Systemic treatment, usually with tetracyclines, often in combination with local treatment, is necessary in moderate to severe acne. If this has no effect, especially with severe and scar-forming acne, the patient should be referred to a dermatologist for assessment of treatment with isotretinoin.
Acne vulgaris is a disease of the sebaceous glands caused by the micro-organism Propionibacterium acnes, hyperplasia of the sebaceous glands and overproduction of sebum (1). It affects 80 – 85 % of teenagers and usually disappears before the age of 25 years. The most severe cases are seen in boys aged 17 – 19 years. There is a connection between the degree of severity of the acne and poor self-image, anxiety and depression, leading in turn to absence from school and place of work. Successful treatment leads to a pronounced improvement in mental health (2).
This article deals with the treatment of moderate to severe acne vulgaris with special emphasis on systemic drugs.
Material and method
The article is based on a non-systematic literature search in PubMed. The articles were selected on the basis of the authors’ experience in the field.
Clinical findings
Moderate acne is characterised by a large number of inflammatory pustules. In more severe disease the patient has deep pustules, nodules, pseudocysts and cysts.
Acne conglobata is characterised by nodulocystic acne with communicating cysts and thick pus. Painful abscesses and pronounced scar formation may develop. In acne fulminans the patient develops ulcerations and necrotic acne with fever, reduced general condition, joint pain and leukocytosis.
Treatment principles
Combination treatment, where several aspects of the pathogenesis are attacked, is important for a successful result. Moderate and severe forms of acne are treated using systemic antibiotics, for example tetracyclines, often in combination with local keratolytic/antibacterial agents such as adapalene, benzoyl peroxide, clindamycin, or azelaic acid (Tab. 1). Patients who do not respond to treatment and/or develop scars or have psychosocial symptoms caused by acne should be evaluated with a view to systemic treatment with isotretinoin (3, 4).
|
Table 1 Treatment alternatives in moderate to severe acne
|
|
Papulopustular rash
|
Nodular lesions. Acne conglobata
|
|
First choice treatment
|
Systemic antibiotic combined with local retinoid treatment, possibly with supplementary benzoyl peroxide or azelaic acid.
|
High dose systemic antibiotic combined with local retinoid treatment and/or benzoyl peroxide
|
|
Other choice of treatment
|
Systemic isotretinoin
|
Systemic isotretinoin. In acne fulminans also prednisolon
|
|
Alternative for women
|
Systemic antiandrogens combined with local treatment with retinoid, azelaic acid and/or benzoyl peroxide
|
Systemic antiandrogens combined with local treatment with retinoid, clindamycin and/or benzoyl peroxide
|
|
Maintenance treatment
|
Local treatment with retinoid possibly combined with benzoyl peroxide
|
Local treatment with retinoid, possible combined with benzoyl peroxide
|
In acne conglobata it may be advisable to use intra-lesion cortisone treatment of selected lesions. In acne fulminans, systemic treatment with cortisone is necessary. Local retinoids, for example adapalene, can be used as maintenance therapy to prevent a flare-up after discontinuing systemic treatment (5).
Antibiotics
Tetracyclines inhibit bacterial protein synthesis by becoming incorporated in the secretion of the sebaceous glands; they inhibit bacterial lipases and prevent the breakdown of lipids to fatty acids, which trigger inflammation (Fig. 1). According to recent guidelines, systemic antibiotic treatment combined with local treatment is the first choice in moderate and severe acne.
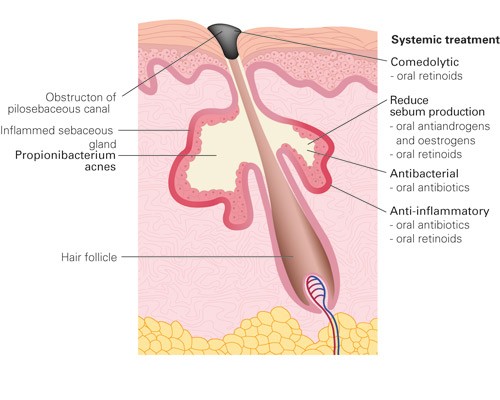
Figure 1 Anatomy of sebaceous gland and points of attack of various medicinal products
First generation tetracyclines such as tetracycline HCl and oxytetracycline are given in doses of 1 g daily divided into 2 doses. Second generation tetracyclines such as lymecycline 300 mg, doxycycline and minocycline 100 mg, are only given once daily. Minocycline is not registered in Norway. In more pronounced and widespread moderate acne, where low-dose tetracycline has not given a sufficient effect, higher doses of the drug should be used.
