Weight loss in overweight women often enhances fertility. However, pregnancy is not recommended in the first year after bariatric surgery, because of an increased risk of nutritional disorder. We present a woman who became pregnant in a phase with rapid weight loss after bariatric surgery.
The patient had been overweight since childhood. After giving birth about 10 years before the incidence described here, she had gradually increased in weight – from 130 to 155 kg, corresponding to a BMI (body-mass index) of 55 kg/m². She had sleep apnoea and periodic low back pain, but worked full time. Various conservative measures had not resulted in enduring weight loss, and she wished to undergo bariatric surgery.
The prevalence of overweight and obesity is increasing in Norway. Morbid overweight is defined as BMI > 40 kg/m2 or > 35 kg/m2 concomitant with serious weight-related disease. Patients with morbid obesity are prone to weight-related diseases, and may have a reduced life expectancy. For some of these patients, weight-reducing surgery may be appropriate. Norwegian hospitals carried out about 1 000 bariatric surgical procedures in 2007. Most patients are women and many are of fertile age (1).
The obesity team at Nordlandssykehuset Bodø recommended biliopancreatic diversion with duodenal switch and construction of a common channel of 100 cm. Open surgery was used. No complications occurred during the operation or in the postoperative period; the patient was discharged after five days and was prescribed oral supplementation, i.e. a multivitamin formulation containing 1 RDA (recommended dietary allowance) of vitamins and minerals; chewing tablets containing 500 mg calcium carbonate and 10 µg vitamin D₃ (Calcigran Forte; Nycomed Pharma, Asker, Norway; and a vitamin D supplement containing 30 000 IE of vitamin D₂ (AFI-D₂ Forte; Nycomed Pharma); and B-vitamin injections. Before the operation the woman was informed that weight loss may enhance fertility and that pregnancy should be avoided during at least the first year after the operation.
Two main surgical approaches have been used in Norway since 2004. Gastric bypass is used most often. Biliopancreatic diversion with duodenal switch is used for some of the heaviest patients and probably causes a greater weight loss. In this operation the first step is a partial longitudinal gastrectomy which decreases the stomach volume. The small intestine is thereafter divided and recoupled so that two separate intestinal limbs emerge (one for food, and one for bile and pancreatic juices); these two limbs are then coupled together creating a common channel of 50 – 100 cm proximal to the coecum (1). The operation decreases absorption of fat and starch and patients may also have increased satiety. The extent of malabsorption is determined by the length of the common channel. Metabolic complications may emerge after the intervention; e.g. vitamin and mineral deficiencies. Patients are therefore prescribed various nutritional supplements. Lifelong follow-up is recommended (1, 2).
The patient lost 17 kg before the operation and 10 kg the first 4 weeks after the operation (fig 1). She had previously had regular menstruation. She had a spontaneous abortion 5 years ago and had been wanting a child since then. She did not use regular contraception, and became pregnant 2 months after the operation. Folic acid (1 mg) was added to the other vitamins and she was referred to the Women’s Clinic.
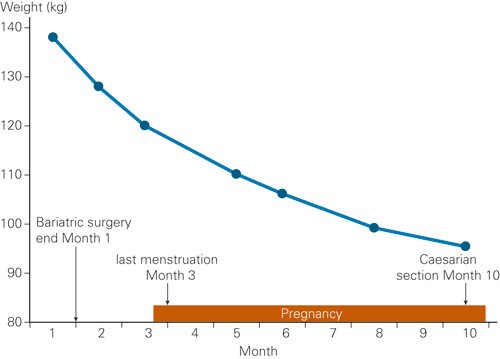
Figure 1 The patient’s weight development
The period with rapid weight loss after bariatric surgery is associated with a risk of nutritional disorder; it is therefore recommended to not become pregnant in that period. Depending on the type of intervention, the weight is usually stabilised after 12 – 18 months. Weight reduction seems to improve obesity-related infertility, possibly because polycystic ovary syndrome is more prevalent in women with a high BMI. Ovulatory dysfunction, insulin resistance and hyperandrogenism may improve after bariatric surgery (3). Such operations may also possibly lead to impaired absorption of contraceptives (4).
Obesity and metabolic syndrome is associated with an increased prevalence of foetal abnormalities and complications related to pregnancy (5). There is an increased risk of a spontaneous abortion in the first trimester. Later in the pregnancy the risk increases for pregnancy-related diabetes, hypertension, preeclampsia and intrauterine foetal death (6). Macrosomy is also more prevalent. Children are more often delivered by caesarean section, with an inherent increased risk of complications related to anaesthesia and wounds.Vaginal deliveries are associated with a higher rate of complications as there is an inherent risk of stuck shoulders, uterine bleeding and perineal tears (6).
