with local debridement and antibiotics. The figures in the national arthroplasty register come from all Norwegian hospitals and represent both combined and purely orthopaedic departments. On the basis of these figures and the type of surgical departments, one can estimate the expected frequency of postoperative deep infections to be 2 - 4 %.
The quarterly reports show great fluctuations. It is important to be aware of this when assessing the three months’ infection record now to be reported. When a sufficiently high number of hospitals participate in the recording, we will have a reasonably good measurement of the hospitals’ average standard. An evaluation of one hospital against another on the basis of quarterly analysis can be misleading. In the monitoring of surgical site infections it is important to analyse the deep and superficial infections separately. Deep infections are believed to arise peroperatively and cause the greatest stress both for patients and society (5).
Our finding, which indicates a link between the surgeon and deep infection after primary total hip replacement, is sensitive and challenging. Cruse & Foord, who also documented a surgeon factor, point out that extremely thorough operation techniques reduce the risk of postoperative infection. The number of deep surgical site infections ought to result in more attention to operation techniques. This is the responsibility of both the surgeon and the head of department.
We found no connection between the number of superficial and deep infections with individual surgeons. This may indicate that superficial infections, most probably, result from postoperative treatment, washing, bandage changing etc. on the wards and in the convalescent homes, and the patients’ own personal hygiene. Superficial infections represent a risk and should not be trivialized.
The 1 430 extra days in hospital because of hip infection are equivalent to new total hip replacements for 29 patients. With a hospital reimbursement (diagnosis-related-group) of (on average) 50 % of the actual costs, this represents a loss of income for the hospital of around 2 million kroner annually.
Conclusion
Systematic recording of surgical site infections is a useful tool for quality assurance in surgery. Nearly three quarters of the infections were first discovered after the patients had been discharged. Quarterly reports over seven years show great variations in the incidence rate. Surveillance of infections should be continuous with follow-up for 4 weeks postoperatively for soft tissue procedures and up to a year for implant surgery. There were marked differences between surgeons regarding the number of deep infections after primary total hip replacement. Attention should be paid to improving hygienic standards.