Second generation tetracyclines have a better pharmacokinetic profile and their absorption is not affected by intake of food and milk. A maximum treatment period of 3 – 4 months is recommended (5, 6), as the effect reaches a plateau after three months. Tetracycline should be combined with local treatment with retinoids and/or benzoyl peroxide, but not clindamycin solution, as this only gives a small additional benefit and increases the risk of development of resistance. There is no clinically relevant interaction between contraceptive pills and tetracyclines. Tetracycline should not be used concomitantly with systemic isotretinoin because of the risk of rise in intracranial pressure.
Erythromycin 500 mg twice daily may be tried as an alternative to tetracycline, although increased resistance to P. acnes has been described. Trimetoprim with or without sulphmetoxazole is not indicated in acne vulgaris, partly because of the risk of severe allergic reactions (6).
Isotretinoin
Isotretinoin, a vitamin A acid derivative, is effective in nodular, cystic and conglobate acne. Isotretinoin reduces sebum production and has keratolytic and antiinflammatory actions (Fig. 1). This treatment should only be started by a dermatologist or by a doctor who has good knowledge of the prescription regulations. The indication is severe acne that does not respond to systemic antibiotics in combination with local preparations. In nodulocystic, scar-forming and trunk acne, and in patients with pronounced psychosocial symptoms caused by the condition, this treatment should be considered earlier (4). The normal dose is 0.5 – 1 mg/kg/day, daily for four months, possibly longer. A cumulative dose of 120 – 150 mg/kg/course reduces the risk of recurrence. The effect of isotretinoin should not be evaluated until several months after completing treatment, as the improvement often continues after stopping treatment. The tablets are taken with food, because this gives the best absorption.
The most common side-effects of systemic isotretinoin are dry mucous membranes, nose bleed, and dry skin. Mental symptoms such as depression and mood changes have been reported, but it is not certain whether these are caused by the drug or by the skin disease. Several patients mention increased mental well-being after finishing treatment (7). Isotretinoin is teratogenic, so safe contraception is obligatory during the whole period of treatment and for a minimum of four weeks after stopping treatment.
Antiandrogen treatment
Contraceptive pills with cyproterone acetate ethinyl oestradiol and drospirenone ethinyl oestradiol have antiandrogenic properties, have an inhibitive effect on sebum production and can be used to treat acne in women (Fig. 1).
Spironolactone has previously been described as an effective drug in doses of 25 – 100 mg twice daily for a minimum of six months. In a new Cochrane overview, however, spironolactone has little effect in the treatment of acne (5), Antiandrogenic treatment is contraindicated in men.
Other treatment
In studies where a comparison is made between laser treatment, light therapy, and photodynamic treatment (PDT) of acne, the best effect of photodynamic treatment was found with inflammatory acne (5, 9). This gives reduced sebum production and inhibits the growth of P acnes. The treatment is painful. The optimal treatment procedure has not yet been clarified. There is no reason to recommend these methods at present.
Treatment of pregnant women
Systemic treatment with isotretinoin, contraceptive pills and tetracyclines is contraindicated during the whole pregnancy. From the second to the third trimester, systemic treatment with erythromycin can be used.
Acne scars
Acne scars may be hypertrophic or hypotrophic. Variations in inflammatory response and genetic predisposition seem to affect the development (10). Hypertrophic scars can be treated with intralesional corticosteroid injections, such as triamcinolone 10 – 40 mg several times. Hypotrophic acne scars should be treated during a quiescent phase, 12 – 24 months after stopping acne treatment. The alternatives are many, but not always good: dermabrasion, chemical peeling, surgical intervention, and laser treatment, including fractionated CO2 laser and YAG laser (3). These forms of treatment are carried out by some dermatologists and plastic surgeons.
Post-inflammatory hyperpigmentation is seen, particularly in those with a dark skin type, and may be present for up to 18 months, but then diminishes spontaneously.
Conclusion
Moderate and severe acne should primarily be treated with systemic antibiotics, such as tetracyclines, preferably in combination with local keratolytic and/or antibacterial agents. Patients with scar-forming or severe acne and those who experience a lack of effect with other treatment should be referred to a dermatologist with a view to systemic treatment with isotretinoin.