Outcome of births after bariatric surgery has not been extensively studied. However, several investigators have concluded that the total risk for mother and child is less than that associated with extremely obese mothers giving birth (7 – 11). Marceau and collaborators compared the outcome of 251 pregnancies after duodenal switch with 1 577 pregancies before such an operation (7). Fertility increased, but there was still a higher incidence of spontaneous abortion than in the normal population. The proportion of children large-for-gestational-age (LGA) decreased from 34.8 % to 7.7 %, while the proportion of children small-for-gestational-age (SGA) increased from 3.1 % to 9.6 %. Several authors believe that neither women who do not increase in weight during pregnancy or their children seem to be at higher risk, but that close follow-up is necessary to prevent potential deficiencies (9).
Anaemia may occur secondary to deficiencies in protein, iron, folic acid or vitamin B12. Night blindness as a consequence of vitamin A deficiency has been reported after malabsorptive interventions, and foetal eye abnormalities have also been described (12). In general, there is an increased risk of volvulus and herniation when uterus grows during pregnancy.
Our patient had gone through a relatively uncomplicated pregnancy about 10 years earlier. She was hospitalized for 5 days in Week 35 with suspected mild preeclampsia. At term, the child was delivered through an urgent caesearan section because of rupture of membrane and umbilical cord prolapse.The child weighed 3 400 g and was healthy.
An ultrasound examination at the Women’s Clinic showed a 13-week foetus with normal organ anatomy. The mother was in good shape. Upon the two following controls the foetus had not grown well, and weighed 15 % less than expected in gestational week 25 and 45 % below that expected in gestational week 29 (fig 2). CTG (cardiotocographic examination) and Doppler examination of the umbilical cord artery were normal. At the time, the woman had lost 43 kg since the operation. She was normotensive, but had proteinuria + 1 on two occasions.
Steroids were given to mature the foetus´ lungs. At a gestational length of 29.6 weeks, ultrasound showed a symmetrical growth deviation of 48 % below the expected weight, with an estimated foetal weight of 750 g. CTG examinations were done daily. Three days later the patient was hospitalized with mild epigrastric pain, proteinuria 1–2+ and blood pressure elevation to 130/100 mm Hg. A caesarian section was performed due to weight deviation and reduced foetal activity. During preoperative preparations the mother had an extreme headache with sensitivity to light; blood pressure rose to 220/120 mm Hg. An uncomplicated caesarean section was performed in spinal anaesthesia and a girl was born (Apgar scores 8–8–9). The mother was in good shape after the operation, but only produced 100 ml of discolored urine during 18 hours. The blood samples were in accordance with the HELLP syndrome (anaemia with haemolysis, increased levels of liver enzymes and low blood platelets): haemoglobin 10.9 g/100 ml, haptoglobin < 0.1 g/l, ALAT 309 U/l, thrombocytes 28 · 10⁹/l and albumin 20 g/l. The mother was stable in the emergency department the next day.
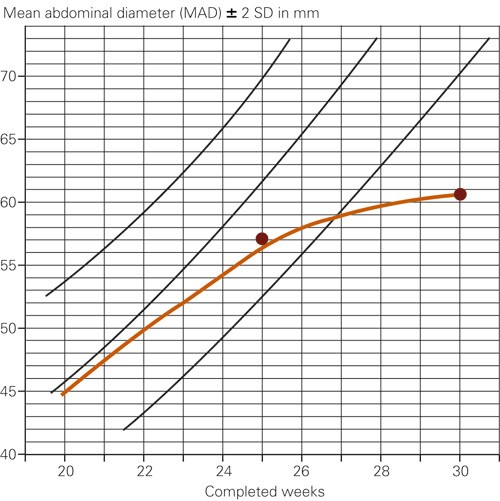
Figure 2 The foetus’ abdominal growth in relation to gestational age
The placenta was very small (weight below the 10-percentile) for the gestational length. Many areas showed insufficient trophoblast infiltration confined to the decidual part of the spiral arteries. The parenchyma showed diffuse ischemic changes with focal foetal inflammation and the umbilical cord had only two vessels.
The child weighed 2 100 g upon discharge from the paediatric ward, 8 weeks after birth. A small ventricular septal defect was not refound at the 7-month control, but physical examination raised suspicion of a slightly delayed motoric development. Mother’s milk substitute, multivitamin and iron supplement was recommended in the first year of life.
