600 patients are annually admitted to Norwegian hospitals for burns (1). Treatment and follow-up of patients with extensive burns is medically demanding. It is expensive and the costs comprise acute treatment and training as well as rehabilitation. Some become chronically disabled and a number of patients will eventually need one or more reconstructive procedures.
The Burn Centre at Haukeland University Hospital opened in September 1984 and has a national function for advanced treatment of burns. The Centre receives patients with extensive burn injuries, burns with difficult localizations (face, hands genitalia) and high-voltage injuries from the entire country. A lack of critical care nurses limited the capacity the first 4 - 5 years. Since 1989, the Centre has received most patients that have needed referral to a specialist department. Only a few patients have been transferred to Sweden because of capacity problems.
The Centre functions as an intensive care unit for burn patients across all ages, also if there is a need for respirator or renal replacement treatment. The Centre was first established with eight beds of which four were for intensive care. Necessary upgrading of the premises was done in 2006. Experience shows that it has been difficult to manage to care for as many as three patients with burns requiring intensive care for more than 10 - 14 days. In this article we present our experience from 20 years of operation.
Material and methods
All stays in the Burn Centre from September 1984 to the end of 2004 with ICD-10 codes T20-T32 or T75 (burns, corrosive injuries or injuries caused by electricity) (2), or corresponding codes from ICD-9 were identified through a search in the hospital’s patient administrative system (PIMS).
A paper-based overview of all stays at the Centre was also used to identify patient stays that were not captured by the electronic search (n = 11).
Stays at the Burn Centre for other reasons than burns (n = 28) and readmissions or stays in connection with reconstructive procedures (n = 30) were recorded, but have not been included in the statistical calculation. Patients who were only treated as out-patients have not been included.
The extent of the injury is expressed as the sum of the partial skin injury and full thickness skin injury in percentage of the body surface, and is taken from a manually completed protocol and medical records. Mortality is expressed as number of deaths during hospitalization. Length of stay is calculated as the date for discharge from the Centre minus the date for admission. The number of inhabitants in the home county is taken from Statistics Norway 1994 (3).
The Data Inspectorate has given us permission to use these health data. The study has not been presented to an ethics committee, in accordance with previous statements from the Regional Committee for Medical and Health Research Ethics that it is not necessary to present quality assurance studies.
Statistics
The results are presented as mean ± standard deviation (SD). One-way variation analysis, chi square test and Mann-Whitney’s test were used to compare groups. P < 0.05 is considered statistically significant.
Results
1 294 (917 [71 %] men) stays caused by burns, corrosive injuries or electrical burns were recorded for the period September 1984- December 2004 (fig 1).
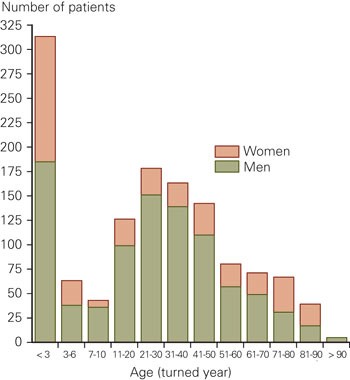
Figure 1 Number of patients admitted for burns 1984 - 2004, by age and sex
The mean age was 29.6 years (SD 24.9; median 27.0). 313 patients (24 %) were less than three years. The mean injured body surface was 19.5 % (SD 18.3; median 15.0) (fig 2). 458 stays (35 %) were for burns involving less than 10 % of the body surface area. For the entire 20-year period only 52 patients (4 %) had a burn that affected 60 % or more of the body surface (fig 2).

Figure 2 Number of patients 1984 - 2004, by injured skin area
The numbers for 1984 cover only four months of operation. In 1998, the situation was special in that the Centre had to shut down for three months after an outbreak of infection in the Centre (4). During the other years the number of admissions for burns was between 47 and 81 (tab 1). There is a certain variation in the number of admissions from year to year, but there is no clear tendency for the number of admissions to change over time.
|
Table 1 Number of patients and length of stay by year of admission
|
|
Year
|
Patients
|
Hospital days
|
|
1984¹
|
19
|
310
|
|
1985
|
56
|
1 188
|
|
1986
|
67
|
1 258
|
|
1987
|
52
|
923
|
|
1988
|
65
|
1 390
|
|
1989
|
72
|
1 516
|
|
1990
|
75
|
1 638
|
|
1991
|
80
|
1 616
|
|
1992
|
57
|
1 453
|
|
1993
|
57
|
1 249
|
|
1994
|
69
|
1 395
|
|
1995
|
76
|
1 285
|
|
1996
|
60
|
1 093
|
|
1997
|
62
|
1 294
|
|
1998
|
43
|
771
|
|
1999
|
47
|
939
|
|
2000
|
66
|
1 119
|
|
2001
|
65
|
1 010
|
|
2002
|
81
|
1 247
|
|
2003
|
51
|
939
|
|
2004
|
74
|
1 588
|
|
[i]
|
The annual hospital days burns in years with normal operation is 923 - 1 638 days and annual variation mainly reflects the number of treated patients (tab 1). The mean length of stay was 19.5 days (SD 19.8; median 14.0). During this 20-year period, only one patient was admitted later with a new burn injury.