At control 15 months after the bariatric surgery, the mother’s weight loss was 65 kg – she then had a BMI of 26 kg/m². She had not taken all the supplements regularly and had a low level of ferritin (12 µg/l) and secondary hyperthyroidism. Bone density measurements were normal.
Discussion
At the end of pregnancy, the child weighed 50 % less than that expected for the gestational age, and the mother weighed 31 % less than before the bariatric surgery. The pregnancy occurred 8 weeks after the malabsorptive intervention, i.e. in the patient’s most catabolic phase. Weight retardation associated with insufficient placenta implantation and development of preeclampsia may be associated with the patient’s obesity at the time of conception, or the child may have been exposed to malnutrition for other reasons.
The expression «weight retardation» is used when a foetus has not reached its weight potential because of genetic or environmental factors. The risk for foetal death is dependant on the gestational length and degree of weight retardation (13). Our patient was followed closely throughout pregnancy, as duodenal switch may cause substantial weight loss the first year after the intervention. In some cases parenteral nutrition and reoperation may be necessary. One may ask whether it was advisable to undergo a pregnancy such a short time after the intervention. Available documention on this issue (7, 10) is not sufficient to advise termination of pregnancy.
In addition to standard vitamin supplementation after surgery, the patient was given extra supplementation of iron and folic acid, which is recommended to all women in the first trimester of pregnancy to prevent neural tube defect in the foetus. Iron is necessary, both for the foetal-placental development and for prevention of anaemia in mother and child. If the foetus is clearly hypoxic in utero; an ultasound examination will show reduced amnion fluid, blood flow changes will be detectable in various foetal vessels and a CTG-examination will show pathological changes. Blood flow was not measured in the uterine artery in our patient, but no other abnormalities were observed.
Hypoalbuminaemia, defined as serum-albumin < 36 g/l, most frequently occurs 6 – 18 months after a duodenal switch procedure (2). The reference range for albumin is about 10 % lower for pregnant women than for others, but nutritional deficiency may also be a cause of hypoalbuminaemia. In our patient the albumin concentration was 29 g/l in gestational week 26. This may be indicative of preeclampsia or protein deficiency.
Can preeclampsia be a cause for weight retardation? According to the Medical Birth Registry in Norway, preeclampsia before Week 34 was the cause of growth retardation in 22 % of children with a low birth weight (13). In preeclampsia, there is an insufficient trophoblast migration in the wall of the spiral arteries. This may damage the spiral arteries by reducing the diameter of the blood vessels, the blood flow and release of cytokines and free radicals. Local infarcts and reduced blood flow may cause deterioration of the foetal nutritional status. The risk is higher in mothers with previous preeclampsia, proteinuria, increased insulin secretion before pregnancy or high BMI at the time of conception.
The Medical Birth Registry reported the HELLP-syndrome in 1.8 of 1 000 pregnancies in Norway in 2006; about 15 – 20 % of the women did not have previous proteinuria or hypertension. The risk of multiorgan failure and death in mothers is decreased with rapid termination of pregnancy or labor within a short time (quick birth). Preeclampsia had not been confirmed before our patient developed the HELLP syndrome. Placenta findings indicate insufficient implantation. This is observed both in serious preeclampsia and weight retardation in the foetus. Hypoalbuminaemia may also be involved.
A number of professional groups were involved in treatment of the patient; i.e. general practitioner, surgeon, specialist in internal medicine, gynecologist, anaesthesist, paediatrician and midwife. Crossdisciplinary cooperation is a prerequisite for successful bariatric surgery. Routines differ between regions (according to telephone discussions with other treatment centres) and no guidelines are available for follow-up of pregnant women after bariatric surgery.
It has been suggested to limit the number of malabsorptive interventions in fertile women to reduce the risk of nutritional deficiency during pregnancy (11). Fertile women who undergo malabsorptive surgery should be recommended (in writing) to avoid pregnancy in the first 12 months after the operation and they should be informed that fertility may increase as a result of weight loss. Before the operation, they should also be advised about contraception. Hormone-releasing intrauterine devices may be favourable options; they reduce the amount of bleeding, are not associated with increased weight or an increased risk of venous thrombosis and their safety does not depend on the woman’s weight (14).
Patients who become pregnant should be referred to a gynecologist for ultrasound control. Foetal growth should be monitored monthly from week 22 in patients who become pregnant shortly after the operation and in patients who have undergone malabsorptive surgery. Serum albumin levels should be monitored regularly if the operation was performed less than one year before start of pregnancy. Additional iron and folate supplements are often necessary. Vitamin B12 supplements should be given after gastric bypass and fat-soluble vitamin levels should be monitored after malabsorptive interventions.