The mean association between length of stay and injured area has been used as a parameter of treatment effectiveness. For all stays the association between length of stay and injured area was 1.7 days/ % injured area (SD 3.3; median 1.1).
140 patients died before discharge. These were significantly older and more extensive injuries than the 1 154 patients that were discharged alive (tab 2).
|
Table 2 Patients discharged alive versus patients who died during hospitalization. Mean (± SD) for age, injured area and length of stay. The Mann-Whitney test was used to compare groups.
|
|
Discharged alive (n = 1 154)
|
Died during admission (n = 140)
|
P-value
|
|
Age (years)
|
26.4 (23.2)
|
55.7 (23.0)
|
P < 0.001
|
|
Injured area (% of the body surface)
|
16.4 (14.1)
|
46.0 (25.8)
|
P < 0.001
|
|
Length of stay (days)
|
20.3 (20.1)
|
13.2 (15.9)
|
P < 0.001
|
Assessment of five-year periods showed a tendency towards a smaller injured area and a shorter length of stay during the last five-year period (tab 3). Despite of various burn preventive measures we did not observe a reduction in the number of burn patients that were transferred to Haukeland (tab 3).
|
Table 3 Treatment for burn injuries at Haukeland University Hospital over five-year periods. Mean (± SD) for age, injured area and length of stay. One- way analysis (ANOVA) was used to compare groups and a chi square test was used to test for mortality trends
|
|
Time-period
|
Number of patients
|
Age (year)
|
Injured area (% of body surface)
|
In-patient days
|
Mortality (%)
|
|
1985 - 89
|
312
|
28.6 (23.0)
|
22.7 (21.0)
|
20.1 (21.9)
|
9.3
|
|
1990 - 94
|
338
|
32.5 (26.5)
|
20.7 (18,6)
|
21.7 (21,2)
|
14.5
|
|
1995 - 99
|
288
|
31.2 (26.0)
|
18.2 (16,3)
|
18.7 (18,4)
|
12.2
|
|
2000 - 04
|
337
|
26.4 (23.8)
|
16.5 (16,5)
|
17.6 (17,6)
|
7.7
|
|
P-value
|
|
0.008
|
< 0.001
|
0.042
|
0.31
|
In figure 3, all patients are categorized according to age - and mortality is given for each group. A burn that affected 60 % of the body surface would give about a 50 % chance of survival across all age groups (fig 4).
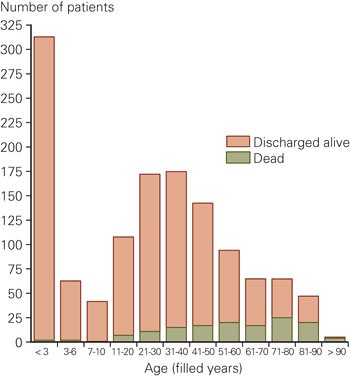
Figure 3 Mortality by age

Figure 4 Mortality by injured skin area
On average 1.50 hospital stays/100 000 inhabitants were recorded per year. If patients from Hordaland are not counted (where Haukeland is the local hospital), a mean of 1.17 patients/100 000 inhabitants were transferred to the Burn Centre (fig 5). The lowest frequency of transferral was from Oslo, Telemark, Rogaland and Troms.

Figure 5 Number of stays annually per 100 000 inhabitants in the home county (n = 1 294 stays). The stipled line shows the average for all counties except Hordaland.
Discussion
Patients with burn injuries are a heterogenous patient group with respect to age, depth and extent of injury. A small, but deep burn of a hand or in the face may have substantial functional or cosmetic consequences. A deep burn that affects large areas of the body can be life-threatening and often requires several operations. In some cases, lack of available skin for transplants may prolong treatment for several months.
71 % of patients were men and 24 % were less than three years (fig 1). This is in accordance with fairly recent data from Swedish hospitals (1987 - 2004), where men accounted for 69 % of all stays caused by burns and 27 % of the patients were less than five years (5).
Extensive burns may be life-threatening for the patient; hospital mortality was 10.8 % in our material. For ten patients (0.8 %) for whom the extent of the injury, the age and premorbid condition gave them such a grave prognosis that there was not a realistic chance of survival transfer was arranged for palliative treatment closer to family and home. The real mortality from burn damage will therefore be somewhat higher than that deducted from solely status upon discharge.
Our material cannot easily be compared directly with burn material from other hospitals. Clinical burn injury material often varies substantially with respect to proportion of children, causes of injury, prevalence of inhalation injury and local practice for transfer of patients between hospitals. We find a survival which is approximately in line with results in a larger American material from 1991 to 93 (in the middle of our study period) (6).
For 52 (4 %) of our patients the burn injuries covered more than 60 % of the body surface. Taking into account the uncertainty contained in a limited number of extensive injuries, a patient with a burn of about 60 % of the body’s surface has approximately a 50 % chance of survival (all age groups assessed together), fig 4. This is in line with findings in an American material where the mortality was 47.5 % among 673 burn patients with injuries of about 60 - 69 % of the body’s surface (7).
The burn- injured patient’s problems are not solved when the wounds are healed upon discharge. For many patients with large burns, a long and demanding rehabilitation period awaits. In a follow-up of 999 patients discharged in 1984 - 1999 we found that among patients with previous burns the risk of sudden or violent death was ten times higher than in the adult population as a whole (8).
Inhalation injury secondary to inhalation of toxic combustion products increases the risk to die as a consequence of a burn. Among 1 665 patients treated at two Boston hospitals in 1990 - 94, three risk factors for death were found: age > 60 years, injured area > 40 % of the body surface and inhalation injury (9).
Several conditions cause the length of stay in the Burn Centre to be somewhat lower than the total hospital stay. With a large demand some patients with wounds in healing or small wounds have been treated in a plastic surgery ward. Total stay at Haukeland may therefore be somewhat longer than what has been recorded as stay in the Burn Centre. In an opposite direction points that after the patient hotel opened in 1998, some patients with healing wounds have been able to stay overnight there, but with daily wound treatment and assessment in the ward.
After skin grafting and with healing wounds, some patients have been returned to complete treatment in their home hospitals. We were not able to describe the duration of the burn treatment for patients who were moved back to their home hospitals because we could not couple databases from different hospitals. We were not able to describe the duration of the burn treatment for patients who were moved back to their home hospitals because we could not couple databases from different hospitals.
The same applies to patients (most often those with very extensive and deep injuries) that have been transferred to other hospitals (most often at Sunnaas hospital) for more specialised rehabilitation after having completed treatment with us.
Palliative treatment
Cumbersome and long lasting treatment of extensive burn injuries in old people, or in patients with additional serious chronic disease, will in some cases have very small chances of succeeding. Especially flame injuries tend to be deeper one day after the incidence occurred than it seemed to be after a few hours. Full thickness skin burns demand operative treatment with removal of injured skin and coverage with skin transplants. It may be especially difficult to recover from deep burn injuries in lower extremities if there is already a marginal arterial circulation or to heal a large, deeply injured skin area on the back or the buttocks.
In the period 1984 - 2004, 47 patients in the Centre died after having stayed there for less than three days (mean injured area 57.3 % [SD 24.3]; mean age 58.9 years [SD 22.1]). Retrospectively, it is difficult to determine whether these patients only received palliative treatment. In addition, some patients were moved in order to receive palliative treatment at their home hospital. Searches in the National Register revealed that seven patients with less than seven days of stay at Haukeland were dead 0 - 12 days after discharge; the majority of these must have been moved back to their local hospitals for palliative treatment.
It is important to have an open discussion with the primary hospitals before moving a patient, this should also concern the patient’s general status and premorbid condition. One may in this way avoid transferring patients for whom palliative treatment would have been the best option from the start. Effective fluid treatment in a start and transport phase will often stabilise the patients’ circulation so well that the process lasts longer than if one had just given purely palliative treatment from the beginning. Transferral of digital images may in many cases be useful in a discussion on whether active and extensive surgery will be realistic in relation to the extent and depth of the injury.
A palliative treatment regimen for very seriously burned patients in primary hospitals may be demanding. Relatives will usually expect all possible measures to be tried and the situation may last for several days. We still perceive it as important that patients with burn injuries without a realistic hope of survival are mainly offered palliative measures and treatment in a hospital close to home and family.
National function
In a review of highly specialized national services in 2005, Rasmussen & Bratlid commented that counties localized near monopoly institutions used highly specialized services to a larger degree than others (10). We see no such tendency for seriously injured patients in our material. Haukeland is the local hospital for patients from Hordaland, and as expected we found relatively more stays for patients with smaller burn injuries from Hordaland than from other counties. 73 % of the stays and 85 % of all in-patient days were still for patients outside of Hordaland. Number of patients across counties was otherwise evenly distributed (fig 5), but with somewhat fewer admissions from Oslo, Telemark, Rogaland and Troms (which all have hospitals with plastic surgery departments).
Change in number of patients over time
A recent survey from Sweden reported that the number of hospital stays for burn- injured patients was reduced with 30 % in the period 1987 - 2004 (5). It is not clear to what extent this is a real decrease or whether it mainly reflects an increased degree of out-patient treatment of smaller burns. With the presumption that our material cannot clarify whether practice for referrals to Haukeland has changed in the period 1984 - 2004, we find that during a 20-year period the number of patients annually transferred with burn injuries has not changed, even if we notice a slight trend towards a somewhat smaller injured skin area (tab 3).